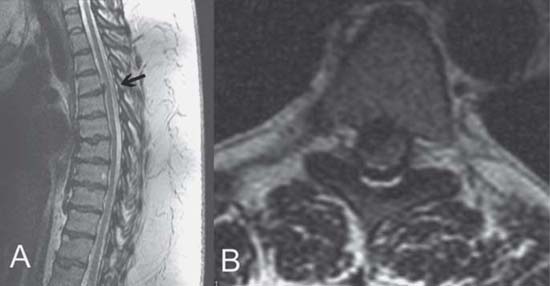
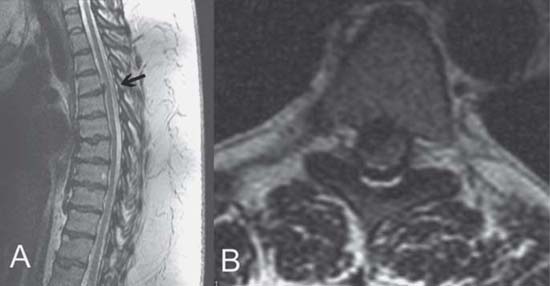
Case 92 Thoracic Disk Herniation Remi Nader Fig. 92.1 (A) Sagittal and (B) axial T2- weighted magnetic resonance images of the thoracic spine showing herniated disk (arrow) at the T4–T5 level. Magnetic resonance imaging of the cervical spine is read as normal by the radiologist. You then decide to obtain an MRI of the thoracic and lumbar spine. The thoracic spine MRI is shown in Fig. 92.1. The lumbar MRI is read as normal.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
92 Thoracic Disk Herniation
Case 92 Thoracic Disk Herniation Fig. 92.1 (A) Sagittal and (B) axial T2- weighted magnetic resonance images of the thoracic spine showing herniated disk (arrow) at the T4–T5 level.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


