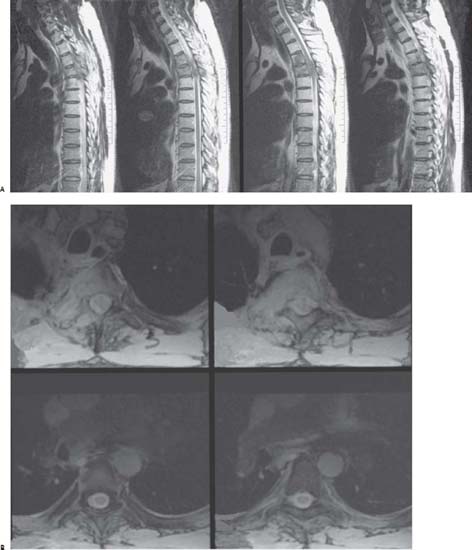
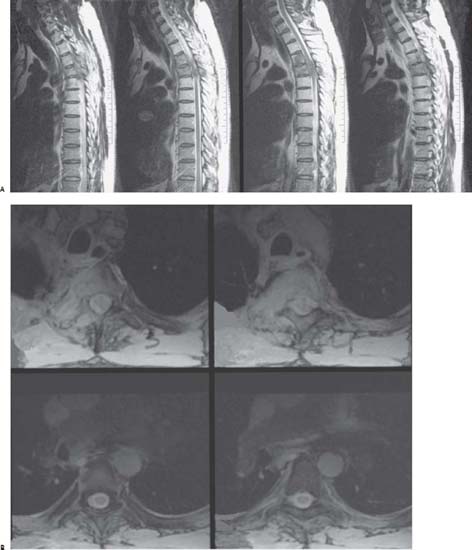
Case 95 Spinal Metastases Brian Seaman and Joseph A. Shehadi Fig. 95.1 (A) Thoracic spine sagittal T2-weighted and (B) axial T2-weighted magnetic resonance images through T3–T6: Upper two images — T3 and T4, lower two images — T5 and T6. Computed tomography (CT) of the chest, abdomen, and pelvis failed to reveal visceral metastasis. Bone scan and MRI of the spinal axis revealed the lesions at T3 and T4 to be isolated. Karnofsky performance status was 80 prior to his recent neurologic decline. The patient acutely underwent surgical intervention. The goals of surgery were to prevent neurologic decline, alleviate pain, stabilize the affected motion segments, and possibly restore lost neurologic function. Also, surgical intervention was a good option given that the vertebral and epidural metastases were from radioresistant NSCLC. The patient underwent single-stage transpedicular vertebrectomies at T3 and T4 with circumferential decompression and fixation. Anterior vertebral body reconstruction was completed with polymethylmethacrylate (PMMA). Posterior segmental instrumented fusion was completed via pedicle screws and rods from T1–T6 (Fig. 95.2). Local radiotherapy and systemic chemotherapy were initiated after the wound healed. The patient was ambulatory after treatment with significant pain relief. His survival was 6 months. Fig. 95.2 Postoperative anteroposterior thoracic x-ray.
 Clinical Presentation
Clinical Presentation
 strength in the right lower extremity (based on the Medical Research Council scoring system) and a sensory level at T4 to pinprick.
strength in the right lower extremity (based on the Medical Research Council scoring system) and a sensory level at T4 to pinprick.
 Questions
Questions

 Answers
Answers
95 Spinal Metastases
Case 95 Spinal Metastases Fig. 95.1 (A) Thoracic spine sagittal T2-weighted and (B) axial T2-weighted magnetic resonance images through T3–T6: Upper two images — T3 and T4, lower two images — T5 and T6. Fig. 95.2 Postoperative anteroposterior thoracic x-ray.
 Clinical Presentation
Clinical Presentation
 strength in the right lower extremity (based on the Medical Research Council scoring system) and a sensory level at T4 to pinprick.
strength in the right lower extremity (based on the Medical Research Council scoring system) and a sensory level at T4 to pinprick.
 Questions
Questions

 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


