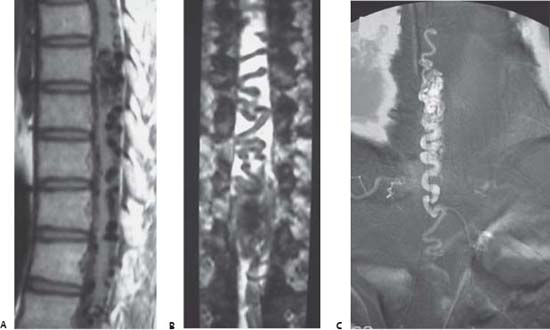
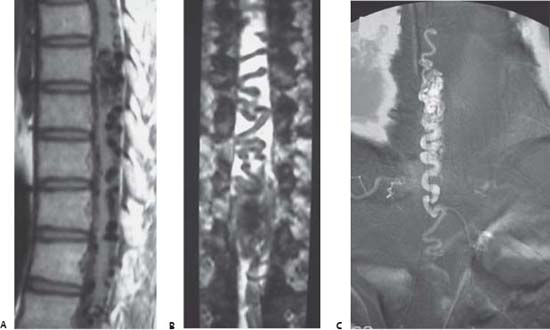
Case 96 Spinal Arteriovenous Malformation Bassem Sheikh Fig. 96.1 (A) T1-weighted and (B) myelographic magnetic resonance imaging, and (C) selective spinal digital subtraction angiography.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
96 Spinal Arteriovenous Malformation
Case 96 Spinal Arteriovenous Malformation Fig. 96.1 (A) T1-weighted and (B) myelographic magnetic resonance imaging, and (C) selective spinal digital subtraction angiography.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


