34
Accidents in Epilepsy
Introduction
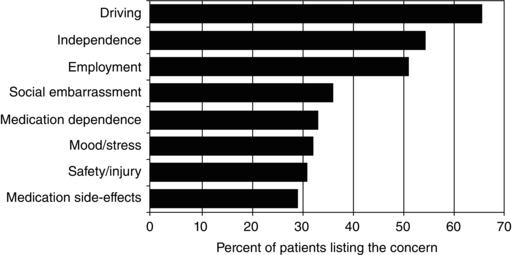
Individual seizures usually are not very dangerous, but their unpredictability makes them increase the risk for accidents and injuries. This risk for accidents is the major reason for the many restrictions and limitations placed on people with seizures, the basis of much of the disability associated with epilepsy, and the cause of some of the adverse psychosocial consequences of epilepsy. Therefore, it is important for healthcare providers to carefully consider how best to manage epilepsy patients to ensure that they are optimally protected but their life activities are not unnecessarily limited. Indeed, people with epilepsy themselves note that many activities limited by accident risk, such as driving and employment, are among their major concerns (Figure 34.1).
Epidemiology
Accidents are unexpected and unintended events leading to injury or death and are more common among individuals with epilepsy. Here we address nonfatal accidents and injuries, as Chapter 33 addresses mortality in epilepsy.
Comorbid conditions may increase risk for accidents and injuries in adults and children with epilepsy. Individuals with epilepsy have a higher incidence of cognitive and motor impairment that may predispose them to accidents. For example, those with posttraumatic epilepsy may be prone to additional accident and injury. Other factors influencing accident risk are sedating and cognitive side effects of antiepileptic medications.
Types of accidents and injuries
Burns
Individuals with epilepsy experience a higher rate of burn injuries. As many as 16% report suffering a seizure-related burn. Burns are more likely to occur with complex partial seizures as opposed to generalized tonic–clonic seizures, with scald and contact burns (e.g., from a bath or iron) being the more common types. In cultures where open fires are used for cooking, burns associated with seizures are a common presentation of epilepsy.
Figure 34.1. Concerns noted by patients with epilepsy. From Gilliam F, Kuzniecky R, Faught E, et al. Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia 1997; 38:233–236, with permission.
Falls and head injuries
It is reported that 45% of seizures are associated with a fall, which may then lead to head injury. The risk of head injury is higher with generalized tonic–clonic or myoclonic seizures. The most common seizure-related head injury is a concussion, accounting for 10% of injuries in people with epilepsy. Only a minority of head injuries are severe, causing intracranial bleeding or skull fracture.
Drowning
Seizures pose a clear risk when individuals are in or near water, and people with epilepsy have a substantially higher risk of submersion injuries and drowning. In one retrospective study, 14% of adults with epilepsy reported a seizure while bathing or swimming. Submersion is more likely to be fatal than other accidents in children and adults with epilepsy. Most submersions occur in the bathtub or swimming pool, with most deaths occurring when a person with epilepsy is not properly monitored.
Fractures
Fractures account for 11% of injuries in people with epilepsy. Although older antiepileptic medications such as phenytoin, carbamazepine, phenobarbital, valproate, and primidone can decrease bone mineral density, there are not enough data to conclude that the increased risk of fracture is associated with specific drugs.
Dental injury
Ten percent of people with epilepsy report a seizure-related dental injury. This is usually associated with falls and consists of losing teeth or fracturing the jaw.
Soft tissue injury
Contusions, wounds, and abrasions are the most common injuries seen with seizures. These soft tissue injuries account for as much as 25% of seizure-related injuries. A retrospective study of children showed that scalp and facial bruises were the most common seizure-related injuries.
Motor vehicle crashes
People with epilepsy have a nearly twofold increased risk for crashing, but that is for crashes of all causes, rather than just seizure-related ones. In fact, only 11% of all car crashes involving individuals with epilepsy are caused by seizures. Most result instead from the same cause of most crashes in the general population—namely, driver error. Studies of large populations confirm that the risk of crashing for individuals with epilepsy is not substantially higher than it is for other individuals who are not as strictly regulated, such as those with similar chronic medical conditions, including diabetes or hypertension, or certain higher-risk drivers, such as young males. Furthermore, the risk of motor vehicle crashes for individuals with epilepsy is far less than the risk of crashes related to alcohol. While a seizure during driving is dangerous, the risk of this happening is relatively limited and somewhat predictable, depending on how long an individual has been seizure-free.
Work injuries
Employment is a major concern for people with epilepsy. Surveys indicate that epilepsy is the medical disability viewed least favorably by prospective employers. Accident risk is a major consideration. Unemployment rates for people with epilepsy in the USA vary from 12% to 50%, depending on epilepsy type and associated medical, psychological, and social issues. Misconceptions about epilepsy contribute to these employment problems. Most people with epilepsy are actually capable of functioning at a high level, and accident and absence rates of workers with epilepsy are not higher than those of other employees. Current social and legal trends are combating discrimination against people with medical disabilities such as epilepsy to bring down barriers to employment.
Safety and prevention
Driving
Every US state permits those with controlled seizures to drive. The person with epilepsy is legally obligated to report his or her condition to the Department of Motor Vehicles. Physicians are required to report that a person has epilepsy only in a minority of states. Specific standards are available online (www.epilepsyfoundation.org). In general, states limit driving for those at greatest risk for seizures while driving. The standard for determining that risk is the duration of time a person with epilepsy has had no seizures, with the accepted period varying from 3 to 12 months, depending on individual US state rules. Emphasis on the seizure-free interval is widely supported, with a 3-month seizure-free interval recommended in a consenus statement from the American Academy of Neurology, the American Epilepsy Society, and the Epilepsy Foundation. Several favorable and unfavorable modifiers were proposed to modify the duration of the required seizure-free interval for driving with epilepsy (Table 34.1).
Table 34.1. AAN, AES, EF consensus on driving and epilepsy.
Source: Anonymous. Consensus statements, sample statutory provisions, and model regulations regarding driver licensing and epilepsy. American Academy of Neurology. American Epilepsy Society, Epilepsy Foundation of America. Epilepsia 1994; 35:696–705.
| General principles: |
|
Work
Most jobs are suitable for people with epilepsy. Most categorical prohibitions should be avoided and are usually not legal in the USA, although a small number of jobs require them (Table 34.2). When medical advice is sought regarding the suitability of particular jobs for people with epilepsy, the response should take into account the job requirements and that individual’s seizure history. For jobs with a high physical risk to the worker or others, the details of the work should be examined to reduce this danger to an acceptable level. Only when such risk reduction cannot be achieved are restrictions on the employment justified and potentially legal. The Americans with Disabilities Act (ADA) specifically prohibits exclusion of qualified people with epilepsy from employment opportunities unless they are actually unable to perform the job. Consequently, categorical prohibitions on employment of people with epilepsy in any capacity, previously widespread, are now illegal for most employers.
Table 34.2. Jobs and careers for which epilepsy-specific standards and rules or restrictions exist.
| Commercial driving (especially for interstate commerce) |
| Airplane pilots |
| Bus drivers |
| Military service |
| Law enforcement officers (varies by state) |
After someone with active seizures begins work, it may be advisable for that person to inform selected coworkers of the problem so that panic and other inappropriate responses to seizures are avoided. When seizures are likely in the workplace, education of coworkers and supervisors may help avoid or deal with misunderstandings. The Epilepsy Foundation has specific resources to help with employment and legal support.
Sports and recreation
Individuals with epilepsy should be able to participate in most types of sports. Yet some sports may require additional safety precautions. Organized sports are to be encouraged, and there is no evidence that contact sports worsen seizure frequency. Reasonable supervision is required for swimming, and additional safety measures may be considered for sports such as rock climbing, gymnastics, or horseback riding. Relatively few sports are discouraged in people with epilepsy. The list of discouraged sports includes such activities as sky diving, rock climbing without a harness, and scuba diving, because a seizure in those situations would be particularly dangerous.
Home
A person with epilepsy may modify the home to improve safety without sacrificing independence or privacy. To avoid burns, the microwave oven may be used preferentially over the stove. If the stove must be used, then the back burner is preferable. In the bathroom, while showers are safer than baths, one should ensure that drains work. In regard to burns and scalding, there are safety devices to control water temperature. Ladders and some power tools should be avoided by individuals at risk for seizures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


