INTRODUCTION
The rise in numbers of older people and the changing proportion of old to young people has been predicted for some time. It has become clear that the potential impact of this ageing phenomenon would have a major impact on population health profiles. Its potential impact on social and economic aspects of the more affluent countries highlights ageing as a sufficiently important issue in resource allocation. Discussion between the UK Department of Health, UK Medical Research Council (MRC), and experts from the scientific and medical communities late last century resulted in the decision that brain changes, most particularly cognitive decline, dementia and their relation to disability were key topics requiring investigation at the population level. This prompted a decision to invest in research into this area and a working group was convened, which included those with epidemiological and biostatistical expertise relevant to such investigation. Out of this working group a successful bid for the study now known as the MRC Cognitive Function and Ageing Study (CFAS) emerged1.
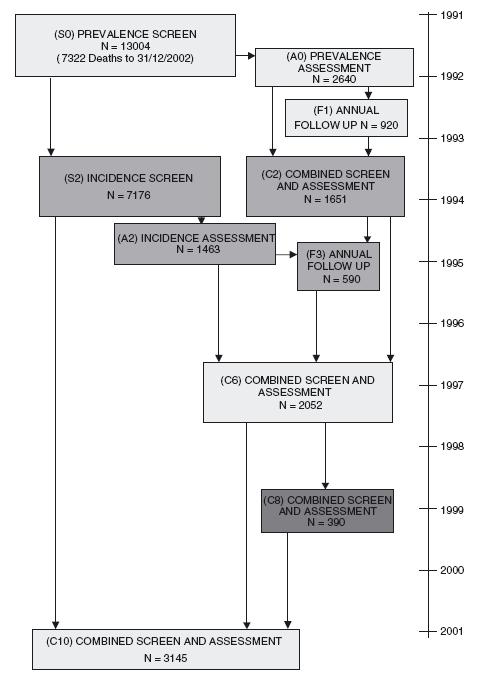
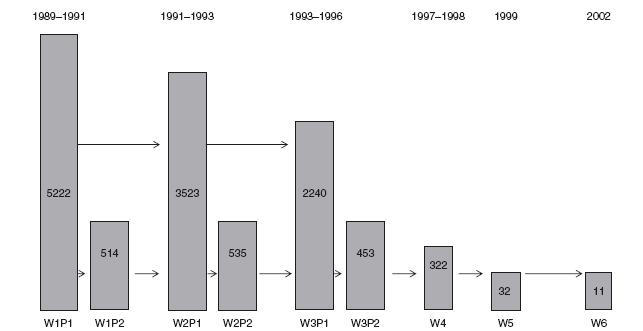
The study is a six-centre multidisciplinary multiphased longitudinal design. There are five identical sites and one with a different sampling and interview structure. This centre (Liverpool, also known as the ALPHA study, see Figure 39.1) was already funded at the time of the discussions noted above and thus started earlier than the other five centres2. The other five centres (Cambridgeshire, Gwynedd, Newcastle, Nottingham and Oxford) were able to follow a standardized design and are referred to as the five identical sites. Their basic structure was a two-phase design with a screening interview followed by an assessment interview shortly afterwards, with a repeat at two years. The fieldwork began in 1991 to 1993 (centre dependent)3 (see Figure 39.2 for flow diagram). Additional features are more fully described on the website (www.cfas.ac.uk).
In 2008 additional funding from the MRC enabled the introduction of a new cohort in three of the original CFAS centres (Cambridgeshire, Newcastle and Nottingham). Further funding from the Economic & Social Research Council (ESRC) in 2009 will enable a new cohort to be recruited to the Gwynedd centre (plus a new centre in Neath, Port Talbot) which focuses more on the social aspects of ageing.
The aims of the study (see Box 39.1) have evolved over its existence and cover a wide range including descriptive epidemiology, neuropathology, policy, molecular epidemiology and ethics. The principal neuropathological aim was to determine the contribution of different underlying pathologies to the rates of dementia and the geographical variation in these rates, and to the burden of disability.
Box 39.1 CFAS core aims
CFAS I core aims:
The main descriptive epidemiological aims include:
- the estimation of the prevalence and incidence of cognitive decline and dementia, and geographical variation in those rates;
- the determination of the natural history of dementia, in particular the rate of progression of cognitive decline including the distribution of the interval between the identification of cognitive impairment and death;
- the identification of factors associated with differing rates of cognitive decline and with the risk of dementia.
Additional aims included:
- to determine the prevalence and severity of pathological lesions in the brain of an unselected cohort of older people with and without cognitive impairment;
- to determine the frequency of specific pathological diagnoses in people with cognitive impairment;
- to correlate severity of specific pathologies with patterns of cognition, function and behaviour in life independently of clinical and pathological diagnostic categories. CFAS II core aims include:
- to update profiles of cognitive and physical function, physical and mental health and disability of people aged 65 or over in four of the original CFAS centres: Cambridgeshire, Gwynedd, Newcastle and Nottingham;
- to estimate the cohort change in prevalence and incidence of cognitive impairment and dementia;
- to investigate whether the measures that characterize the intermediate stage (mild cognitive impairment) best within the original CFAS are stable across generations;
- to quantify medication, health, social service use, social support, residential characteristics and care states, including formal and informal care, of people with dementia, frailty or physical disability across the three sites;
- to assess the contribution of different diseases, particularly dementia, to any change in the burden of disability over time, specifically whether diseases have become more or less disabling and estimate the effect of prevention vs. treatment;
- to compare the size of relationship of known genetic factors with frailty, including cognitive impairment, with those found in the earlier cohort;
- to provide a foundation for other collaborative studies that investigates biomarkers and further investigation of early markers, including imaging, for risk of cognitive decline.
The DNA resource was incorporated in a later phase of CFAS I. In CFAS II saliva is collected at baseline. The main molecular epidemiological aim has been to support genetics studies that have sought genes associated with dementia, Alzheimer’s disease, mixed and vascular dementia, cognitive impairment and decline. A later aim of the study was to explore the ethical and legal aspects of brain donation within a population-based sample given changing perception surrounding organ donation. The study also aimed to act as a core resource and provide a framework to support specific sub-studies in lone or joint centres. The Resource Implication Study 4-10 used this framework to achieve the core policy aim (see above).
Because the main study is focused on cognition and dementia it has collected the necessary dimensions of physical and mental health to arrive at a study diagnosis of dementia. It now has four major themes: (i) dementia (covering all aspects including cognition); (ii) depression; (iii) disability and healthy life expectancy; and (iv) health policy and health. In addition it has particular strengths in that it is one of
Figure 39.1 MRC Alpha Study: Liverpool centre design number of interviews
Source: Morris, J.C. (1993) The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology, 43, 2412-4
the very few truly population-based programmes with a brain donation programme – individuals in the study have indicated whether they wish to contribute to brain research through the donation of their brain after death (declaration of intention to donate).
Study Population
The first aim of the study was to estimate age-specific rates of prevalence of cognitive impairment and dementia among those aged 65 and over. The population is thus all those aged 65 years and over on the index date for centre (1990, 1991), living within a specified geographical location. Background information on the demographics of the populations sampled was collected from the Office of Population Censuses and Surveys (OPCS) 1990-91 census, now Office for National Statistics (ONS), to relate to regional and national data. Family Health Services Authority (FHSA) lists were used as the sampling frame. The frame would be incomplete if eligible members of the population were not registered with a GP. However, individuals in long-stay hospitals remain registered with their GP two years after institutionalization so sampling from FHSA lists ensured their inclusion. Each centre looked into the practices of long-stay hospitals in their area to confirm this. The FHSA list of individuals was used for sampling on a geographical basis. Each centre defined this area, and the study population was drawn from all those who were resident within it. Problems of inaccuracy, patients who died or moved away but were still on the FHSA list, were resolved by asking GP surgeries to check the lists. On this basis, a sample of sufficient size to yield 2500 interviews of individuals aged 65 years and over, stratified by age (equal numbers aged 65-74 and 75 plus) was chosen from the FHSA lists for each selected area (in Liverpool this was 5000 interviews stratified by sex and five-year age band). The population is flagged at ONS for mortality and the database is updated continuously. The follow-up has been determined by funding and the design of associated bolt-on studies.
The main follow-up waves for the identical sites are captured in the audit trail shown in Figure 39.2, which shows the numbers for the main screen, assessment, one-year follow-up and two-year rescreen, new selection for assessment and further one-year followup, six-year follow-up of the assessed (with venepuncture), eight-year follow-up of those with intentions to donate, and 10-year follow-up of the total sample. In addition to this the main associated studies are the Resource Implications Study (four centres – Cambridgeshire, Newcastle, Nottingham, Oxford), which followed those who provided care to the physically and cognitively frail at baseline4-10, the ESRC-funded Healthy Ageing Project, which interviewed in detail those who were not selected into the Resource Implications Study in Nottingham and Cambridgeshire11-16, the Network Study conducted in Gwynedd and Liverpool to examine individuals’ social networks, an embedded case-control study at two-year incidence stage (Cambridgeshire), and the ongoing brain donation programme in all centres. This programme, in combination with the bloods taken at year 6, form the major components of the biological resource of the study.
CFAS II will also have the same sampling frame and study size (at each centre). CFAS II is longitudinal at outset with two complete sweeps of the data planned. Each phase is two years apart.
Interview Method
All interviews were conducted in the respondent’s place of residence, using portable computers with customized software. If the interviewer felt that the respondent was frail and tiring, or becoming agitated, the short ‘priority mode’ set of questions could be invoked manually. Permission was also sought to access GP and hospital notes.
Content
CFAS I screening interview contains questions on residence, marital status, education and occupation, living circumstances, contact with friends and family, health and social care contact, self-reported physical health, instrumental activities of daily living and activities of daily living, cognitive measures (Mini Mental State Examination (MMSE) with augmentation) and medication. The assessment interview is mainly the Geriatric Mental State Examination (GMS) adapted for CFAS17-19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree