Chapter 7 Anatomy and Physiology of Congenital Spinal Lesions
Preoperative Considerations
In general, congenital spinal anomalies are sporadic, isolated cases.1,2 A wide variety of associated anomalies often accompany the spinal deformity and often need to be addressed prior to treatment of spinal lesions.3,4 In fact, the incidence of associated renal abnormalities is roughly 25% and that for cardiac abnormalities is 10%.5 Intraspinal anomalies, such as stenosis, diastematomyelia, and tethering of the spinal cord, may also occur (5–35%) in association with congenital spinal deformities.6–9 Therefore, before making treatment decisions, the entire bony vertebral column and spinal cord must be thoroughly analyzed using radiographs, CT, and MRI. Pulmonary function testing and/or arterial blood gases should be obtained when a thoracotomy is planned or when severe thoracic lordosis is present.
Craniovertebral Junction Abnormalities
Basilar Invagination
Basilar invagination results from a defect in the chondrocranium and is often associated with both skeletal and neural axis abnormalities.10–12 It results from deformation in all three parts of the occipital bone (basiocciput, exocciput, and squamous occipital bone).11 Two types of basilar invagination have been identified: ventral and paramedian.10–12 In ventral basilar invagination, the basiocciput is shortened and the associated platybasia raises the plane of the foramen magnum. In paramedian basilar invagination, the exoccipital bone is hypoplastic and the medial portion of the occipital bone is elevated. Clinically, the distinction is not important, and there is admixture between types. One should evaluate patients for an associated elevation of the floor of the posterior fossa that is most pronounced in the region of the foramen magnum. This anomaly may compromise the space available within the foramen magnum.13 Associated skeletal developmental anomalies found with basilar invagination include occipitalization of the atlas and Klippel-Feil syndrome in addition to neural axis abnormalities such as Chiari malformation, syringobulbia, syringomyelia, and hydrocephalus.11,12 Although the term basilar impression is often used synonymously with basilar invagination, this condition refers to an acquired form of basilar invagination caused by softening of the occipital bone, which occurs in conditions such as rheumatoid arthritis, Paget disease, hyperparathyroidism, achondroplasia, and osteogenesis imperfecta.14
Patients who are symptomatic from pure basilar invagination most commonly present with weakness and paresthesias in the limbs, whereas those patients with symptomatic Chiari malformations typically have cerebellar and vestibular complaints. Both groups may have evidence of lower cranial nerve dysfunction. Many patients do not develop symptoms until the second or third decade of life.15 This may be related to increasing instability from ligamentous laxity caused by aging, similar to that from delayed myelopathies reported after atlantoaxial dislocations.16 If chronic instability is present, granulation tissue may develop and act as a space-occupying mass in the ventral portion of the foramen magnum. Fibrous bands and dural adhesions are common in the dorsal cervicomedullary junction and around the cerebellar tonsils in basilar invagination.11 A high incidence of vertebral artery anomalies in basilar invagination has been reported (important for surgical planning), and symptoms of vertebral artery insufficiency can occur.12,17 Diagnosis of basilar impression (or invagination) is based on radiographic evaluation that demonstrates the altered relationship between the occipital bone and the upper cervical spine. Classically, this diagnosis is made by radiographic evaluation of the craniovertebral junction. A series of reference lines have been described to assist with this evaluation.12 MRI assists in delineating the relationship between the neural structures and the bony abnormalities; however, bony pathology should be evaluated with a thin-section CT.
Assimilation of the Atlas
Assimilation of the atlas represents a failure of segmentation between the atlas and the base of the skull. Embryologically, this entity represents a failure of segmentation between the fourth occipital and first spinal sclerotomes. This condition occurs in 0.25% of the population.10 The assimilation may be partial or complete and can involve the ventral arch of the atlas, the lateral masses, or the entire atlas. In many instances, assimilation of the atlas occurs with other spinal abnormalities, such as basilar invagination; Klippel-Feil syndrome; or Chiari malformation; as well as systemic congenital abnormalities such as cleft palate or urinary tract abnormalities.18 Patients with atlanto-occipital fusion often present with symptoms much like those for patients with classic Klippel-Feil syndrome, that is, restricted motion, short neck, low hairline, and torticollis.10 An increased incidence of atlantoaxial instability occurs with assimilation of the atlas, especially if there is failure of segmentation between the second and third vertebrae.11
The onset of symptoms in assimilation of the atlas generally occurs in the third and fourth decades of life. Dull headache and scalp tenderness in the distribution of the greater occipital nerve occurs frequently. Ventral compression of the brainstem from the odontoid processes is also a common finding. Weakness, spasticity, gait disturbances, or cranial nerve dysfunction can be associated problems.10 Neurologic symptoms have been related to the position of the odontoid process as an indication of the degree of actual or relative basilar impression. Vertical and horizontal nystagmus is related to cerebellum and tonsillar abnormalities. Decreased posterior column function from dorsal compression by the foramen magnum or a dural band is a less common finding. Symptoms may develop precipitously, but in the majority of cases the onset is gradual.
Atlantoaxial Instability
Atlantoaxial instability may result from aplasia or hypoplasia of the odontoid process, from laxity of the transverse ligament, or with assimilation of the atlas. Atlantoaxial instability is associated with Down syndrome, Klippel-Feil syndrome, numerous skeletal dysplasias, osteogenesis imperfecta, neurofibromatosis, and congenital scoliosis.19 The clinical significance of this condition is the potential for neurologic compromise, which can range from pain and dysesthesias in the distribution of the greater occipital nerve to tetraplegia or death.10,11 The articulation between the first and second cervical vertebrae is the most mobile segment in the vertebral column and is the least inherently stable. The odontoid process acts as a bony buttress that prevents hyperextension. However, the remainder of the normal range of motion is maintained and depends on the integrity of the ligamentous and capsular structures. Neurologic compromise can occur despite a normal odontoid process. With an attenuated or ruptured transverse atlantal ligament, a relative ventral shift of the atlas over the axis can result in spinal cord injury by impingement against the intact odontoid process such as occurs with atlantal assimilation.11,20 The risk is less if the odontoid process is absent, fractured, or moves with the axis during flexion, as occurs with most cases of os odontoideum.21 The stability of the atlantoaxial complex can often be determined using lateral radiographs. The atlantodental interval (ADI) is the distance between the dorsal edge of the ventral ring of the atlas and the ventral edge of the odontoid process. The normal ADI is less than 3 mm in adults and less than 4 mm in children.22,23 It has been suggested that an ADI greater than 3 mm in adults indicates a disruption of the transverse ligament. An ADI of 5 to 10 mm represents additional ligamentous damage, with total ligamentous disruption occurring in patients with an ADI greater than 10 mm.22 In congenital anomalies, such as hypoplasia of the odontoid process or os odontoideum, the space available for the cord (SAC) is often a better predictor of potential for neurologic compromise. The SAC is the distance from the ventral edge of the dorsal ring of the atlas or foramen magnum to the dorsal aspect of the odontoid process or the dorsal aspect of the axis. Greenberg suggested that in the adult, spinal cord compression always occurred when the SAC was 14 mm or less and never occurred if the SAC was 18 mm or more.24 In cases of os odontoideum, a SAC of 13 mm or less is associated with neurologic sequelae.25 In cases with persistent concerns about atlantoaxial stability, flexion-extension lateral radiographs can be performed. An awake patient should voluntarily perform the flexion-extension movements. MRI should be considered for any patient with a neurologic deficit before obtaining flexion-extension radiographs. MRI with flexion and extension views provides an excellent method of determining the potential for neural impingement with movement.
Anomalies of the Odontoid Process
Aplasia-Hypoplasia of the Dens
Aplasia-hypoplasia of the dens is a rare condition with a spectrum of presentations ranging from a hypoplastic rudimentary dens to complete absence of the dens. Usually, the rudimentary dens does not reach the upper edge of the ventral arch of the atlas, and an associated incompetence of the cruciate ligaments and alar ligaments results in atlantoaxial instability. Distinguishing aplasia or hypoplasia is of limited clinical importance because both conditions can lead to atlantoaxial instability and the treatment is identical. Vascular compromise from stretching and torsion of the vertebral arteries has been reported. Chronic atlantoaxial dislocation may provoke the formation of granulation tissue that can cause neurologic deficit because of constriction of the cervicomedullary junction.11 The presentation in children with atlantoaxial dislocation and congenital anomalies varies and includes syncope, torticollis, dysesthesia, and tetraplegia.
Os Odontoideum
Os odontoideum is an independent ossicle located rostral to the axis bone in the position of the odontoid process that is separated from a hypoplastic dens by a variable distance.26 The space between the os odontoideum and the remnant of the odontoid process is above the level of the superior facet of the axis. This leads to potential incompetence of the transverse ligament, which can lead to atlantoaxial instability.2 In children younger than 5 years, the normal epiphyseal line may be confused with the presence of an os odontoideum or a fracture. In os odontoideum, the free ossicle is rounded or oval, with a smooth cortical border. In the case of an odontoid fracture, the gap is usually narrow and irregular and often extends into the body of the axis at the level of the superior facet of the axis vertebra.2 The incidence of os odontoideum is increased in Down syndrome, spondyloepiphyseal dysplasia, Morquio syndrome, and after upper respiratory tract infections.26,27
There are two types of os odontoideum: orthotopic and dystopic. In the orthotopic variety, the ossicle lies in the location of the normal dens and moves with the axis body and the ventral arch of the atlas. This type is often associated with an intact cruciate ligament. In the dystopic variety, the os is located near the basion and is often fused to the clivus. The ventral arch of the atlas is hypertrophied, and the dorsal arch is hypoplastic. Dystopic os odontoideum has a greater likelihood of causing neurologic compromise than the orthotopic variety. This may occur because of dorsal compromise of the spinal cord by the ventrally located dorsal arch of the atlas during flexion and ventral compromise by the odontoid ossicle.26 Evaluation of atlantoaxial instability should be performed with flexion-extension films. In cases of chronic subluxation, dense granulation tissue may form, leading to an irreducible state. Os odontoideum has been ascribed to congenital, vascular, and traumatic causes.26 Trauma or infection during childhood is the most likely cause for the vast majority of cases of os odontoideum. Several cases have been reported in children with a normal odontoid process before trauma who subsequently developed os odontoideum. Many patients have a significant episode of trauma before the diagnosis of os odontoideum. After fracture or vascular compromise, a separation of the bone fragments occurs, probably because of contracture of the apical ligaments. The ossicle continues to receive a blood supply via the apical arcade, but the blood supply in the region of the fracture is disrupted, resulting in poor healing. It is probable that congenital forms of os odontoideum also exist. The congenital form results from failure of fusion of the portions of the dens derived from the proatlas and first cervical sclerotome. Dystopic os odontoideum is thought to be congenital in origin.
Disorders of the Subaxial Cervical Spine
Klippel-Feil Syndrome
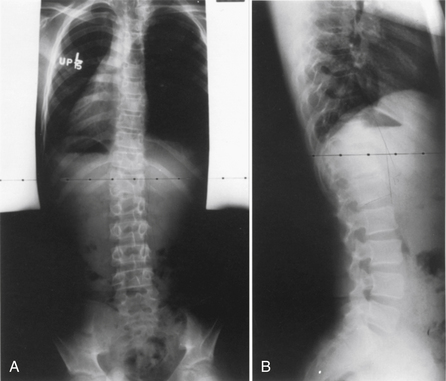
Klippel-Feil syndrome was first described as a case report with the clinical triad of a short neck, low dorsal hairline, and marked limitation of cervical range of motion resulting from a single unsegmented vertebral mass extending from the craniocervical junction through the fourth thoracic vertebra.28 Fewer than half of patients have all three signs. The most consistent finding is limitation of cervical motion.10 Currently, the term Klippel-Feil syndrome is used to describe any congenital fusion of the cervical spine with or without the clinical features of the original description (Fig. 7-1).
Often patients with Klippel-Feil syndrome have associated congenital abnormalities, which are often the conditions that prompt evaluation. The Klippel-Feil syndrome occurs in 25% of patients with congenital scoliosis.29 Therefore, all patients with congenital scoliosis should have radiographs of the entire spine to exclude the coexistence of the Klippel-Feil syndrome, and, conversely, all patients with a diagnosis of Klippel-Feil syndrome should have radiographs of the thoracic and lumbar spine. Approximately 50% of patients with congenital cervical or cervicothoracic scoliosis have associated Klippel-Feil anomalies. Renal anomalies occur in more than one third of patients. It has been suggested that routine screening ultrasonography be performed in all patients with Klippel-Feil syndrome.30
Sprengel deformity (an abnormal elevation of the scapula) occurs in 25% to 35% of cases of Klippel-Feil syndrome. It may be unilateral or bilateral.10 Other less commonly associated anomalies include deafness, synkinesis (involuntary paired movements of the hands and occasionally the arms), congenital heart disease, cervical ribs, ptosis, Duane syndrome (an abducens nerve palsy in which the adducted eye becomes retracted), lateral rectus palsy, facial nerve palsy, syndactyly, hypoplastic thumb, and upper extremity hypoplasia.
Symptoms related to the Klippel-Feil syndrome can be classified as mechanical or secondary to neural compression. Cervical instability and stenosis are potential problems in Klippel-Feil patients. The spinal cord area adjacent to the vertebral fusion may be compressed because of cervical instability, particularly at the occiput-C1 and C1-2 levels. All of these patients should have flexion-extension cervical spine radiographs. Neurologic deficits can range from radiculopathy to sudden death from minor trauma. Overall, 20% of patients who develop neurologic symptoms do so during the first 5 years of life and 65% by the age of 30 years.10 Neurologic symptoms detected during infancy are usually related to craniovertebral junction abnormalities. Children often have pain with atlantoaxial fusions. Subaxial cervical fusions often do not become problematic until the third decade or later, when degenerative changes begin to develop. Patients with short-segment fusions are less likely to develop symptoms, because of compensatory movement at uninvolved segments.
Iniencephaly
Iniencephaly is a disorder of the cervical spine consisting of congenital cervical synostoses, fixed retroflexion of the head, severe cervical lordosis, and varying degrees of deficits of the dorsal occiput and cervical vertebrae. This condition probably belongs to the spectrum of neural tube defects. The majority of fetuses with this condition are not viable.10 Parents of a child with iniencephaly have a 5% risk of having another child with a neural tube defect. Ultrasonography and serum or amniotic α-fetoprotein levels can be used to detect this condition in utero.31 Surviving patients are often handicapped by the cervical lordosis and hyperextension of the head. This posture makes it impossible to see straight without flexing the low back and hips.
Disorders of the Thoracolumbar Spine
Congenital Scoliosis
Congenital scoliosis is an abnormal curvature of the spine in the coronal plane that develops when anomalous vertebrae are present at birth. Congenital scoliosis is distinct from infantile idiopathic scoliosis, although both present with deformity during childhood. Infantile idiopathic scoliosis has no structural vertebral abnormality. Although vertebral abnormalities are present at birth in congenital scoliosis, the spinal deformity is rarely noticeable during infancy and usually presents during childhood or adolescence. Patients with mild or compensated deformities often receive diagnosis as adults when vertebral anomalies are discovered incidentally during routine radiographs. Congenital scoliosis can be associated with a variety of cardiac, genitourinary, and skeletal abnormalities.1,32 The spectrum of clinical presentations ranges widely based on number, location, and type of vertebral abnormalities. Certain vertebral anomalies result in rapidly progressive scoliosis during early childhood, resulting in severe morbidity, whereas other anomalies cause little or no deformity at any time.33 In general, 25% of congenital scolioses do not progress, 50% progress slowly, and 25% progress rapidly.33 Major advancements in the treatment of congenital scoliosis are improved imaging of the spine by CT and MRI, classification by type of vertebral anomaly, improved understanding of the natural history, and clarification of the indications and timing of surgery.
Advances in imaging have aided the diagnosis of associated neural axis abnormalities, such as occult spinal dysraphism and tethering of the spinal cord. Between 10% to 20% of all congenital scoliosis patients have some anomaly of the neural axis.8 Dorsal midline skin lesions (e.g., hairy patches or deep dimples), asymmetrical foot deformities (cavus or flat feet), muscle weakness, or spasticity all suggest underlying nervous system abnormalities. A thorough imaging evaluation is therefore indicated.
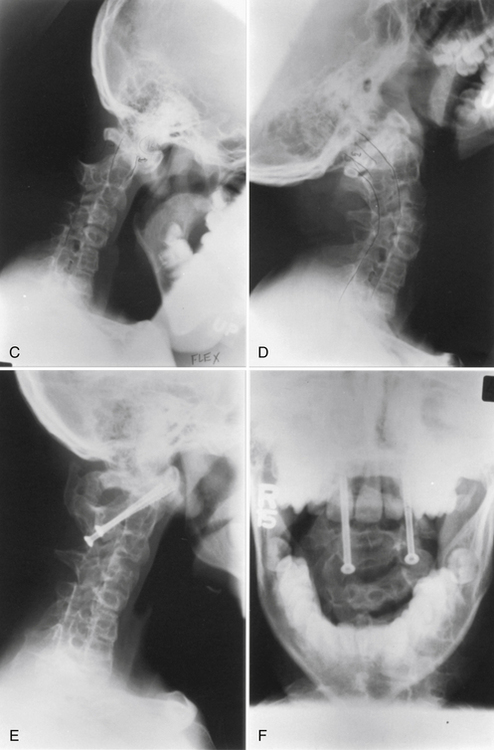
Usually, the vertebral abnormalities can be classified by the anomaly in the mesenchymal precursor that results in either a failure of formation or a failure of segmentation. Failure of formation results from a defect in the developmental process that produces an absence of part or all of the vertebrae. The defects range from mild wedging to total absence of the vertebra. A hemivertebra occurs with the complete absence of half of a vertebra and is one of the most common causes of congenital scoliosis. The hemivertebra consists of a wedged vertebral body with a single pedicle and hemilamina (Fig. 7-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree