Anterior Cervical Discectomy and Fusion (ACDF)
Kamran Majid
Jeffrey S. Fischgrund
Degeneration of the intervertebral disk is a normal function of aging, occurs in the majority of the population, and is frequently asymptomatic. Symptomatic disk degeneration can lead to axial pain, radiculopathy, or myelopathy. Intermittent axial neck pain frequently resolves after a short period of time and is rarely treated operatively. Cervical radiculopathy is also frequently treated successfully with nonoperative management, but the patient who remains symptomatic for a prolonged period of time may require surgical intervention. Surgical treatment options for cervical radiculopathy include anterior and posterior decompressive procedures. Cervical myelopathy is a graded process with variable clinical manifestations. Anatomic location of compression, ischemia, and dynamic factors also contribute to its spectrum. Myelopathic patients present with complaints of motor weakness, radicular symptoms, neck pain, hand clumsiness/dysfunction, gait disturbances, and bowel or bladder difficulties. The focus of this chapter is on anterior cervical discectomy and fusion (ACDF): indications, contraindications, evaluation, patient positioning, surgical techniques, postoperative management, clinical results, and complications.
SURGICAL INDICATIONS
There are several indications for an anterior cervical discectomy/corpectomy with fusion. In cases of trauma, it may be important to decompress the spinal canal after burst fractures. Other indications include tumor, infection, deformity, ossified posterior longitudinal ligament (OPLL), and spondylosis (1). Most patients with degenerative disease are initially managed nonoperatively. More expeditious surgical intervention is recommended in patients with severe myelopathy, rapidly evolving deficits, radiculopathy with persistent disabling pain and weakness (3 months), static deficits with significant pain, and/or progressive kyphosis.
CONTRAINDICATIONS
There are no specific contraindications to performing an ACDF. However, discectomy procedures should be considered when compression is limited to the disk level at one to two interspaces. In addition, posterior procedures should be considered in patients with predominantly posterior compression, multiple-level spondylosis or congenital stenosis, anterior bony ankylosis due to degenerative or inflammatory disease, developmental stenosis, prior anterior neck surgery or severe anterior soft tissue injury, continuous OPLL, and severe osteoporosis, which may increase the possibility of graft collapse
EVALUATION
Due to the high incidence of major abnormalities noted in the radiographic studies of asymptomatic patients, the history and physical examination are ultimately the most important diagnostic modalities. Neurologic involvements are defined by careful physical examination, with particular attention to sensory changes, motor deficits, reflex abnormalities, long tract signs, and gait and grasp difficulties. Deformity and overall bony architecture are defined by plain radiographs obtained in anteroposterior and lateral projections. The extent of spinal canal compromise and cord impingement is defined by myelography followed by computed tomography or magnetic resonance imaging (MRI). In all cases, clinical findings must be consistent with imaging before surgery is recommended. In clinical settings where the diagnosis is not clear, obtaining further neurophysiologic testing (i.e., electromyogram) may be helpful, both as a diagnostic exam and for later follow-up. Patients presented with radicular symptoms should be managed nonoperatively for at least 3 months with nonsteroidal anti-inflammatory drugs and physical therapy. However, those patients who are myelopathic with
unbearable pain, radiculopathy (motor deficit, worsening of symptoms), or instability should be counseled for earlier operative intervention.
unbearable pain, radiculopathy (motor deficit, worsening of symptoms), or instability should be counseled for earlier operative intervention.
PATIENT POSITIONING
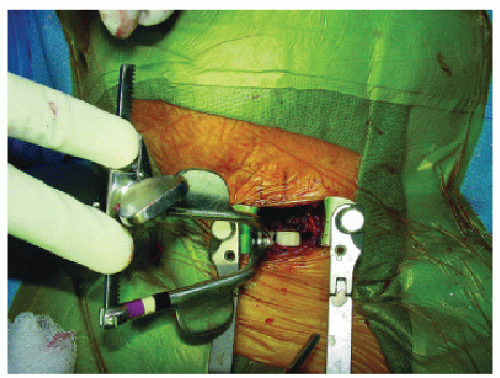
ACDF is performed with the patient under general anesthesia. Positioning of the patient is of extreme importance because proper positioning will enable the surgeon to perform the surgery in a safe fashion (see Fig. 74.1). Proper positioning of the endotracheal tube assists the surgeon especially in patients with herniations of upper cervical disks. If the surgeon chooses to perform the procedure on the left side of the patient’s neck, the tube should be taped to the right side of the patient’s mouth. A small rolled towel is then placed between the scapulae longitudinally to allow for slight hyperextension of the neck. This will assist in exposure of the cervical spine, but care should be taken when performing this maneuver if patients are myelopathic. Cervical myelopathy is often worsened with neck hyperextension, and this position should be avoided during the surgical positioning if the patient develops marked symptomatology while hyperextending the neck before the surgical procedure. The arms should be tucked along the patient’s sides, with traction being placed in a downward position on the shoulders with surgical tape. This downward retraction and securing of the shoulders helps with patient positioning and is extremely helpful for visualizing the lower cervical spine intraoperatively with radiographs, because the shoulders can often obscure the lower cervical spine when they are in the neutral position. It should be noted that there is a risk of brachial plexus injury, which has been reported in the literature.
PROCEDURE
Many spine surgeons perform this procedure on the left side of the neck to decrease the risk of injury to the recurrent laryngeal nerve. On the left side of the neck, the nerve predictably enters the thorax within the carotid sheath, then loops under the aortic arch, and ascends into the neck between the trachea and esophagus. Many authors have shown that the risk of injury to the recurrent laryngeal nerve can be decreased with this left-sided approach. Newer reports have disputed the anatomic basis for injury to the recurrent laryngeal nerve (2) and have hypothesized that retractor displacement of the larynx against the shaft of the endotracheal tube impinges on the intralaryngeal segment of the recurrent laryngeal nerve. It has been suggested that deflation of the endotracheal cuff can decrease the incidence of injury to the recurrent laryngeal nerve, thereby decreasing the incidence of postoperative voice changes.
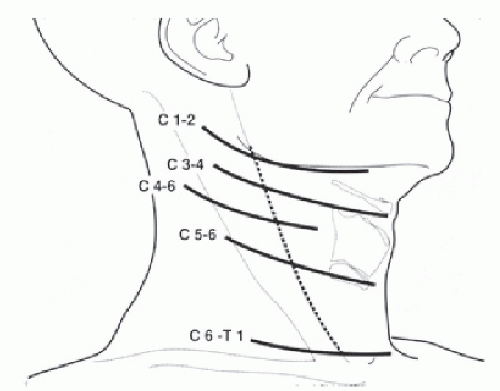
Transverse incisions are recommended for one- or twolevel discectomies and can occasionally be even used for more extensive procedures. Longitudinal incisions should be used for more extensive procedures such as multilevel corpectomies and may be beneficial in patients with short, thick necks. The incision should be placed using superficial landmarks to ensure that the dissection proceeds at the proper cervical level. Generally, the hyoid bone can be palpated at the level of C3; the thyroid cartilage is located at C4-C5, while the cricoid cartilage lies at the level of C6 (Fig. 74.2). The lower cervical spine (C7-T1) should be accessed through a longitudinal incision because the inferior thyroid vessels are frequently located at this level and can be managed more easily through the longitudinal approach. Exposure at this level does place the thoracic duct at risk on the left, and care should be taken to avoid the structure during the approach.
After the skin incision is complete, hemostasis can be obtained along the skin edges with electrocautery. The two edges of the skin can then be elevated with either handheld retractors or a small self-retaining retractor. The dissection then continues through the fascia until the platysma muscle is identified. The platysma muscle can then be incised in line with the original incision by placing a blunt, curved hemostat under the platysma muscle and then using electrocautery to incise the muscle. After the platysma muscle is incised, care should be taken to enlarge the approach along the fascial planes. The surgeon should not proceed with the dissection to the deeper planes using a limited exposure. Below the platysma muscle, the sternocleidomastoid is visualized laterally, and the approach can then proceed in a medial direction between the carotid sheath laterally and the trachea and esophagus
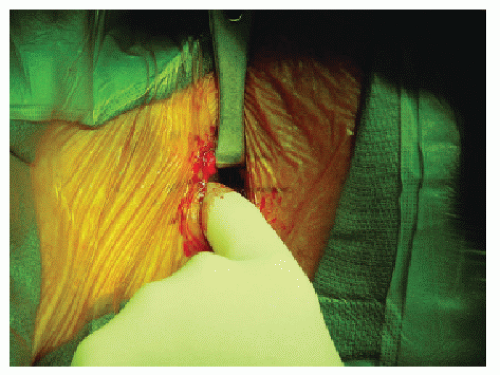
medially. This interval can usually be bluntly identified by manual palpation leading to the anterior vertebral bodies. The carotid artery can usually be palpated with the surgeon’s index finger, and although pulsations are occasionally not discernible, the contours of the carotid artery are easily felt (Fig. 74.3). Care should be taken not to compress the carotid artery for a prolonged period of time because this can lead to bradycardia, owing to compression of the carotid body. After the anterior vertebral body is palpated, retraction at this level is obtained with blunt handheld retractors because sharp edges can injure either the carotid vessels or the esophagus. Occasionally, the superior and/or inferior thyroid vessels arising from the carotid artery are observed crossing this interval and may need to be ligated if excessive tension is required to retract them during the procedure. With more extensive procedures, the omohyoid muscle is frequently visualized and may need to be divided to facilitate exposure to multiple levels of the lower cervical spine.
medially. This interval can usually be bluntly identified by manual palpation leading to the anterior vertebral bodies. The carotid artery can usually be palpated with the surgeon’s index finger, and although pulsations are occasionally not discernible, the contours of the carotid artery are easily felt (Fig. 74.3). Care should be taken not to compress the carotid artery for a prolonged period of time because this can lead to bradycardia, owing to compression of the carotid body. After the anterior vertebral body is palpated, retraction at this level is obtained with blunt handheld retractors because sharp edges can injure either the carotid vessels or the esophagus. Occasionally, the superior and/or inferior thyroid vessels arising from the carotid artery are observed crossing this interval and may need to be ligated if excessive tension is required to retract them during the procedure. With more extensive procedures, the omohyoid muscle is frequently visualized and may need to be divided to facilitate exposure to multiple levels of the lower cervical spine.
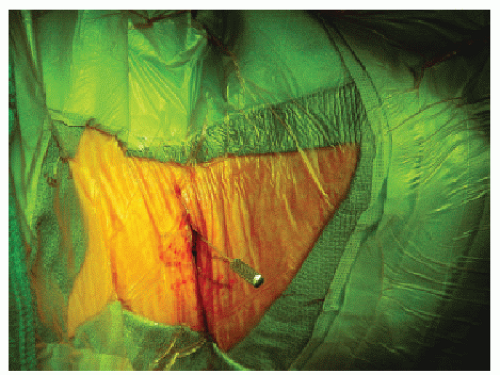
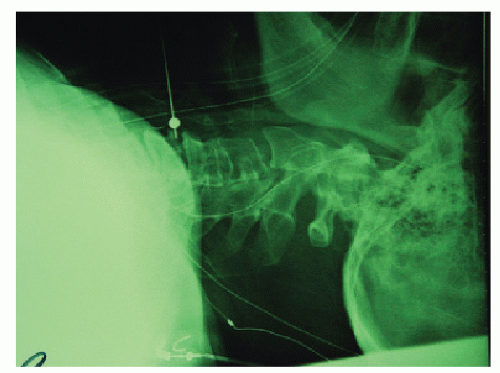
Palpation of the vertebral bodies can often lead to correct level identification. The preoperative films should be examined for anterior osteophytes, which are typically most prominent at the level needing surgical intervention. These can easily be palpated at the time of surgery to assist with correct level identification. In addition, Chassaignac’s tubercle can be palpated laterally at C6 and can aid in identifying the C5-C6 level. It is mandatory, however, that correct level identification be performed with an intraoperative radiograph. This is usually done by placing either a marker or a spinal needle in the disk space (Figs. 74.4 and 74.5). Nassr et al. (3), in a retrospective case series, concluded a threefold increase in developing adjacent-level disk degeneration in incorrectly marked disks after ACDF in the short term. This may indicate that either needle-related trauma or unnecessary surgical dissection contributes to accelerated adjacent segment degeneration. The surgeon should note, however, that if the exposure is in the lower cervical spine and the patient has either a short, thick neck or broad shoulders, it may be difficult to visualize the lower cervical spine radiographically. Therefore, the surgeon may elect to place a spinal needle at two levels, such that the superiormost needle can be visualized on the lower radiograph.
After the correct disk space is identified, the prevertebral fascia over the anterior vertebral body is divided, and the longus colli muscles are then easily visualized. The longus colli muscles are then elevated, bilaterally, with a combination of electrocautery and mild blunt dissection. Blunt self-retaining retractors can then be placed to maintain slight retraction of the longus colli.
With exposure complete, the anterior longitudinal ligament, which overlies the disk space, is incised with a No. 15 scalpel blade in a rectangular or box fashion. Through this opening, pituitary rongeurs can be used to remove the superficial portion of the intervertebral disk. After disk material can no longer be easily removed with the pituitary rongeur, small, straight, and angled curettes are used to remove the cartilaginous end plates and attached intervertebral disk. After approximately 50% of the disk has been removed, the disk space should then be distracted to facilitate removal of the posterior half of the intervertebral disk. Disk space distraction can be obtained through either intervertebral spreaders, or, alternatively, pins can be placed in the adjacent bodies and then specialized distractors are used to distract the disk space. With distraction, the remainder of the disk is removed with curettage of the cartilaginous end plates of the adjacent vertebral bodies. Occasionally, large overhanging anterior osteophytes off the superior body need to be removed with either a burr or rongeur to improve visualization of the posterior half of the disk space. It is imperative that the surgeon note the
angle of the disk space on the intraoperative localization film, and care should be taken to perform the disk removal along the angle of the end plates to avoid inadvertent penetration of the vertebral bodies.
angle of the disk space on the intraoperative localization film, and care should be taken to perform the disk removal along the angle of the end plates to avoid inadvertent penetration of the vertebral bodies.
When the discectomy is complete, along with complete removal of the cartilaginous end plates, the uncinate process, as well as posterior longitudinal ligament, is visualized. Although MRI is helpful for determining whether a sequestered disk fragment is present, visualization of the posterior longitudinal ligament is mandatory. If there is no preoperative suspicion of a sequestered fragment and the posterior longitudinal ligament appears intact, it is generally not recommended to remove the posterior longitudinal ligament. If, however, preoperative studies do indicate the possibility of a sequestered fragment or there is a tear in the posterior longitudinal ligament, the tear should be probed with a nerve hook and then a portion of the posterior longitudinal ligament should be removed with a micro-Kerrison rongeur to allow visualization of the dura and facilitate a search for free disk fragments. Removal of posterior osteophyte remains controversial and is not mandatory unless there is significant spinal cord or nerve root compression.
Once disk space removal is complete and the search for sequestered fragments has been completed, the disk space should be measured from an anterior to posterior direction using either a calibrated nerve hook or a small wire. Typically, the disk can accept a graft up to 10 mm in height (usually 5 to 8 mm), 10 to 15 mm wide, and 12 to 17 mm deep. The actual depth of the graft should be several millimeters less than the actual depth of the disk space to allow for slight recession of graft and avoidance of spinal cord compression (Fig. 74.6).
To facilitate bony union of the graft, bleeding bone should be obtained on the end plates. This can be accomplished by several means. A small, angled curette can be used to make several holes in the adjacent end plates, or, alternatively, the end plates may be partially removed with a burr. Care should be taken to avoid excessive bony end plate removal, because this can lead to structural incompetence and a collapse of the disk space on the graft.
Historically, iliac crest bone graft has been used with the anterior height 1 to 2 mm larger than the posterior height. This trapezoidal shape helps to avoid posterior retropulsion of the graft and also creates some lordosis. The disk space is then distracted again, either manually by the anesthesiologist or mechanically with various intervertebral distractors. The bone graft can then be placed in position and tamped with a mallet. If an anterior cervical plate is not a planned part of the procedure, the bone graft is usually countersunk 1 to 2 mm in relation to the anterior margin of the adjacent vertebral bodies to decrease the chance of graft extrusion, as well as esophageal compression. If the surgeon’s preference is to add an anterior cervical plate, then minimal countersinking of the graft is necessary. Before application of the plate, it is necessary to remove any anterior osteophytes that may not allow the plate to sit flush on the bone. A final lateral intraoperative radiograph should then be obtained to confirm correct graft placement, as well as hardware placement, if so indicated.
AUTOGRAFT VERSUS ALLOGRAFT VERSUS SYNTHETIC GRAFT
In recent years, the use of allograft for cervical spine fusion has become much more common. The use of allograft instead of autogenous bone for cervical fusion is acceptable if the fusion rates are equivalent and if the risk of disease transmission from the allogenic bone is minimized (4,5). Allograft obviously eliminates the necessity for a second surgical procedure to obtain the graft, thereby decreasing operative time, morbidity, and pain at the donor site.
Until recently, the most common type of allograft used was tricortical iliac crest harvested from cadaver iliac crest, similar in fashion to autogenous bone. In an effort to decrease the incidence of collapse rate, several surgeons have advocated the use of graft with superior structural properties such as fibula shaft and patella (6, 7 and 8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree