1 Approach to Nerve Conduction Studies and Electromyography
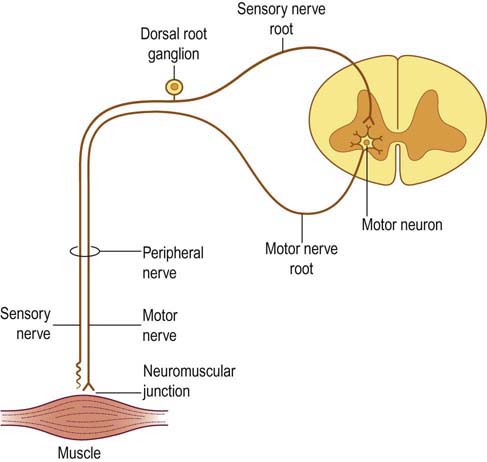
NCSs and EMG are most often used to diagnose disorders of the peripheral nervous system (Figure 1–1, Box 1–1). These include disorders affecting the primary motor neurons (anterior horn cells), primary sensory neurons (dorsal root ganglia), nerve roots, brachial and lumbosacral plexuses, peripheral nerves, neuromuscular junctions, and muscles. In addition, these studies may provide useful diagnostic information when the disorder arises in the central nervous system (e.g., tremor or upper motor neuron weakness). Occasionally, information from the EDX study is so specific that it suggests a precise etiology. In most cases, however, the exact etiology cannot be defined based on EDX studies alone.
Localization of the Disorder is the Major Aim of the Electrodiagnostic Study
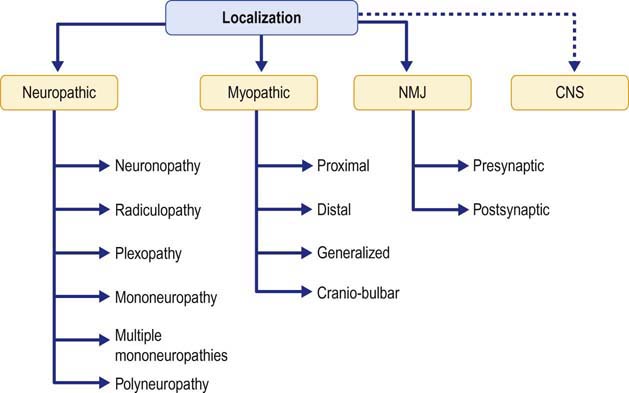
Once the localization is determined to be neuropathic, myopathic, a disorder of the NMJ or of the CNS, EDX studies can usually add other important pieces of information to localize the problem further (Figure 1–2). For instance, the differential diagnosis of a patient with weakness of the hand and numbness of the fourth and fifth fingers includes lesions affecting the ulnar nerve, lower brachial plexus, or C8-T1 nerve roots. If EDX studies demonstrate an ulnar neuropathy at the elbow, the differential diagnosis is limited to a few conditions, and further diagnostic studies can be directed in a more intelligent manner. In this situation, for instance, there is no need to obtain a magnetic resonance imaging scan of the cervical spine to assess a possible cervical radiculopathy because the EDX studies demonstrated an ulnar neuropathy at the elbow as the source of the patient’s symptoms.
Neuropathic Localization
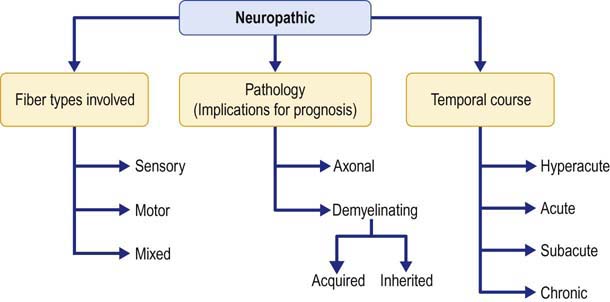
In the case of neuropathic lesions, EDX studies often yield further key information, including the fiber types involved, the underlying pathophysiology, and the temporal course of the disorder (Figure 1–3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree