FIGURE 12.1 The three-step test in a patient with a right fourth nerve palsy. Note the right hypertropia is greater on left gaze and with right head tilt.
Step 2. Record the magnitude of the deviation on gaze to either side. In a right fourth NP, the deviation is greater on left gaze, indicating that it must be due to a muscle that has its greatest action in that direction of gaze, either the right superior oblique or the left superior rectus.
Step 3. Compare the deviation with head tilt to either side. In a right fourth NP, the deviation is worse with right head tilt. A right head tilt demands an intorsion movement of the right eye, normally accomplished by the superior oblique and superior rectus muscles. The vertical actions of these two muscles normally cancel each other out but, in the face of a weak superior oblique, contraction of the unopposed superior rectus elevates the eye and worsens the misalignment.
G. Other examination features. It is important to look for orbital signs, which are sometimes subtle. These include proptosis, chemosis, conjunctival injection, and globe retraction with attempted eye movement, the latter best observed from the side. Careful inspection for pupil asymmetry or abnormal pupillary function is important, particularly in cases of a suspected mild or partial third NP. It is also helpful to look specifically for evidence of aberrant third nerve regeneration, which may accompany a slow-growing lesion causing a compressive third NP. Lid abnormalities may be helpful, including both retraction (usually indicative of thyroid eye disease) and ptosis (common in myasthenia, third NP, and oculosympathetic palsy). Von Graefe’s sign (retarded descent of the upper lid on downward movement of the eye) and lid lag (static higher than normal elevation of the upper lid in downgaze) may be seen with thyroid eye disease. Cogan’s lid twitch (twitch of the upper lid on return to primary gaze after prolonged downgaze) may be seen in myasthenia gravis. When eye movements appear limited with voluntary gaze, it is sometimes helpful to also test reflex movements, either with head turning (the vestibulo-ocular or “doll’s head” maneuver), Bell’s phenomenon (upward eye deviation with forced eyelid closure), or calorics.
LOCALIZATION AND ETIOLOGIES
Binocular diplopia can be caused by disorders of the extraocular muscles, neuromuscular junction, cranial nerves, brainstem, and orbit. In most cases, the pattern of ocular motor dysfunction and the presence of associated abnormalities allow accurate localization.
A. Brainstem. Disorders within the brainstem can cause abnormal eye movements by causing nuclear or fascicular cranial nerve palsies, INO, and skew deviation. Most lesions that involve supranuclear structures do not produce diplopia because reflex input keeps the eyes aligned. The main exceptions to this concept are disorders that affect vergence: divergence insufficiency causes esotropia at distance, and convergence paresis produces exotropia at near. Common causes of brainstem dysfunction are stroke, demyelinating disease, hemorrhage, inflammation, tumor, trauma, congenital anomalies, and certain metabolic derangements (e.g., Wernicke’s encephalopathy).
1. Nuclear lesions cause distinctive patterns of oculomotor dysfunction
a. Unilateral lesions of the oculomotor nucleus cause ipsilateral paresis of the extraocular muscles (EOMs) innervated by the third nerve, plus bilateral ptosis and loss of upgaze. The ipsilateral superior rectus subnucleus projects to the contralateral superior rectus causing loss of upgaze in both eyes. Because the levators are innervated by a single midline central caudal nucleus, a unilateral nuclear palsy causes bilateral ptosis.
b. The trochlear nucleus innervates the contralateral superior oblique muscle. Head trauma, midbrain tumors, and hydrocephalus may damage both fourth nerves because they decussate in the anterior medullary velum.
c. A lesion of the abducens nucleus produces an ipsilateral horizontal gaze palsy rather than a sixth NP because, in addition to motor neurons for abduction, the nucleus contains interneurons that supply the contralateral medial rectus subnucleus.
2. Fascicular lesions usually affect adjacent brainstem structures and can be localized accordingly. These syndromes are characterized by an ipsilateral ocular motor NP and a contralateral hemi-sensory or hemi-motor deficit and/or ipsilateral cerebellar dysfunction.
3. Damage to the medial longitudinal fasciculus produces a disconnection between the ipsilateral abducens nucleus and the contralateral medial rectus subnucleus, resulting in an INO. In addition to a variable degree of ipsilateral adduction deficit, there is slowing of medial rectus saccades and overshoot of contralateral abducting saccades with abduction nystagmus. Despite limitation of adduction, the eyes are usually aligned in primary position. In young patients, the most common etiology is demyelination and INO is commonly bilateral; in older individuals, the cause is most often stroke and lesions are more often unilateral.
4. Loss of otolith input causes vertical strabismus termed skew deviation. As otolith input changes with head position, the ocular misalignment of a skew deviation may improve with the patient in the supine position. Unlike misalignment due to a cranial NP, the muscle imbalance in skew is typically comitant, that is, the same in all directions of gaze.
B. Cranial nerves. Common causes of cranial neuropathy are ischemia, compression, meningitis (inflammatory or neoplastic), trauma, and congenital. The most common cause of an isolated ocular motor palsy in older adults is microvascular disease, termed a vasculopathic palsy. Most patients have one or more vascular risk factors (diabetes mellitus, hypertension, and hypercholesterolemia). Onset is acute, usually with ipsilateral pain, which resolves spontaneously within 7 to 10 days. Resolution of the motility disturbance takes place within 6 months.
1. Third (oculomotor) NP, when complete, causes loss of adduction, supraduction, and infraduction, profound ptosis, and a large, poorly reactive pupil. Unopposed action of the superior oblique and lateral rectus muscles causes a characteristic exotropic and hypotropic eye position. Partial forms are common, however, and recognizing the pattern of ocular misalignment is important (Fig. 12.2). One specific form of partial third NP affects only the superior division, resulting in ptosis plus isolated loss of upgaze. Because the pupillomotor fibers travel superficially in the third nerve, the pupil is usually affected early in a compressive third NP, particularly that is due to a posterior communicating artery (pCOM) aneurysm. In contrast, vasculopathic third NP typically spares the pupil (Video![]() 12.1). Thus, the presence of pupil sparing is often taken to “rule out” a pCOM aneurysm as the cause of a third NP. When a third NP is partial, however, pupil sparing is less reassuring because this pattern is occasionally seen with pCOM aneurysms. An otherwise complete but pupil-sparing third NP is never due to a pCOM aneurysm. Pupil sparing is also common in third NPs arising from lesions in the cavernous sinus.
12.1). Thus, the presence of pupil sparing is often taken to “rule out” a pCOM aneurysm as the cause of a third NP. When a third NP is partial, however, pupil sparing is less reassuring because this pattern is occasionally seen with pCOM aneurysms. An otherwise complete but pupil-sparing third NP is never due to a pCOM aneurysm. Pupil sparing is also common in third NPs arising from lesions in the cavernous sinus.
2. Fourth (trochlear) nerve palsies result in a limitation of infraduction when the eye is adducted. Patients report vertical and torsional diplopia. The most common cause is trauma, which frequently produces bilateral fourth NPs. Congenital fourth NPs are also common and may present at any age because of decompensation of fusion. A contralateral head tilt on old photographs may be a clue to a history of a congenital fourth NP. It is difficult to test fourth-nerve function in the presence of a third NP because the globe does not move to the position of advantage for the superior oblique muscle; instead the presence of intorsion on attempted downgaze is used to indicate preservation of fourth-nerve function (Video 12.1).
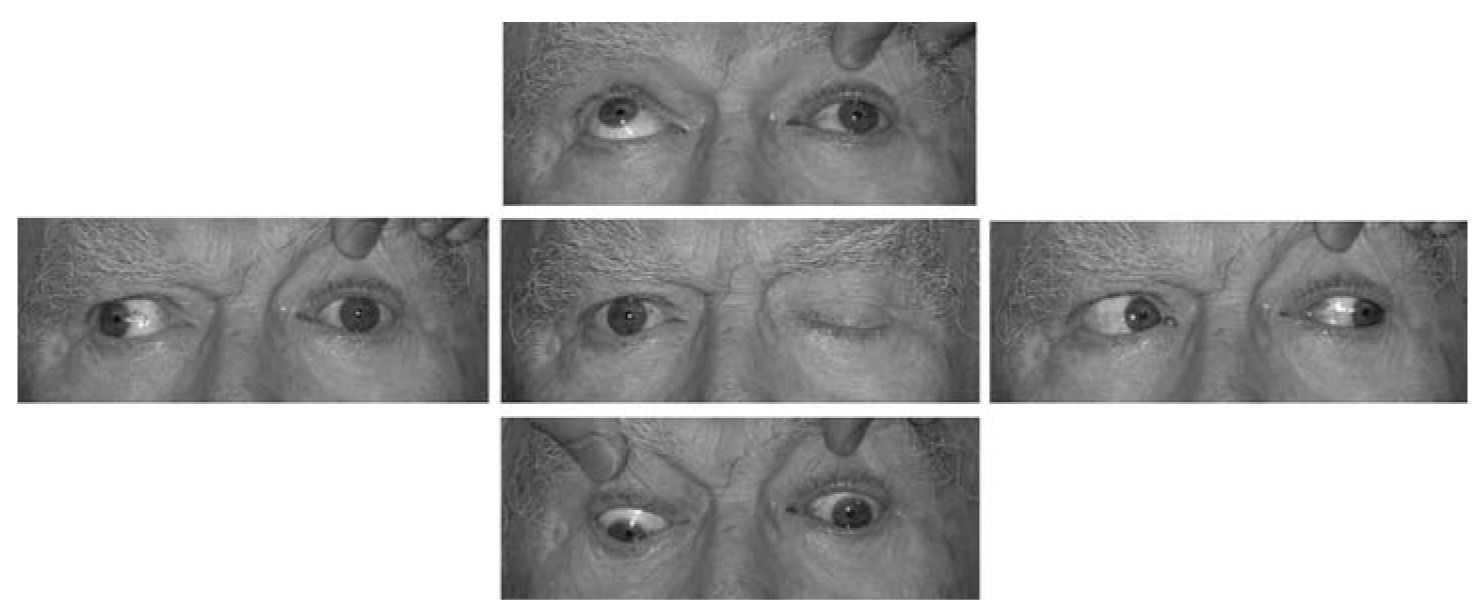
FIGURE 12.2 A 65-year-old man with a diabetic (vasculopathic) left third nerve palsy. There is loss of all third-nerve function with the exception of the pupil.
3. Sixth-nerve (abducens) palsy causes esotropia and loss of abduction with slowing of lateral rectus saccades (Fig. 12.3). In young adults, multiple sclerosis and tumors are important considerations; in older adults, vasculopathic cranial NP is most common. Chronic (greater than 6 months duration) sixth NP is often due to a compressive lesion at the skull base, such as a meningioma. Sixth NP can also be a “false localizing sign” of elevated ICP, caused by downward traction on the nerve.
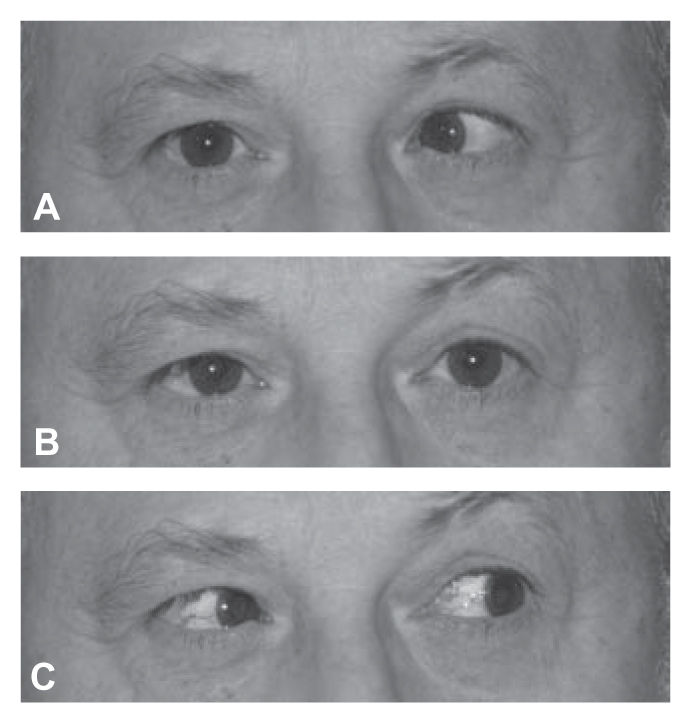
FIGURE 12.3 A 35-year-old man with acute onset of a right sixth nerve palsy secondary to multiple sclerosis. There is a moderate esotropia in primary position (B) that increases on right gaze (A).
4. Combined cranial NP involving the third, fourth, and sixth nerves localizes to the cavernous sinus or superior orbital fissure. The oculosympathetics and first division of the trigeminal nerve are commonly involved. Etiologies include tumor (primary and metastatic), vascular conditions (cavernous sinus thrombosis, fistula, and aneurysm), pituitary apoplexy, and infection/inflammation.
C. Extraocular muscles.
1. Neuromuscular junction disease is most commonly due to myasthenia, which causes painless, pupil-sparing, variable ptosis and diplopia. Other etiologies include paraneoplastic disease, botulism, and tick paralysis. Myasthenia is characterized by variability and prominent fatigability, often evident in the history and examination. Symptoms are typically absent upon awakening. Ptosis increases with prolonged upgaze and recovers after rest. Myasthenia may affect just a solitary muscle, several EOMs, or all muscles diffusely. Because of this enormous variability, the disease may mimic a number of different ocular motor conditions, such as cranial nerve palsies, gaze palsy, and INO. Weakness of eyelid closure as well as eyelid opening is a very helpful finding when present because the levators and the orbicularis oculi muscles are innervated by different cranial nerves (third and seventh, respectively).
2. Chronic progressive external ophthalmoplegia (CPEO) represents a group of hereditary disorders that causes limitation of eye movements with marked slowing of saccades and ptosis. Most are due to mitochondrial mutations, including Kearns-Sayre, which is sporadic and includes cardiac conduction abnormalities, atypical retinitis pigmentosa, and spongiform CNS changes. CPEO typically evolves over many years and is symmetric. It can be distinguished from myasthenia by its very slowly progressive and chronic course and by atrophy of extraocular muscles on orbital imaging.
3. Orbital myositis is occasionally due to a systemic granulomatous or vasculitic disorder but most commonly occurs as a form of idiopathic orbital inflammatory disease (orbital pseudotumor). Acute onset of diplopia is accompanied by pain with eye movement and the diagnosis can be confirmed on neuroimaging.
4. Graves’ ophthalmopathy causes restriction of eye movements due to inflammatory infiltrates, proliferation of fibroblasts, and edema. The inferior rectus is most commonly affected, producing loss of supraduction. The typical order of extraocular muscle involvement can be remembered by the mnemonic “IM SLO” for inferior rectus, medial rectus, superior rectus, lateral rectus, and obliques. Esotropia is more common than exotropia because frequent involvement of the medial rectus causes an abduction deficit, which can mimic a sixth NP (Fig. 12.4).
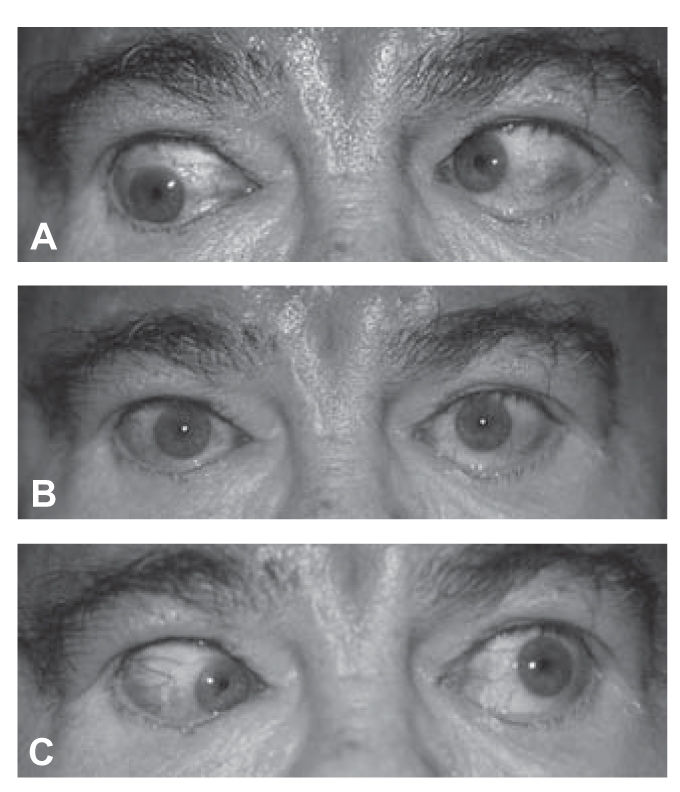
FIGURE 12.4 Esotropia and bilateral abduction deficit in a patient with thyroid eye disease. The presence of bilateral lid retraction and conjunctival injection are helpful signs indicating orbital restrictive disease rather than bilateral sixth nerve palsies.
5. Giant cell arteritis (GCA) is an important cause of diplopia in older individuals. Ischemia of extraocular muscles can produce a variety of patterns, sometimes mimicking a cranial NP. GCA can also cause diplopia as a result of ischemic injury to the third, fourth, or sixth cranial nerves.
6. Sagging eye syndrome (SES) is a non-neurologic cause of diplopia due to involutional changes in EOMs and orbital connective tissues. It can cause a small-angle distance esotropia (divergence insufficiency) accompanied by cyclovertical strabismus and often ptosis in elderly patients. SES is associated with excyclotropia in the hypotropic eye, whereas a fourth NP exhibits excyclotropia in the hypertropic eye.
D. Orbit.
1. Masses in the orbit may displace the globe, mechanically interfere with EOMs, or cause a cranial NP. Specific etiologies include primary or uncommonly metastatic tumors, vascular lesions, and inflammation including lesions of the adjacent paranasal sinuses. Pain, proptosis, chemosis, and conjunctival injection are common.
2. Lesions at the orbital apex cause a distinctive combination of ipsilateral optic neuropathy and ocular motor disturbance. Because structures are crowded at the back of the orbit, a relatively small lesion can produce severe dysfunction. Small lesions in this area may not be appreciated on neuroimaging, but the clinical findings should point to the correct localization.
3. Orbital trauma often causes fracture of delicate orbital bones. A blowout fracture of the orbital floor can cause entrapment of the inferior rectus muscle, producing a loss of supraduction. Fracture of the medial wall can entrap the medial rectus, which causes an abduction deficit that mimics a sixth NP.
EVALUATION
A. Clinical diagnosis. As is so often the case in neurology, the initial step in diagnosis is localization. It is often helpful to start by asking whether the pattern of ocular misalignment fits the pattern of a cranial NP. In the case of a third NP, it is important to be able to recognize ocular alignment patterns that indicate a partial third NP. However, isolated weakness of a single third-nerve muscle is exceedingly rare. Cases with this appearance more likely represent myasthenia, INO, or orbital restriction.
In cases in which the diplopia pattern is not consistent with a single cranial NP, pattern recognition is very helpful. For example, loss of supraduction when the eye is abducted is typical of inferior rectus restriction, such as from Grave’s disease or an orbital floor fracture. Limitation of eye movement accompanied by ipsilateral optic neuropathy constitutes the orbital apex syndrome. Any combination of third, fourth, and sixth nerve palsies points to a lesion in the cavernous sinus or superior orbital fissure; there is no other location where these nerves come together. Bilateral sixth NP indicates a lesion (tumor) of the clivus, meningitis (inflammatory or neoplastic), or increased ICP. Certain brainstem disorders create distinctive ocular motor deficit patterns. The one-and-a-half syndrome, for example, causes complete loss of horizontal eye movements in the ipsilateral eye and loss of adduction in the fellow eye, leaving only abduction away from the lesion (unilateral gaze palsy + INO). The combination of a third or sixth NP and contralateral long tract deficit is an example of a “crossed brainstem syndrome” and is highly localizing. In any patient with painless, pupil-sparing diplopia, the possibility of myasthenia should be considered.
B. Ancillary testing.
1. Blood tests. In all elderly patients with diplopia, giant cell arteritis should be considered. Testing includes complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Testing for acetylcholine receptor antibodies is appropriate if myasthenia is suspected, but antibodies are only positive in 50% to 80% of patients with ocular myasthenia. On the other hand, false-positive antibody testing is so rare that for practical purposes a positive result provides the diagnosis. Similarly, thyroid function tests may be normal in patients with thyroid orbitopathy (termed euthyroid Graves’ disease). Thyroid-stimulating immunoglobulins (TSIs) correlate with the activity and severity of Graves’ ophthalmopathy and can be tested by bioassay.
2. Radiographic testing should be directed to the area of interest determined from the clinical findings. Magnetic resonance imaging (MRI) generally provides more information than computed tomography (CT), especially at bone–soft tissue interfaces (skull base) and within the brainstem. However, if an orbital process is suspected, it is important to include dedicated fat-suppressed orbit views with gadolinium. The MRI “orbits” protocol at most institutions consists of coronal and axial thin sections with fat suppression. Alternatively, CT is an effective modality for imaging most orbital structures with the exception of the optic nerve. If optic neuritis is suspected, MRI is the study of choice.
3. The edrophonium chloride (Tensilon) test is often useful in patients with suspected myasthenia gravis. The ideal endpoint is an objective finding such as ptosis or a ductional deficit that resolves or substantially improves following injection. A small phoria or a subjective judgment by the patient is unreliable and should be avoided. False-negative results are not uncommon, but false positives are rare.
4. Single-fiber electromyography (EMG) is a highly sensitive test for ocular myasthenia gravis, but lacks specificity.
5. Ice test. Improvement of ptosis by at least 2 mm after placement of ice on the eyelids for 2 to 5 minutes constitutes a positive ice test for myasthenia. Similar improvement is sometimes seen in diplopia due to myasthenia. Alternatively, myasthenic ptosis often shows dramatic improvement following an interval of sleep or simple rest (eyes closed) for about 20 minutes.
URGENCY OF EVALUATION
In certain conditions, the clinical outcome depends on timely and appropriate treatment. Prompt recognition of these syndromes is thus crucial.
A. Aneurysmal third NP. Third NP due to a pCOM aneurysm usually presents with acute onset of ipsilateral pain and pupil involvement. Most pCOM aneurysms can be identified on a good-quality MR angiography (MRA) or CT angiography (CTA); however, even with high-quality imaging an aneurysm may still be missed. If there is high suspicion of an aneurysm on the basis of the clinical features, catheter angiography should be obtained despite a negative MRA or CTA. Features that strongly suggest an aneurysm include patients without vascular risk factors and those with a history suggestive of subarachnoid hemorrhage.
B. Pituitary apoplexy. Hemorrhage or infarction of a pituitary tumor usually causes acute onset of severe headache with signs and symptoms related to meningeal irritation. Visual loss, usually with a bitemporal pattern, and diplopia are common. Diplopia is most often due to third-nerve involvement, which may be unilateral or bilateral. In most cases of pituitary apoplexy, a pituitary tumor was not suspected prior to hemorrhage. The diagnosis is usually apparent on MRI, but can be more difficult to visualize with CT, which is often the imaging modality of choice for headache in an emergency department setting. Prompt diagnosis is crucial because of the potential for acute adrenal insufficiency and to improve the visual prognosis in patients with chiasmal compression. Emergency management should include systemic corticosteroids in stress dosages (e.g., hydrocortisone 100 mg IV every 6 to 8 hours) with careful monitoring of electrolyte balance. Surgical decompression is usually indicated, although occasional patients do well with conservative management.
C. Giant cell arteritis. In any elderly patient with diplopia, the possibility of GCA should be entertained. In addition to inquiring about typical symptoms, ESR, CRP, and CBC should be obtained. High-dose steroid treatment should be started upon suspicion of the diagnosis and temporal artery biopsy may be obtained thereafter.
TREATMENT
The treatment of diplopia is generally directed toward the underlying condition. Symptomatic treatment of double vision may include simple patching of one eye, which may be an acceptable solution in situations in which the underlying cause of double vision is expected to resolve imminently. In young children, the patch should be alternated to prevent the development of ambylopia; in adults, this is not a concern, and patients are usually most comfortable with the nondominant eye covered. An alternative to patching is to place translucent tape over one eyeglass lens, allowing some blurred vision, but not enough for double vision. A paste-on (Fresnel) prism can be helpful for diplopia that is expected to be temporary or change over time. A ground-in prism is generally preferred for long-term treatment. Patients may complain of excessive blurring, chromatic aberration, and weight of the prism for thick prisms required to correct large-angle ocular deviations. In situations in which the deviation is too large and/or incomitant to treat with prisms, eye muscle surgery may be undertaken after ocular alignment has been stable for a sufficient time period.
Key Points
• Monocular diplopia typically localizes to the ocular media and is very rarely neurologic in origin. Binocular diplopia that resolves with covering either eye is a hallmark of ocular misalignment.
• A complete third NP is characterized by an exotropia and hypotropia with ptosis, with or without pupillary dilation. A pCOM aneurysm can cause a complete pupil-involving or partial third NP. An otherwise complete but pupil-sparing third NP is never from a pCOM aneurysm.
• A fourth NP is characterized by ipsilateral hypertropia worsened with contraversive gaze and ipsilateral head tilt.
• A sixth NP is characterized by esotropia that is worse in the direction of gaze of the palsy.
• INO causes an ipsilateral adduction deficit and contralateral abducting nystagmus. Slowing of adducting saccades is the most sensitive clinical sign for INO.
• Ocular myasthenia gravis is seronegative in 50% to 80% of cases and should be considered with any pupil-sparing ocular misalignment.
• Cranial nerve palsies and supranuclear disorders cause slowing of saccades, while myasthenia and orbital restrictive processes do not.
• The primary treatments for double vision are occlusion of one eye, prisms, and eye muscle surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








