2. Pediatric guidelines for brain death were first published in 1987 and again revised in 2011 by the American Academy of Pediatrics (AAP) and the Child Neurology Society (CNS). The guidelines define the minimum standards that must be met in all clinical situations for brain death to be considered. There are three distinct differences in comparison to the adult guidelines that include apnea test requirements, number of examinations, and an observation period. The guidelines are as follows:
a. Exclusion of confounders
b. Established etiology of coma
c. Ascertain the futility of interventions
d. All clinical prerequisites are met
e. Test for the absence of motor responses
f. Test for absence of brainstem reflexes at all levels
g. Test for conclusive lack of respiratory drive
h. Confirmatory apnea test with Paco2 ≥60 mm Hg and Paco2 increase >20 mm Hg from normal baseline value
i. Two separate neurologic and apnea examinations performed by different qualified examiners
j. Interexaminer observation periods of:
(1) 24 hours for term newborns up to 30 days of age
(2) 12 hours for infants and children up to 18 years of age
B. Prerequisites. For each patient, the clinical assessment of brain death should be performed in an orderly and repetitive fashion. A step-by-step approach should be developed by the examiner that creates an unbiased and objectively confident diagnosis. With this approach, prior to examination, the clinician should define a set of prerequisites that rule out all medical and neurologic cofounders that mimic brain death.
1. Coma should be evaluated and assessed early on in the clinical course. Both etiology and irreversibility are key factors in determining the need for a brain death examination. A thorough review of the history, a complete neurologic examination, and adequate assessment of ancillary data are necessary. In approach to the patient, some period of time should be allowed to pass following acute presentation to exclude the possibility of recovery. Some conditions that may mimic brain death and reverse with appropriate management include hypothermia, drug intoxication, basilar artery occlusion, nonconvulsive status epilepticus, Guillain–Barré syndrome, and botulism. The etiology of acute presentations can be established with a variety of objective assessments including examination, neuroradiologic testing, and neurophysiologic testing. The concept of irreversibility is established not only with examination, but by the assurance that all necessary interventions for a given etiology have been performed. Such interventions can include ventriculostomy placement, hematoma evacuation, craniectomy, osmotic diuresis, and intoxication reversal. If these considerations have been met, then consideration of brain death may be necessary.
2. Neuroimaging should be performed and strictly evaluated with every patient suspected of brain death. Typical patterns with cause for concern include mass lesions with hemispheric shift, subdural hematoma with multiple parenchymatous contusions, diffuse subarachnoid hemorrhage, generalized loss of gray–white junction, and diffuse brain edema alone with effacement of the basal cisterns. In specific situations, such as early cardiac arrest, initial computed tomography scans may be normal. In such cases, repeat imaging should be performed to confirm or exclude the presence of advancing pathology. In cases of repeated normal neuroimaging, other confounders including intoxication and metabolic disturbance should be considered.
3. Pharmacologic interventions are a commonly overlooked confounder in the assessment of brain death. A detailed historical and objective examination into the history and administration of sedative, analgesic, and paralytic agents should be performed. It is recommended that all patients undergo a urine and plasma drug screen in addition to an adequate medication reconciliation. Examiners should consider the half-life clearance of all medications administered, and in situations of impaired renal and hepatic function, adjust appropriately. In patients who have undergone therapeutic hypothermia, metabolic clearance rates are slower and should be accounted for during examination. In patients who have received paralytic agents, confirmation of clearance with either facial nerve stimulation or the presence of muscle stretch reflexes is imperative.
4. Metabolic parameters should be adequately assessed in all patients prior to procession of the neurologic examination. Reversible metabolic conditions such as uremia, renal failure, hepatic failure, and hyponatremia should be worked up and treated. The presence of a severe acid–base disturbance may suggest an alternate underlying pathology. Metabolic acidosis is typically seen following drug intoxication. Respiratory acidosis may be seen following sedative and analgesic administration. Consideration of such factors and appropriate reversal should be considered. Finally, absence of all endocrine abnormalities, such as Hashimoto’s encephalopathy, should be confirmed to rule out such confounders that may mimic comatose or brain death states.
5. Physiologic parameters such as blood pressure and core temperature should also be considered in the assessment of brain death. In general, the diagnosis of brain death should never be made in an individual whose core temperature is <36°C. With every 1° drop in temperature, there is some decrease in brainstem responses, and at <20°C, all brainstem responses may be lost. In terms of blood pressure, it is recommended to achieve a baseline systolic blood pressure (SBP) of >100 mm Hg or an MAP >80 mm Hg. This can be achieved with either volume resuscitation or vasoactive medications. If overt arterial hypotension and shock are present, the brain death examination should not continue until all morbidities have been treated.
6. Respiratory analysis should be performed to ensure that no spontaneous respirations occur. The absence of physiologic respiratory patterns confirms suspected pontomedullary dysfunction and is necessary when testing apnea. In specific situations, including tidal volume mismatch, triggering of the ventilator may not be indicative of a breathing patient. If some form of ventilatory triggering is present, the examiner should consider further analysis using decreased sensitivity or a pressure support setting to confirm all absence.
C. Neurologic examination. Following confirmation that all prerequisites have been met and all confounders have been excluded, procession with the neurologic examination is warranted. The assessment of brain death should include a detailed evaluation of the following: pupillary response, corneal reflexes, oculocephalic reflexes, oculovestibular reflexes, facial movement, gag reflex, cough reflex, and motor responses.
1. Pupillary responses are the first examination technique in the assessment of brain death, measuring the integrity of the afferent limb of cranial nerve II and the efferent limb of cranial nerve III. The examiner should use a bright light in both eyes to determine the presence or absence of a pupillary response. The typical pupillary patterns associated with brain death are the midposition (4 mm) fixed pupils and dilated (6 mm) fixed pupils. Pupillary dilation, in some cases, is still present in brain death because of intact ascending cervical sympathetic input. With initial assessment prior pupillary trauma or surgery should be distinguished from history. Many drugs are known to influence pupillary size. However, such agents do not inhibit the total contraction or dilation of the ciliary muscle and with careful examination can be excluded.
2. Corneal reflexes assess the integrity of the afferent limb of cranial nerve V and the efferent limb of cranial nerve VII, to elicit a blink response. Such response requires a distinct interplay between cranial nerves and an intact brainstem is vital. The examiner should induce corneal stimulation by squirting water on the cornea or by stimulating with a cotton swab. Stimulation of this pathway should produce a bilateral blink response. Facial trauma and edema may preclude adequate examination. The complete absence of blink response is compatible with brain death.
3. Oculocephalic reflexes assess the functionality of cranial nerves III, IV, and VI. This technique, also referred to as the doll’s eyes technique, requires the examiner to initiate quick turning of the head from midposition to 90 degrees in either direction. Turning of the head should stimulate horizontal ocular movements. The examiner should also observe the eyes initially at rest with the lids open, assessing presence or absence of spontaneous ocular movements. The presence of forced deviation (vertical, horizontal, or skew) and nystagmus at rest would otherwise imply intact brainstem or cortical function. The absence of all ocular movements at rest and with motion is compatible with brain death.
4. Oculovestibular reflexes are used to assess the integrity of cranial nerves III, IV, VI, and VIII. In contrast to the oculocephalic reflex, the oculovestibular reflex requires the use of cold caloric testing with ice water. The examiner should elevate the patient’s head 30 degrees from supine position to ensure verticality of the horizontal canal. Next, a small suction catheter should be attached to the end of a 50-cc syringe filled with ice water and instilled into the patient’s auditory canal. Following injection, 1 minute should be allowed for observation of response, and 5 minutes should be given between examinations of either canal. Instillation of cold water into the tympanum induces an inhibition of the ipsilateral vestibular complex. In a comatose patient, a forced deviation of the eyes would ensue toward the cold stimulus. Certain pharmacologic agents including anticholinergics, tricyclic antidepressants, ototoxic antibiotics (aminoglycosides), and antiepileptics (phenytoin) may diminish such response, but are rarely relevant confounders. In brain death the oculovestibular response is completely absent.
5. Facial movements are a less common examination technique used in the assessment of brain death, but should be considered in all patients. Noxious stimulation should be performed with either deep nail bed pressure or bilateral condylar temperomandibular pressure. Stimulus in a comatose patient should cause activation of cranial nerve VII and elicit a grimace response. Supraorbital pressure may also be applied, stimulating both cranial nerve V and VII. The complete absence of facial grimacing following noxious stimulation is compatible with brain death.
6. Gag and cough reflexes are used to assess the functionality of cranial nerves IX and X. Determination of the gag and cough reflexes in an intubated patient can at times be difficult. The examiner should attempt stimulation by using bronchial suctioning. The catheter should be advanced completely through the endotracheal tube, followed by suctioning pressure for several seconds. In a comatose patient, a cough or gag reflex is typically initiated. Simultaneously, the clinician should also observe for physiologic responses to suctioning including tachycardia and change in respiratory rate. The complete absence of physiologic response and cough reflexes during bronchial suctioning is consistent with brain death.
7. Motor responses are used to assess functionality of the cortical and brainstem pathways required for movement. The examiner should apply a noxious stimulus, such as deep nail bed pressure, sternal rubbing, or condylar temperomandibular pressure, to the patient. In brain death, noxious stimulation should produce no motor response at all. The presence of spinally mediated reflexes to noxious stimulus can be seen, but is not indicative of an intact brainstem. The spinal reflexes can include brief movements of the upper limbs, finger flexion, finger tremors, and arm elevation. Differentiation between normal motor responses and spinal reflexes can be difficult and requires much expertise. Typically repetitive stimulation will cause spinal reflexes to diminish and help the examiner define a response. Fasciculations may also be noted on examination, and are likely due to pathologic anterior horn cells. Plantar reflexes are typically absent in brain death, but may be seen with instances of triple flexion. The absence of all motor movements is consistent with brain death ![]() (Video 34.1).
(Video 34.1).
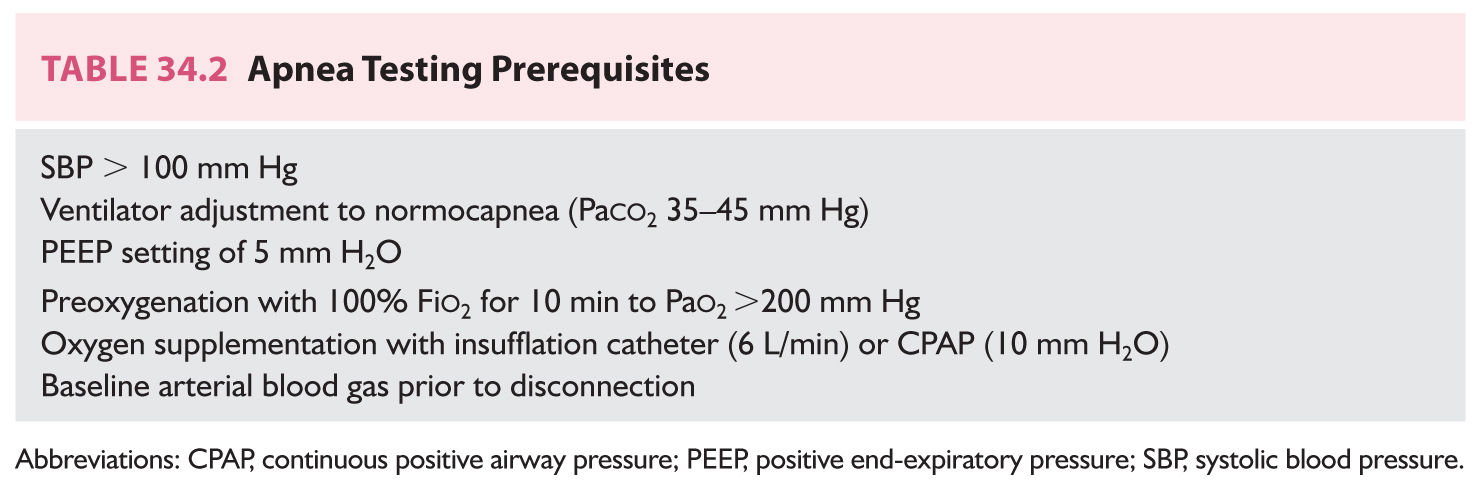
D. Apnea testing uses the mechanics of oxygen diffusion to assess ventilatory drive and is the most commonly used technique in the assessment of brain death. The apnea test itself, like that of the overall brain death assessment, requires a definable set of prerequisites be met to ensure that performance and interpretation of the test is adequate (Table 34.2). Prior to initiation, the patient must be hemodynamically stable with a SBP >100 mm Hg. The ventilator should then be adjusted to achieve normocapnea (Paco2 35 to 45 mm Hg) and a consistent positive end-expiratory pressure (PEEP) of 5 cm H2O should be initiated. The patient is then preoxygenated with 100% Fio2 to a goal of Pao2 >200 mm Hg to ensure adequate oxygenation. Once all prerequisites have been met, the ventilator is disconnected and an oxygen insufflation catheter is inserted. After 8 minutes, an arterial blood gas is drawn and the patient is reconnected to the ventilator. The defined criteria for determining brain death with the apnea test includes the absence of all spontaneous respirations, a Paco2 >60 mm Hg, or an increase in the baseline Paco2 >20 mm Hg.
In rare instances, complications may arise during the apnea test. The two most common complications include hypotension and hypoxemia. If the patient’s SBP drops below 70 mm Hg, the apnea test should be aborted and the patient should be reconnected to the ventilator. In general, cases of hypoxemia can be avoided by the use of a tracheal insufflation catheter to supply oxygen following disconnection from the ventilator. Cardiac arrhythmias, another concern, are very uncommon and can also be avoided with oxygen supplementation. If the examiner concludes that all criteria for the apnea test have been met, a diagnosis of brain death is confirmed. However, if the patient fails to meet all criteria, further investigation with ancillary testing should be considered.
E. Confirmatory tests. The use of confirmatory tests in the assessment of brain death is reserved for instances when the apnea test cannot be performed, the test itself was inconsistent, or the neurologic examination was unreliable. The current available confirmatory tests aim at the evaluation and interpretation of two distinct categories: cerebral blood flow and neuronal function. Confirmatory tests alone should never be used to diagnose brain death, but rather confirm findings from the neurologic examination. To date, only electroencephalography (EEG), transcranial Doppler (TCD), and cerebral scintigraphy have consensus statements regarding testing in brain death. The use of other ancillary studies including conventional cerebral angiography, and somatosensory evoked potentials (SSEPs) may be considered, but true evidence is lacking. It should also be noted that confirmatory testing may provide false-negative results with an otherwise convincing neurologic examination. The usual explanation in these cases is that testing was performed too early in the determination of brain death, and details that timing of ancillary testing is a crucial concept.
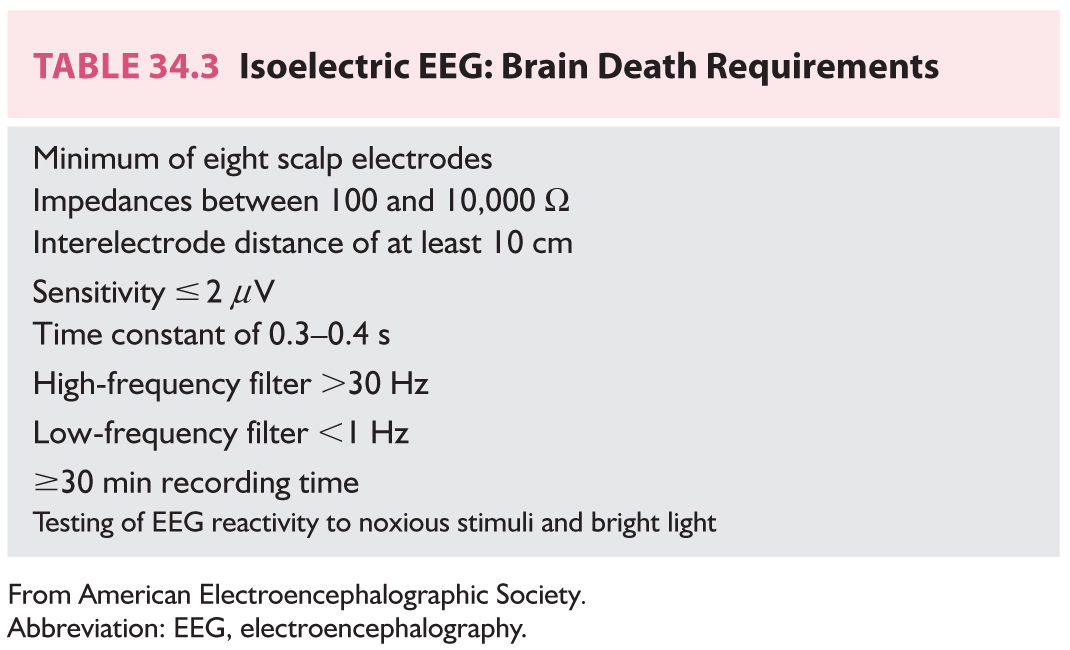
1. EEG is the most used ancillary test in the determination of brain death worldwide. Diffuse isoelectric activity is the EEG pattern consistently observed with brain death. Prior to interpretation of the EEG, consensus criteria must be met and consistent throughout the recording (Table 34.3). The overall sensitivity and specificity of EEG in brain death is 90%; however, limitations do exist. Confounders including electrical interference in the intensive care unit, posterior fossa lesions, and preserved subcortical function with ischemic cortex should all be considered. If all stated criteria are not met and a definitive isoelectric pattern is not observed, the EEG may not be considered valuable when assessing brain death.
2. TCD is used in brain death to identify and transmit signals from both middle cerebral arteries (MCAs) and is a validated ancillary test. The sensitivity and specificity are 91% to 99% and 100%, respectively. Performing the exam in the assessment of brain death requires the confirmation of intracranial circulatory arrest on two separate occasions at least 30 minutes apart. The typical pattern seen with cerebrovascular arrest is oscillating flow with early systolic peaks and a high pulsatility index. It should be noted, however, in normal population studies that sonography of the MCAs cannot be obtained in 10% of patients. This limits its use for definitive diagnosis in brain death. The major advantage of TCD is its portability; however, its major disadvantage is interpretive, relying on expertise of the sonographer and the clinician experience. All variables must be taken into account when TCD analysis is considered in the assessment of brain death.
3. Cerebral scintigraphy is a dynamic nuclear scan that utilizes radioisotope gamma monitoring to identify cerebral circulation patterns. The tracer isotope is injected into the patient 30 minutes before initiation of the scan. In clinical instances of brain death, the scan will display complete cerebrovascular circulatory arrest at the skull base. Comparison with the spleen or internal carotid arteries should be performed to assess the viability of intracranial tracer uptake. The specificity in brain death is 96%. In certain instances, small amounts of uptake may be seen in cortical venous or subcortical parenchymal structures, rendering the scan inconclusive. Nuclear scanning can also be difficult to obtain institutionally, and with its reported false-positive and false-negative rates, is not a preferred test in the assessment of brain death.
4. Conventional digital subtraction cerebral angiography (DSA) is a dynamic vascular study utilizing contrast injection to visualize the anterior and posterior circulation. In healthy individuals, filling follows normal anatomic and physiologic variables, with internal carotid artery (ICA) and intracranial filling first, followed by external carotid artery filling. In brain death, this normal filling pattern is reversed with extracranial filling occurring first, and arrest of ICA flow at the skull base. This reversal is due to the ICP gradient created at the base following brain death. Of note, DSA has also been shown to correlate quite well with cerebral scintigraphy. To date, no criteria for confirmation of brain death have been established by neuroradiologic societies, implying lack of standardization and perhaps limitation.
5. Electrophysiological studies used in brain death include SSEPs and brainstem auditory evoked potentials (BAEPs). Both studies utilize the generation of electric potentials to assess the functionality and connectivity of specific neural circuits. Several studies have evaluated the use of SSEPs and BAEPs in the assessment of brain death and have found very poor predictive values. With SSEPs, cortical responses are shown to be absent bilaterally in up to 20% of comatose patients. With BAEPs, patients with anoxic ischemic encephalopathy are shown to have absent wave forms, while wave forms are present in brain death. Although certain institutions recommend the use of electrophysiologic studies in brain death, they should truly be reserved for unique instances with otherwise inconsistent confirmatory tests.
ETHICAL CONSIDERATIONS
A. Legal background. Traditionally, the legal definition for death was defined as the complete cessation of all cardiopulmonary function. Early in the literature there was no mention of brain functionality as a definitive criterion. In 1981, the President’s Commission on Bioethics reinterpreted the definition of death as either irreversible cessation of cardiopulmonary function, or irreversible cessation of all brain functions. This Uniform Determination of Death Act was widely adopted by both medical and legal authorities in the United States. All states have also either adopted identical or similar legislation defining brain death as a mortal qualifier. These laws, given their correct use and interpretation, allow a clinician to cease all physiologic support when brain death is confirmed. There are, however, two qualifiers that continue to exist prohibiting termination of resuscitative care. These include preparedness for organ procurement and accommodation of specific family wishes. In three states (California, New Jersey, and New York), law currently protects all family wishes following a diagnosis of brain death, and they must be accommodated regardless of medical opinion.
B. Religious beliefs. Religion in the United States and throughout the modern world plays an integral part in the determination of brain death. Each major religion has long-standing traditions of defining death. Traditional language for most includes the cessation of the beating heart. Over time, however, general acceptance of brain death as a definition of death has been established. Both Christianity and Islam have held international summits that have come to the consensus that no brain function qualifies as death. In Judaism or Jewish Law, brain death is somewhat less defined and divided. Jewish Orthodoxy accounts only cardiopulmonary function as a qualifier, but less-conservative Judaism accepts brain death as a true entity. In general, the qualification of brain death is dependent on religious leaders and their acceptance of both the medical examination and objectivity used to determine diagnosis. In Buddhism, the prolongation of suffering is against standard practice, and brain death is widely accepted. The religious stance of organ procurement is a completely separate topic and again dependent on specific organizations. As an examiner, it is imperative that religious preference is known during the assessment of brain death to accommodate all parties involved.
C. Social background. Family and social support in the initial, intermediate, and late assessment of brain death is vital. Family-centered care and communication go a long way in understanding the diagnosis and willingness to accept death. Studies have shown that only half of families who have undergone an experience with brain death are able to define its criteria and show understanding of the process. Traditional cultural thinking defines the heart as the ultimate living being and the keeper of the soul. With its failure, then and only then is death imminent. A clinician must be able to approach these conflicting beliefs with care and compassion as well as clarity.
Ethnicity also plays an important role in communication and education in brain death. It is crucial to develop a multidisciplinary team approach for the care of the patient and the family that is sensitive to all beliefs and cultures. This will create a unique understanding and sense of respect with the family that may otherwise be lacking. Use of the clergy is also recommended as a safe go-between in the evaluation of brain death.
COMMON PRACTICAL PROBLEMS
A. Examiner qualification. To date, there are no specific studies detailing the accuracy of examination and diagnosis among different specialties. In the majority of tertiary care centers across the United States, the brain death examination is performed by either a neurologist, neurosurgeon, or a critical care physician. Other subspecialties likely participate in other institutions. Legally, all physicians in the United States are allowed to diagnose brain death. There are no adult guidelines recommending qualified examiners; however, the pediatric guidelines allow only for intensivists, neonatologists, trauma surgeons, neurologists, and neurosurgeons. Currently, there exists no standardized competency test to determine qualification. The most common portions of the examination left unchecked are the oculovestibular responses and the apnea test. Moving forward, two separate examinations may need to be considered in the adult population to ensure accurate diagnosis and qualification of examiners. Institutions may also consider implementation of standardized training and evaluation ensuring uniform certification. In general, most physicians do not feel comfortable with or have never performed the brain death examination. Further consideration should be made in the future to allow for only qualified interpretation in the assessment of brain death.
B. Primary brainstem lesion. Acute, destructive lesions to the brainstem can mimic brain death. In primary brainstem lesions, the cerebral hemispheres usually remain intact, precluding a diagnosis of brain death. Typical lesions that will cause catastrophic injury include basilar artery occlusion, pontine hemorrhage, compression from cerebellar hemorrhage, and direct brainstem trauma. In most common instances, a detailed neurologic examination will show some preservation of brainstem function. In most typical brainstem lesions, the medulla oblongata will be spared. The patient will have preserved respiratory drive and lack signs of autonomic failure. In instances when examination is concerning for brain death, patients will pass an apnea test. Ancillary studies such as EEG and intracranial vascular studies will show alpha coma pattern and preserved blood flow, respectively. Generally speaking, brain death examinations in patients with catastrophic brainstem injuries should be reserved for highly qualified clinicians.
C. Spinal reflexes are a polysynaptic, polysegmental reflex that can occur in brain death. Such reflexes are described as slow, short-duration movements that can be diminished by repetitive stimulation. Typical descriptions of such reflexes include triple flexion, finger jerks, head turning, abduction or adduction of the arms, and even attempts at sitting up. The frequency of movements in brain death varies, but has been reported as high as 39%. Review of spinal reflexes compared to complex motor movements has shown no correlation. Typical decerebrate and decorticate motor responses have no clinical correlation with spinally mediated responses, and are thus differentiated. The presence of spinal reflexes on examination does not preclude the diagnosis of brain death. Both experience and careful assessment will allow an examiner to reach a correct conclusion.
D. Difficulty with the apnea test. The final step in the confirmation of brain death is completion of the apnea test. There are several clinical scenarios in which the apnea test may be difficult to ascertain.
1. Chronic CO2 retention is commonly encountered in patients with a history of chronic obstructive pulmonary disease (COPD). It is well documented that chronic hypercapnia (pco2 50–70 mm Hg) results in a reduction of the chemoreceptor response. In such clinical instances, it is impossible to set target pco2 values with the apnea test. Although rare, situations may arise where brain death determination is warranted in a patient with COPD. In such cases, the apnea test cannot be reliably performed and further ancillary testing is indicated.
2. Breathing during the apnea test is usually seen in comatose patients with a catastrophic neurologic injury. Brain death exclusively implies that all respiration is absent. Careful re-examination may reveal a cough reflex or other brainstem function that excludes brain death as a diagnosis. In a small number of documented patients, small gasps and agonal breathing have been seen. In such instances a repeat of the apnea test 24 hours later resulted in a positive test. Once the apnea test is positive, breathing effort will not return. If breathing during the apnea test has truly been established, family conversation should switch to determine further goals of care.
3. Termination of the apnea test is a common concern that continues to exist. Factors associated with the need for early termination include insufficient preoxygenation, hypotension, pretest acidosis, and polytrauma. Review of most clinical scenarios demonstrates that patients are inadequately preoxygenated. Additionally, all test prerequisites are not typically met including SBP >90 mm Hg and PEEP supplementation (5 mm Hg) following disconnection from the ventilator. If hypotension occurs during testing, a trial of intravenous phenylephrine may be considered. In situations where adequate oxygenation is difficult to overcome, apnea testing may not be reliable and other investigations should be considered.
E. Cardiopulmonary resuscitation and hypothermia. Therapeutic hypothermia following cardiac arrest has become a standardized practice in most institutions. Brain death occurs in around 5% of patients following arrest. The institution of hypothermia has shown to be beneficial in improving long-term neurologic outcomes and thus utilized today. Most protocols use a combination of benzodiazepines, opioid analgesics, and neuromuscular blocking agents to achieve cooling goals. Such medications are confounders in the examination of brain death and can present a diagnostic challenge. Additionally, hypothermia itself changes the pharmacokinetics of most drugs and delays objective neurologic findings on exam. Some authors recommend delaying a definitive neurologic examination up to 1 week following therapeutic hypothermia compared to the typical 3 days. The clearance of most medications during this time has been shown to be delayed up to five times the norm. Following therapeutic hypothermia it is important that examiners allow for adequate time to pass in order to exclude all major confounders and proceed with assessment of brain death. The use of a checklist prior to examination is highly recommended.
Key Points
• Brain death is defined as the complete, irreversible loss of brain function, leading to viscerosomatic and cardiopulmonary failure.
• A definable set of evidence-based guidelines for the diagnosis of brain death are widely available and should be used consistently during evaluation.
• Clinicians should have a firm background in the criticism and interpretation of confirmatory testing in brain death.
• Physicians must have a deep understanding of the ethical, religious, and legal implications of a brain death diagnosis.
• Effective communication and education are vital in brain death, and a multidisciplinary care team should be used to achieve such goals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree