A. Neurally mediated syncope, also referred to as neurocardiogenic, reflex, or vasodepressor syncope, is common and results from the activation of a reflex that produces a significant vasodilatory (vasodepressor) and/or bradycardic (cardioinhibitory) response. Typically, it occurs after prolonged standing or sitting and may be reproduced on tilt-table testing. Long-term follow-up studies have shown that neurally mediated syncope carries a benign prognosis and a similar survival outcome to those patients with no history of syncope. Table 7.1 shows various etiologies that can lead to neurally mediated syncope. Almost all of these etiologies can be diagnosed by a carefully taken history. Classic vasovagal syncope may be considered in this group and usually occurs in the setting of emotional or orthostatic stress, although it can also have an atypical presentation with no clear triggering events or premonitory signs. A careful history should also diagnose the etiology of several causes of situational syncope (e.g., postprandial, postmicturition, postdefecation). Syncope due to carotid sinus hypersensitivity occurs in the setting of inadvertent mechanical pressure on the carotid sinus and can be reproduced by carotid sinus massage. Glossopharyngeal neuralgia may present with syncope associated with painful swallowing.
B. Orthostatic hypotension/orthostatic intolerance syndromes can cause inadequate cerebral perfusion leading to syncope upon rising from a sitting or supine to an upright position. The most common mechanism of hypotension is the loss of peripheral vascular tone because of failure of the autonomic nervous system to maintain peripheral vascular resistance. This can occur because of a primary dysfunction of the autonomic nervous system associated with several neurodegenerative conditions (multiple system atrophy) or because of diseases causing secondary autonomic nervous system failure (e.g., diabetes, amyloidosis). Multiple systems atrophy (MSA) encompasses a group of sporadic progressive neurologic disorders characterized clinically by autonomic dysfunction (i.e., orthostatic hypotension, impotence, urinary retention or incontinence, and so on), parkinsonism, and ataxia in any combination. Medications, alcohol, and drug toxicity should also be considered when evaluating orthostatic hypotension. Volume depletion (e.g., dehydration, hemorrhage, Addison’s disease) may cause or exacerbate orthostatic syncope. Combinations of medications that contribute to orthostatic hypotension are a particularly common and overlooked cause.
POTS is a form of orthostatic intolerance in which the HR elevates (>30 bpm) in response to orthostatic stress in the absence of hypotension (blood pressure decrease <20 mm Hg). Although presyncope is more common, syncope also occurs in addition to a variety of other symptoms.
C. Cardiac arrhythmias often present with syncope because of a decrease in cardiac output. This can occur in bradycardia (e.g., sinus arrest, heart block) or tachycardia (e.g., nonsustained ventricular tachycardia/fibrillation). It is relatively uncommon for supraventricular tachycardias to cause syncope in the absence of other structural heart diseases or the Wolff–Parkinson–White syndrome (i.e., preexcited atrial fibrillation). Arrhythmic syncope may indicate a risk for sudden death and should be aggressively managed. In patients with congestive heart failure (CHF), syncope is associated with an increased risk of cardiovascular and total mortality.
D. Structural heart disease can cause syncope because of the inability to produce sufficient cardiac output to match demand. Obstructive valvular heart disease and hypertrophic cardiomyopathy are well-established etiologies. Primary pump failure due to myocardial dysfunction can also lead to syncope; however, associated ventricular arrhythmias are a more common cause. Other less common conditions include atrial myxoma and pericardial tamponade.
E. Cerebrovascular and other vascular causes of syncope are rare. These include acute aortic dissection and steal syndromes, such as subclavian steal, in which CBF is shunted away from the brain. Obstruction of CBF is a rare cause of true syncope. Most carotid artery distribution transient ischemic attacks (TIAs) cause unilateral visual impairment, weakness, or loss of sensation. Posterior circulation TIAs generally manifest as vertigo, diplopia, unilateral or bilateral hemianopia, ataxia or disequilibrium, but not loss of consciousness. Rare patients with TIA may have TLOC, but isolated syncopal episodes without accompanying neurologic symptoms should generally not be ascribed to a TIA.
F. Psychogenic “syncope” (pseudosyncope) is a form or TLOC mimicking syncope that occurs without any substantial changes in hemodynamics and is often associated with a prior significant psychologic event. Physical causes must be excluded. It and other causes are included in the differential diagnosis of TLOC, but are usually distinguished from true syncope.
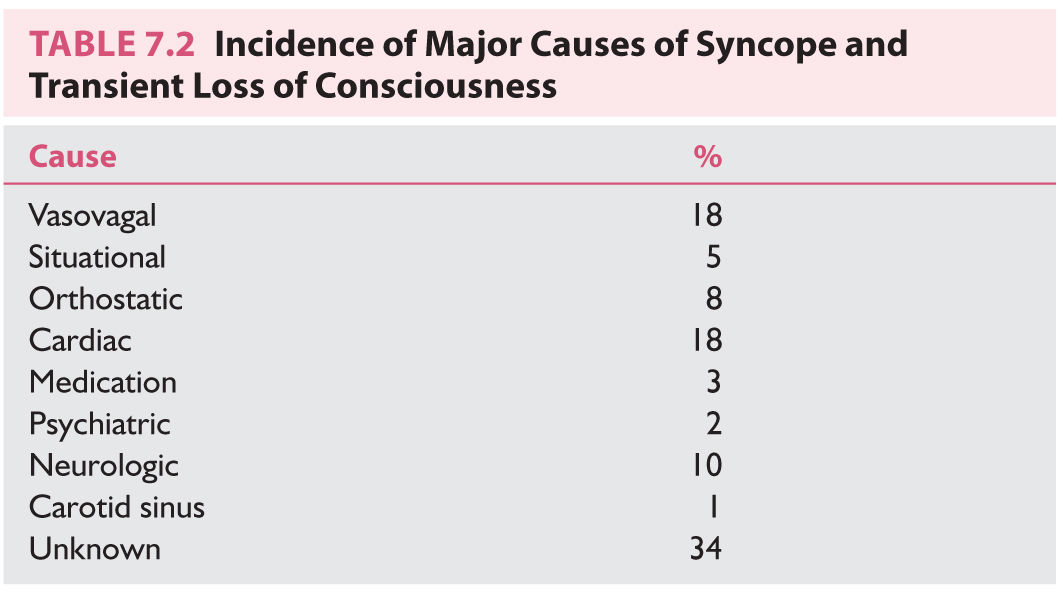
G. Syncope of unknown origin is a diagnosis made after a careful history, physical examination, and selected laboratory tests have failed to elucidate a specific etiologic factor. Up to 40% of syncope may fall into this category. This diagnosis is clinically useful because it is associated with a prognosis considerably better than that of patients who have identifiable cardiac or neurologic causes of syncope. Although long-term follow-up studies have shown that patients with syncope and a history of cardiac or neurologic disease may have increased mortality rates, those patients with syncope of unknown causation have a distinctly better prognosis.
H. TLOC from neurologic or other causes, such as seizures or concussion, are distinct from syncope and are covered elsewhere (see Chapters 6, 37, 42, and 43).
EVALUATION
The evaluation of syncope should address these key questions:
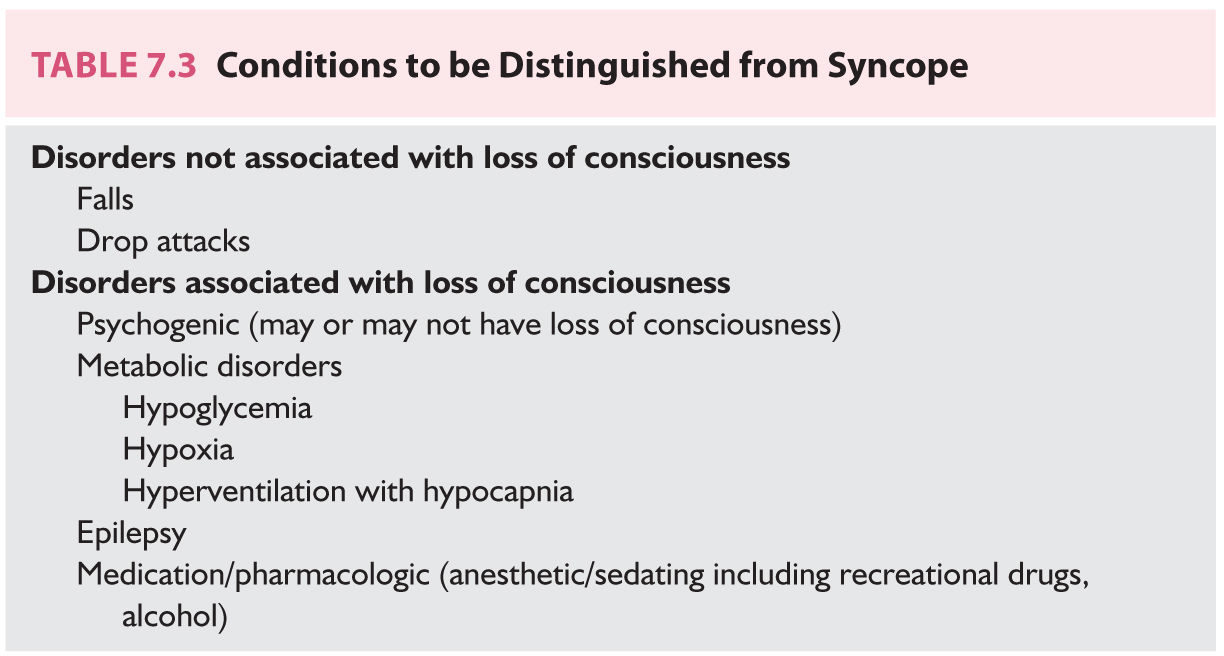
• Was the loss of consciousness attributable to true syncope or to other causes? A careful history is crucial for making the diagnosis and excluding nonsyncopal etiologies. Table 7.3 lists some conditions that are commonly distinguished from syncope, some of which are associated with a TLOC.
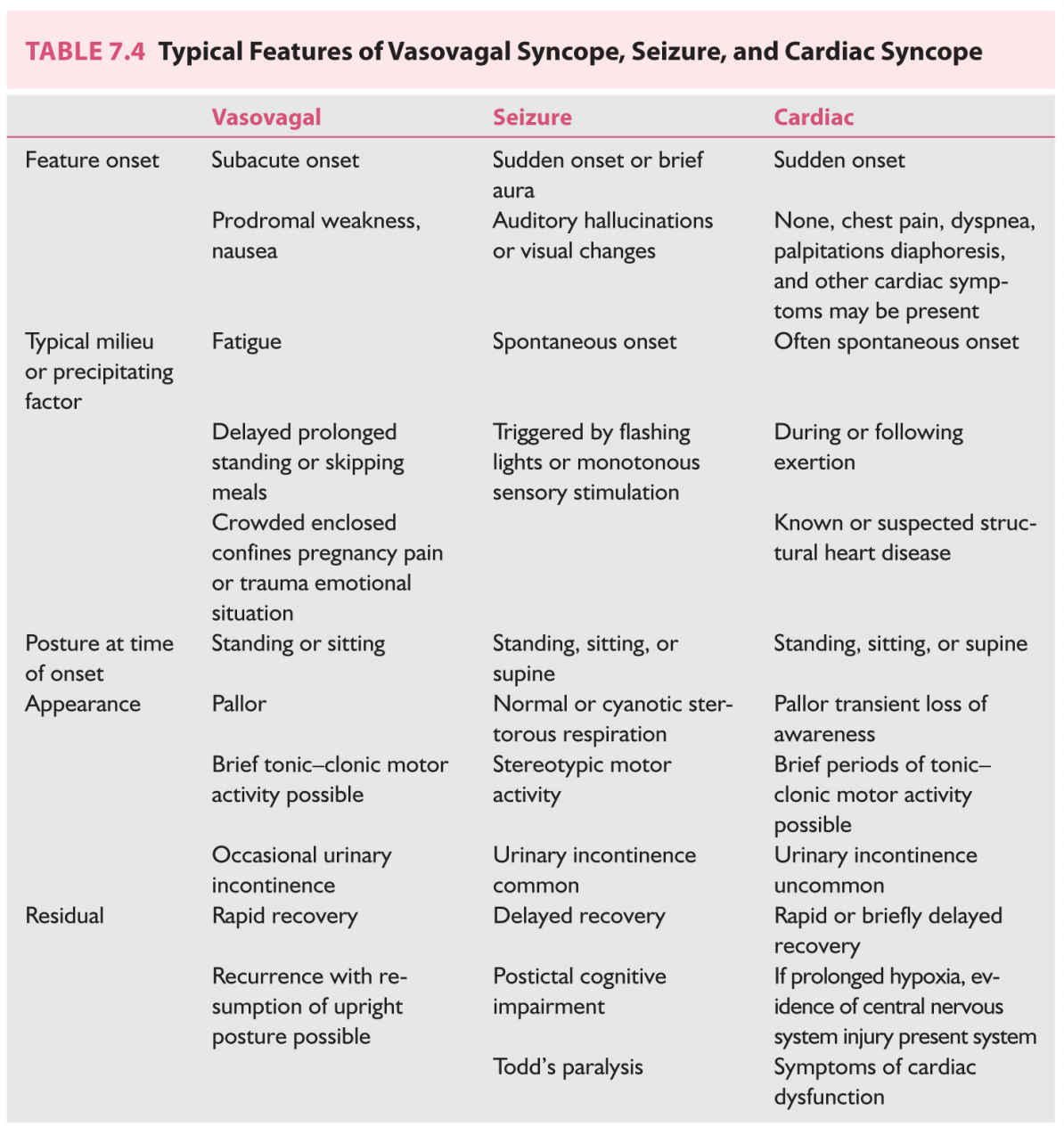
• Which distinguishing features exist that may indicate the diagnosis? Table 7.4 lists features of vasovagal syncope, seizures, and cardiac syncope.
• Is heart disease present? This is an important question not only for diagnosis, but also for prognosis. Patients with syncope often have a fairly benign clinical course in the absence of heart disease. On the other hand, the presence of cardiac disease may carry a much more ominous prognosis.
• Is the patient at risk of sudden death? As syncope can be a manifestation of a life-threatening condition, a determination of patient risk should be made relatively early on.
Answering these questions can often largely be accomplished by an astute evaluation of the history and physical examination alone. Additional studies are used as needed to provide further insight or to guide therapy.
A. History.
The history is by far the most crucial component of the evaluation of syncope. In many cases, a good history alone can point to the diagnosis and afford a good evaluation of risk. Particular attention should be paid to the following points:
1. Patient characteristics. In addition to the patient’s current age and gender, the age of onset of syncope yields relevant clues in recurrent cases. A long-standing history of syncope from a young age in an otherwise healthy individual may suggest a neurocardiogenic etiology. Comorbidities are often relevant to the diagnosis. The most important prognostic factor in patients presenting with syncope is the presence of cardiac disease. Known comorbidities such as coronary artery disease, hypertension, congestive heart failure, hypertrophic obstructive cardiomyopathy, and valvular disorders require special emphasis. Symptoms associated with cardiac conditions such as palpitations, dyspnea, fluid retention, decreased exercise tolerance, lightheadedness, or chest pain require further evaluation.
2. Events leading to syncope. A patient’s activity and posture before the episode should be noted. Syncope that occurs while supine may favor either an arrhythmic etiology or seizure, and largely excludes the etiologies dependent on orthostatic stress. Conversely, syncope occurring shortly after standing is typically because of orthostatic hypotension, while syncope during prolonged standing is most often neurocardiogenic. Vasovagal syncope is likely if the event was triggered by fear, pain, emotional distress, or blood draw.
Syncope occurring during or immediately after urination, defecation, coughing, or swallowing is a feature of situational syncope. Postprandial syncope is characterized by episodes that occur 15 to 90 minutes following meals. Syncope in the setting of neck manipulation such as extension, flexion, rotation, or compression (e.g., a tight shirt collar, necktie, or during shaving) may suggest carotid sinus hypersensitivity.
Syncope in the setting of exercise is particularly worrisome for a cardiac etiology. Syncope during physical exertion is a characteristic finding in aortic stenosis, atrioventricular (AV) block, or tachyarrhythmias, whereas loss of consciousness after exercise should arouse suspicion for hypertrophic cardiomyopathy or ventricular arrhythmia.
3. Prodromal signs and symptoms often provide clinically relevant information. Very brief prodromal symptoms lasting only seconds are a characteristic of cardiac causes, situational syncope, and orthostatic hypotension. Cardiac causes of syncope often do not have any prodromal symptoms or may present with dizziness and/or palpitations. On the other hand, vasovagal syncope typically has a more sustained warning period accompanied by symptoms of nausea, diaphoresis, and flushing. Focal neurologic symptoms such as vertigo, diplopia, ataxia, dysarthria, hemiparesis, and unilateral numbness are uncommon and may be indicative of a TIA as the cause of the loss of consciousness.
4. Events during the syncopal period. Though this typically requires the presence of a witness, obtaining as much detail as possible regarding the events during the syncopal episode may be highly valuable. The patient may be amnestic for events before, during, and after the episode. Often patients deny the loss of consciousness, even when it occurs. A detailed history confirming a true loss of consciousness and describing neuromuscular activity is extremely valuable. Although prolonged episodes of cerebral anoxia (more than 10 to 15 seconds) can induce brief involuntary motor activity, the presence of more sustained episodes of alternating tonic and clonic muscle action is strongly suggestive of a seizure. Urinary incontinence is more frequent among patients with seizures, although it can accompany syncope of any cause. Fecal incontinence is more specific for seizures.
5. Postsyncopal events. Details of events immediately following the loss of consciousness may provide important diagnostic clues. This history may also need to be obtained from witnesses. Prolonged duration of confusion, amnesia, or lethargy is more consistent with seizure activity rather than a cardiac or neurally mediated event. Similarly, the presence of focal neurologic symptoms or signs points to an inciting neurologic event such as a seizure with residual functional deficit (Todd’s paralysis) or ischemic injury. Facial pallor points to syncope, facial plethora is more suggestive of seizure, and diffuse muscle soreness suggests seizure activity (see Chapters 5, 6, 42, and 43).
6. Family history. A family history of syncope, arrhythmias, or early sudden cardiac death may point to a genetic condition linked to ventricular arrhythmias, even in the absence of structural heart disease. Such a history should prompt more detailed cardiac investigation.
7. Comorbid conditions. In addition to the emphasis placed on obtaining a detailed history of any cardiovascular pathology, other comorbidities may be of relevance.
The history taker should address the possibility of neurologic disorders predisposing to seizures mimicking syncope. This includes primary or metastatic neoplasia, as well as a history of previous trauma, infection, and ischemic or hemorrhagic injury to the brain. Medical conditions such as diabetes mellitus, alcohol abuse, vitamin B12 deficiency, or other metabolic disorders are associated with peripheral or autonomic neuropathy and can cause orthostatic hypotension.
A gynecologic history should be elicited in appropriate patients to identify risk factors for pregnancy, particularly in ectopic locations. Pregnant patients are at increased risk of syncope because of orthostatic hypotension and vasovagal reactions. Moreover, a ruptured ectopic pregnancy occasionally manifests with syncope.
A history of anxiety disorders and depression is important to elucidate. Psychiatric illness should be suspected as a potential etiology, especially in patients with severe, atypical, repetitive, and drug-refractory episodes. Patients with psychogenic syncope may have reproducible symptoms on tilt-table testing despite a normal HR, blood pressure, and electroencephalography (EEG).
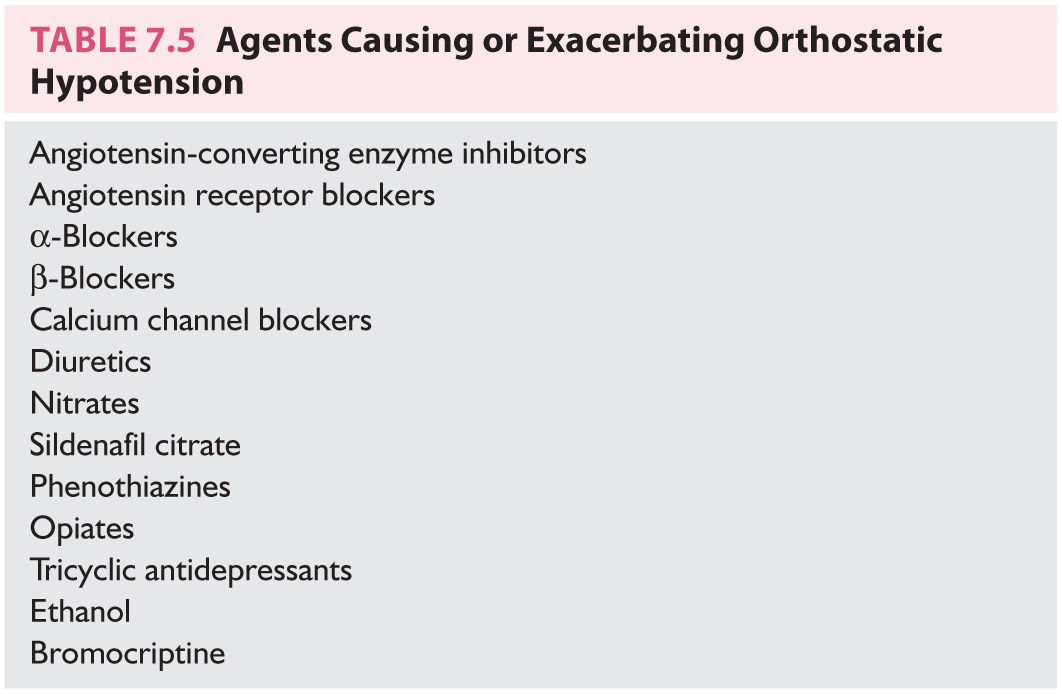
Finally, careful review of the patient’s medication list is essential. Antihypertensive and other drugs can cause syncope by reducing cardiac output and lowering peripheral vascular resistance. As shown in Table 7.5, many antihypertensive and psychotropic medications can induce orthostatic hypotension. Numerous drugs can prolong the QT interval and may provoke ventricular arrhythmias that lead to syncope. Combinations of drugs can often be the culprit.
B. Physical examination.
1. Vital signs should include an assessment of orthostatic hypotension, which is defined as a decrease of 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic blood pressure following standing from a supine position. It is important that the supine blood pressure be obtained after at least 5 minutes of recumbency and the standing blood pressure measured initially and again after the patient has been erect for at least 2 minutes.
2. Given the prognostic importance of cardiac disease, a detailed cardiovascular examination should be performed. Palpation of the carotid arteries may demonstrate weak and delayed carotid pulsation (pulsus parvus et tardus), which occurs with hemodynamically significant aortic stenosis, or biphasic carotid pulsation (pulsus bisferiens), which may be found in hypertrophic obstructive cardiomyopathy. Similarly, particular attention should be paid to the presence of systolic–crescendo–decrescendo murmurs, implying the presence of aortic stenosis or hypertrophic obstructive cardiomyopathy. Peripheral edema, elevated jugular venous pressure pulmonary crackles, hepatomegaly, and a third heart sound (S3) signify heart failure. The presence of a carotid bruit signifies a high likelihood of diffuse atherosclerotic vascular disease involving the cerebral, coronary, and peripheral vasculature. A supraclavicular bruit and a diminished upper extremity arterial pulsation are evidence of subclavian steal syndrome.
If carotid sinus supersensitivity is suspected, carotid massage can be performed in the absence of a bruit or known atheromatous disease. Carotid sinus hypersensitivity can be detected by means of monitoring changes in blood pressure and HR after 5 to 30 seconds of unilateral carotid artery massage. Responses are characterized as cardioinhibitory, vasodepressor, or mixed. Carotid sinus hypersensitivity is more common in older patients. Electrocardiographic and resuscitation equipment should be available.
3. A screening neurologic examination should be pursued to detect cognitive impairment, the presence of focal neurologic defects indicative of either acute neurologic injury or a preexisting substrate for a seizure disorder, peripheral neuropathy that would predispose to orthostatic hypotension, or a movement disorder that would cause nonsyncopal falls.
4. A digital rectal or stool examination should be considered if there is concern about gastrointestinal bleeding.
C. Laboratory and other studies.
1. Electrocardiography (ECG)
a. ECG. The resting 12-lead ECG is an important test for both prognosis and triage. Although it is relatively uncommon for the ECG to directly demonstrate an arrhythmic cause for syncope, the presence of pathologic Q waves, left axis deviation, left bundle branch block, or left ventricular hypertrophy may point to underlying cardiac pathology. Severe sinus bradycardia or AV block may be diagnostic. Other ECG signs may suggest pulmonary embolism
Repolarization abnormalities also may provide clues critical to determining the etiology of syncope. These include long QT intervals (long QT syndrome), epsilon waves with precordial T-wave inversions (arrhythmogenic right ventricular dysplasia/cardiomyopathy), and right bundle branch block with coved ST elevation in leads V1-V3 (Brugada’s syndrome). Abnormally short QT intervals may also be relevant.
b. Ambulatory electrocardiography. Ambulatory electrocardiography has become a critical tool in the diagnosis of syncope. Because of the transient nature of arrhythmias causing syncope, routine 12-lead ECGs rarely capture the culprit arrhythmia, and extended monitoring is often required to make a definitive diagnosis. Several types of monitors could be used, depending on the frequency of the symptoms: 24-hour continuous recordings, patient-activated looping and nonlooping event monitors, and continuous 24-hour monitors that can be worn up to a period of 30 days or more.
Ambulatory monitoring has limited specificity because certain rhythm disturbances, such as brief pauses, premature atrial and ventricular contractions, and nonsustained ventricular tachycardia, can be detected even when they are not responsible for the syncope. Thus, it is important to correlate the findings of ambulatory monitoring with symptoms. If symptoms occur during monitoring and no ECG abnormalities are detected, a rhythm disturbance is effectively excluded as an etiologic factor.
c. Implantable loop recorder (ILR). Of increasing utility, subcutaneous ILRs for long-term monitoring have become an essential tool in the evaluation of syncope of unknown etiology. Newer-generation ILRs can be injected in the anterior chest in a brief procedure requiring only a local anesthetic, and have the energy to run for several years. These devices can unmask or exclude cardiac arrhythmias as the cause of infrequent episodes of recurrent syncope when all other evaluation has been inconclusive.
2. Echocardiography is one of the most widely used tests when evaluating patients for cardiac disease. Echocardiography can provide clues regarding the etiology of syncope such as valvular heart disease or atrial myxoma. More importantly echocardiography can confirm or exclude the presence of left ventricular dysfunction, which is associated with a risk of sudden cardiac death and which carries important prognostic implications.
3. Blood laboratory testing. Serum electrolyte abnormalities should be excluded. Elevated prolactin levels have been reported in some patients hours after generalized tonic–clonic seizures. The same is true for creatine kinase levels, although increased serum concentrations also can be caused by injury during a syncopal episode. Serum glucose levels are most valuable at the time of the event, particularly in evaluation of diabetic patients who have recently increased their insulin or oral hypoglycemic therapy or decreased their caloric intake. A complete blood count is occasionally helpful if blood loss or severe anemia is suspected.
Arterial blood gas analysis can be useful in evaluation of the occasional patient in whom pulmonary embolism is suspected because of the history, physical examination findings, or ECG results.
4. Stress testing or coronary angiography to assess for coronary ischemia is appropriate in some patients, particularly the elderly, those with exertional symptoms (syncope, chest pain, or dyspnea), cardiomyopathy, or ventricular arrhythmias.
5. Electrophysiologic testing is used to assess the integrity of the sinus node, cardiac conduction system, as well as the predisposition to ventricular and supraventricular arrhythmias. However, sensitivity is limited. The results are most often abnormal in patients with known heart disease or those with significant abnormalities on a routine ECG. Findings of greatest diagnostic value include inducible monomorphic ventricular tachycardia, markedly abnormal sinus node recovery times, inducible supraventricular tachycardia with hypotension, significant infra-His conduction disease, and pacing-induced infra-His block. Recent studies have shown that patients with underlying left ventricular dysfunction are at high risk of arrhythmic death and benefit from prophylactic defibrillator insertion even in the absence of syncope. Thus, patients with syncope and left ventricular dysfunction may not necessarily benefit from electrophysiologic testing to assess inducibility of ventricular arrhythmias.
6. Tilt-table testing. The utility of tilt-table testing for the diagnosis of neurocardiogenic syncope remains poorly defined. It is only a moderately sensitive and specific test. A positive result is reproducible only 70% of the time. The limited reproducibility of the test and the variable natural history of unexplained syncope reduce its utility. Abnormal response patterns to tilt-table testing include the vasovagal response, which consists of a decrease in blood pressure (vasodepressor) and bradycardia (cardioinhibitory), and the dysautonomic response, which represents a failure of the autonomic system to compensate for an acute decrease in venous return that occurs with upright posture. Thus, the HR does not significantly change while the blood pressure declines. A third response to tilt-table testing is the POTS response in which there is a significant increase in HR in response to upright positioning.
7. Radiographic studies/magnetic resonance imaging (MRI). Routine head computed tomography (CT) and MRI of the brain have low yields but may be useful in the evaluation of patients who have sustained major head trauma, have a newly diagnosed seizure disorder, or have focal deficits on the neurologic examination (see Chapter 35). In addition, cardiac CT and MRI are becoming valuable means of detecting abnormal cardiac substrate that may not have been found by other means.
8. EEG is not required routinely, but should be performed when clinical evaluation points to seizure or in syncope of undetermined etiology when there is adequate suspicion (see Chapter 36).
9. Device interrogation. Patients with syncope in the presence of implanted pacemakers or implantable cardioverter defibrillators should have the devices checked by appropriate personnel. Not only should device malfunction be excluded as a cause of syncope, but modern devices store a plethora of diagnostic information that may be useful in diagnosis.
MANAGEMENT
The majority of syncope is of cardiovascular cause, and the diagnosis is often suggested after a complete history and physical examination. The goals of syncope management are twofold. One is prevention of further syncope and its potential effects including physical injury, driving risks, and work restrictions. Even more important is the prevention of sudden death in those at risk. Some patients with syncope from life-threatening cardiac disorders may appear healthy and be otherwise asymptomatic. For example, highly functional athletes, including at the professional level, may have malignant conditions (hypertrophic cardiomyopathy, genetic causes of ventricular arrhythmias, and so on) that lead to sudden cardiac death.
If the cause is unclear, evaluation of a resting 12-lead ECG should be performed in nearly all patients. Patients with symptoms or signs of cardiac disease, those with abrupt syncope without warning, and those with a concerning family history of sudden death receive more detailed cardiac evaluation, which often includes echocardiography, evaluation for coronary artery disease, and referral to a cardiologist or electrophysiologist. Further cardiac testing, including electrophysiologic studies and/or long-term cardiac monitoring, may be appropriate (see ![]() Video 7.1). Patients with unexplained syncope at high risk may be appropriate for preventive therapies, including the implantation of cardiac rhythm devices. Neurocardiogenic syncope can sometimes be difficult to manage because of the limitations of currently available therapies. Some orthostatically induced causes can also be challenging. Treatment should be in accordance with recent guidelines. When the symptoms are deemed not to be of cardiovascular etiology or are nonsyncopal (e.g., seizure, psychogenic, traumatic), the patient should be managed accordingly or referred to the appropriate specialist.
Video 7.1). Patients with unexplained syncope at high risk may be appropriate for preventive therapies, including the implantation of cardiac rhythm devices. Neurocardiogenic syncope can sometimes be difficult to manage because of the limitations of currently available therapies. Some orthostatically induced causes can also be challenging. Treatment should be in accordance with recent guidelines. When the symptoms are deemed not to be of cardiovascular etiology or are nonsyncopal (e.g., seizure, psychogenic, traumatic), the patient should be managed accordingly or referred to the appropriate specialist.
Key Points
• Syncope, even when broadly defined, is most commonly cardiovascular in etiology.
• Though most cases are of benign etiology, recurrent symptoms can severely impact quality of life and should be aggressively managed.
• Syncope can be the initial manifestation of serious cardiovascular conditions that may place the patient at risk of sudden death.
• With proper knowledge and questioning, the diagnosis is often suggested after a complete history and physical examination.
• The goals of syncope evaluation and management are twofold. One is the prevention of further syncope when feasible. However, the evaluation of risk and the prevention of sudden death are even more critically important.
• An assessment for heart disease is appropriate in many cases, particularly if the diagnosis is uncertain after the initial evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree