Chapter 196 Arachnoiditis
Spinal arachnoiditis is a nonspecific inflammatory process of the arachnoid layer of the spinal cord or cauda equina. Arachnoiditis was first described by Victor Horsley in 1909.1 Since Horsley, numerous authors have described this condition with a variety of terms, including chronic spinal arachnoiditis, adhesive spinal arachnoiditis, meningitis serosa circumscripta spinalis, chronic spinal meningitis, spinal meningitides with radiculomyelopathy, lumbar adhesive arachnoiditis, spinal arachnoiditis, spinal fibrosis, and lumbosacral adhesive arachnoiditis. Furthermore, on the basis of the specific radiographic or pathologic findings, arachnoiditis can be termed arachnoiditis ossificans, calcific arachnoiditis, or pachymeningitis.1
Anatomy
The arachnoid mater is an avascular membrane that lies between two vascularized membranes: the pia mater and the dura mater. The arachnoid is attached to the underlying pia by numerous arachnoid trabeculae, which create a space between the arachnoid and the pia.2 This space, or potential space in some instances, transmits arterioles and is referred to as the subarachnoid space. The arachnoid is composed of layers of squamous cells held together by a network of connective tissue. The arachnoid contains intercellular pores that allow for the passage of molecules.3
Pathogenesis
A chronic infection or irritation can cause the arachnoid membrane to become thickened and adherent to both the overlying dura mater and the subjacent pia mater.4 The pia-arachnoid carries the blood vessels to the spinal cord, and this layer contains mesenchymal cells. In 1951, Smolik and Nash recognized that when the outer arachnoid layer is injured, both the blood vessels and mesenchymal cells lend themselves to extensive proliferation. The ensuing reaction between the pia-arachnoid and the dura mater leads to obliterative arachnoiditis.5
When the arachnoid membrane is exposed to an insult, an inflammatory response ensues, which is characterized by fibrinous exudates, neovascularization, and a relative paucity of inflammatory cellular exudates.6,7 Vascular occlusive changes can occur, which can lead to spinal cord ischemia.4,8–11 The small perforating blood vessels that supply the portions of the white matter may be obliterated, with resultant necrosis and cavitation of the spinal cord parenchyma.8,9,11 In addition to ischemia, blockage of venous return from the spinal cord or occlusion of cerebrospinal fluid (CSF) pathways may occur.8
Burton described the stages of progressive inflammation of the arachnoid that occur in lumbosacral arachnoiditis. The initial stage, radiculitis, consists of an inflamed pia-arachnoid with associated hyperemia and swelling of the nerve roots. The second stage, arachnoiditis, is characterized by fibroblast proliferation and collagen deposition. During this stage, nerve root swelling decreases, and the nerve roots adhere to each other and to the pia-arachnoid. The final stage, adhesive arachnoiditis, is the resolution of the inflammatory process and is characterized by dense collagen deposition. There is marked proliferation of the pia-arachnoid as well as complete nerve root encapsulation, hypoxemia, and progressive atrophy.12 For reasons that are not fully understood, the adhesions occur preferentially on the dorsal segments.1 The exact time course of these three phases has not been elucidated. Furthermore, it is not known how the specific causative insult for the development of arachnoiditis might affect the time course of each of the three phases.
Yamagami et al. postulated that the pathologic changes in arachnoiditis may be secondary to diminished nutritional supply. They found that in an experimental rat model, the development of arachnoiditis and neural degeneration directly corresponded to the magnitude of extradural inflammation and wound-healing processes that occurred after laminectomy, with or without foreign bodies. Furthermore, adhesions of the arachnoid cause the nerve roots to lump together, and in the process, these nerve roots are isolated from contact with the CSF, with resultant nutritional compromise.13
Etiology
In the first half of the 20th century, arachnoiditis was most often attributed to infectious causes.8 Furthermore, arachnoiditis had been described mainly in the cervical and thoracic regions.1 Since the 1950s, there has been a trend toward a higher incidence of arachnoiditis of noninfectious origin affecting the lumbar region.1,8 The precise causes of spinal arachnoiditis are not clear; likewise, the incidence and prevalence of spinal arachnoiditis in the general population are unknown8 (Table 196-1).
TABLE 196-1 Causes of Spinal Arachnoiditis
| Infectious | Noninfectious |
|---|---|
| Tuberculosis | Trauma |
| Bacterial infections | Postsurgery |
| SyphilisParasitic diseasesViral meningitis | Myelographic contrast media (oil-based > water-soluble; water-soluble ionic > water-soluble nonionic) |
| Intrathecal medications | |
| Steroids | |
| Anesthesia | |
| Epidural injections | |
| Neoplasms | |
| Arthritis (especially ankylosing spondylitis) | |
| Spinal stenosis | |
| Herniated intervertebral disc | |
| Intrathecal hemorrhage | |
| Foreign materials |
As was stated previously, arachnoiditis was mainly of infectious origin in the first half of the 20th century. Syphilis, tuberculosis, and gonorrhea were the most prevalent causes.1,14 Less common infectious causes include parasitic diseases and viral meningitis.15,16 These infectious causes are important to differentiate from noninfectious causes of arachnoiditis because, in most cases, effective treatment is available for arachnoiditis of infectious origin. However, despite adequate treatment of the causative agent, scarring of the arachnoid membrane may lead to permanent damage.
Arachnoiditis has a number of important noninfectious etiologies. In the 1940s, blood in the CSF following subarachnoid hemorrhage or surgery became the most prevalent cause of arachnoiditis.1 Spinal arachnoiditis following subarachnoid hemorrhage continues to be common and is usually treated in a conservative fashion.17 The breakdown products of hemoglobin form free radicals, and it has been postulated that these cause damage to nerves.18,19 In experiments on dogs, it has been shown that injecting blood breakdown products into the subarachnoid space causes more meningeal inflammation than does the injection of fresh blood.18 Cases of patients who have received epidural blood patches have given controversial results. Digiovanni et al. described that the placement of an autologous blood patch into the epidural space produced no more inflammation than a standard lumbar puncture.20 Other authors, though, have described cases in which an epidural blood patch had allegedly been responsible for arachnoiditis.21 Abouleish et al. described 118 cases of epidural blood patches over a 2-year period. This group found 19 cases of axial back pain, 2 cases of radiculopathy, and no cases of arachnoiditis.22
Oil-based contrast media have been an historically important cause of arachnoiditis. Iophendylate (Myodil, Pantopaque) is an oil-based contrast medium used in diagnostic myelograms. It was first used in the United States in 1944, and its usage continued for 40 years. In Sweden, iophendylate was banned from clinical use in 1948 because of animal studies that identified it as a causative agent for arachnoiditis.23 The incidence of arachnoiditis after the use of iophendylate is dose dependent and is quoted as 1%.24 Iophendylate has a very long half–life, so it is usually removed from the thecal space by aspiration at the conclusion of the myelogram.8 Often, this removal process is not entirely successful; in fact, incomplete removal of the contrast dye may produce further trauma and cause bleeding into the CSF.25
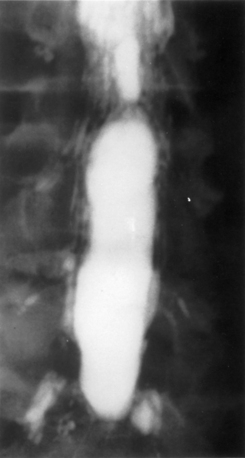
Guyer et al. listed the following factors as influencing the development of arachnoiditis after myelography: the type of contrast agent used (the risk is greater with oil-based than with water-soluble media and greater with ionic than with nonionic media), the dosage of contrast medium, and the observation time after myelography25 (Fig. 196-1).
The use of intrathecal medications, either steroids or anesthetic agents, has been implicated as a cause of arachnoiditis. Intrathecal injection of corticosteroids was previously used for multiple sclerosis.8 Epidural injection of corticosteroids for back pain is a common practice. One of the most commonly used agents is methylprednisolone acetate (MPA), which has been reported to cause arachnoiditis.26–28 MPA is suspended in polyethylene glycol, which can cause arachnoiditis.26–28 Furthermore, MPA is known to easily cross the intrathecal space, thus causing arachnoiditis.28 However, animal studies have not shown MPA to cause significant meningeal inflammation after epidural injections.29–31
The use of intrathecal bupivacaine, with or without epinephrine, has also been reported to cause arachnoiditis. Boiardi et al. described several cases of arachnoiditis after administration of bupivacaine with epinephrine.32 Gemma et al. described a case of arachnoiditis after intrathecal administration of bupivacaine without epinephrine.33 It is unclear in these cases whether the arachnoiditis was triggered by the bupivacaine or other preservatives. Furthermore, it is unclear whether epinephrine plays a role in the pathogenesis of arachnoiditis.
A history of spine surgery is a risk factor for arachnoiditis.8 In particular, some investigators have specifically stated that surgery for a herniated intervertebral disc may lead to arachnoiditis.5,7,25 Carroll and Wiesel showed that a postoperative pain-free interval lasting between 1 and 6 months, followed by the gradual onset of leg pain, increases the likelihood that some scar tissue is responsible for the symptoms.34 Smolik and Nash showed that simple dural retraction for the visualization of a ruptured intervertebral disc may trigger arachnoiditis.5 Haughton et al. showed that in monkeys, the nucleus pulposus of an intervertebral disc was able to cause focal arachnoiditis.35
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree