Artificial Disk Surgery of the Cervical Spine: Multilevel Disk Replacement and Arthroplasty Adjacent to Interbody Fusion
Gerald M.Y. Quan
Vincent Pointillart
MULTILEVEL CERVICAL DISK REPLACEMENT IN CERVICAL SPONDYLOSIS
In recent times, there has been an increasing trend in the use of cervical disk replacement for the reconstruction after anterior decompressive surgery for multilevel cervical spondylosis. Important advantages of this newer technology over the traditional procedures are that problems associated with long fusions are avoided and that motion at the operated segments is maintained. With multilevel anterior cervical discectomy and fusion (ACDF), the outcomes worsen in terms of pseudarthrosis and reoperation rates, as the number of vertebral fusion levels increases (1,2). Pseudarthrosis rates of greater than 25% have been reported with two- or three-level arthrodeses with bone grafting and without instrumentation, presumably because of increased motion and compressive loads resulting from the multiple discectomies. A significant proportion of these patients have inferior clinical outcomes and ongoing pain requiring revision surgery (1). The addition of an anterior cervical plate may decrease the incidence of nonfusion, although higher rates of pseudarthrosis and instrumentation failure have still been reported for multilevel compared with single-level instrumented fusions (3), and anterior plating itself has known associated morbidity. Alternatively, a cervical corpectomy may reduce the number of surfaces at which fusion is required but increases operating time and bleeding risk and creates a mechanically more demanding environment for the graft. Furthermore, the incidence of graft displacement and instrumentation failure in cervical corpectomy is also directly related to the number of vertebral bodies removed.
In contrast to multilevel ACDF, however, the clinical outcome of multilevel cervical arthroplasty remains consistent with increasing levels of implantation (4). The increasing morbidity and complication rates associated with a greater number of vertebral fusion levels are not evidently observed with multilevel cervical arthroplasty. Pseudarthrosis is not a problem, cervical disk replacements have no ventral profile, and postoperative external immobilization or the limitation of activity is not obligatory, thus potentially allowing earlier resumption of normal activities. No catastrophic failure of any artificial disk prosthesis has been reported, and intermediate-term radiologic evidence supports maintenance of motion (5,6). In a prospective study comparing 31 patients who had bi-level arthroplasty with 34 patients who had bi-level instrumented ACDF, both groups had marked improvement in neck and arm pain visual analogue scores and neck disability index at 2-year follow-up (7). However, the arthroplasty group had greater improvement in neck disability index scores than the ACDF group. Interestingly, another prospective study noted a significantly greater improvement in clinical outcome scores in 69 patients who underwent multiple level cervical arthroplasty, compared with 71 patients who underwent single-level disk replacement surgery (4). The reasons for this were unclear and may be a reflection of reporting bias or positive bias of patient-reported outcomes as a result of receiving the newer technology. In a multicenter European trial on the Bryan cervical disk replacement (Medtronic, Sofamor Danek, Tennessee, USA), the success rate for bi-level implantation of the Bryan disk at 12 months using Odom’s criteria was 96%, although only 26 out of 43 patients achieved the follow-up period (5).
To investigate the long-term outcome of patients who have undergone cervical arthroplasty, the authors evaluated clinical and radiologic outcomes in a series of 21 patients who underwent a total of 27 cervical arthroplasties with the Bryan cervical disk, at a minimum of 8 years of follow-up.
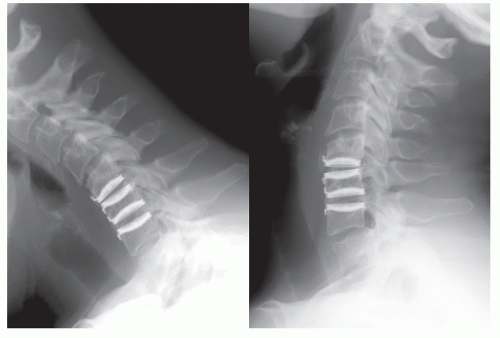
The results of the 6 patients who received bi-level arthroplasties were compared to 15 patients who underwent single-level procedures. Overall, the arthroplasty group maintained favorable clinical and radiologic results at longterm follow-up, with greater than 90% of patients reporting fair to excellent outcome according to Odom’s criteria and able to perform daily work and/or recreational duties without limitation. There was no significant difference in clinical outcome between bi-level versus single-level cases. No patient had clinical or radiologic evidence of recurrent spondylosis at the operated level, and no patient required revision surgery. Overall, the cervical arthroplasty maintained range of motion in vivo after 8 years in 78% of cases. Functioning prostheses had an average range of movement of 10.6 degrees, which was similar to that of the adjacent nonoperated segments of the cervical spine. Spontaneous fusion associated with bony ankylosis bridging the vertebral bodies above and below the prosthesis of the arthroplasty occurred in six cases (24%), which is slightly greater than the 10% to 17% fusion rates reported by others at 1- and 2-year follow-up (4,7, 8 and 9). The incidence of spontaneous fusion of the arthroplasty was not different in bi-level versus single-level cases. Most of the fused arthroplasties occurred at the C6-C7 level, and of the three fused arthroplasties that occurred in bi-level procedures, the fused prosthesis was always at the inferior of the two levels (Fig. 95.1). Radiographic evidence of adjacent segment degeneration was observed in four patients (19%), including in three patients with immobile arthroplasties; however, all these patients had preexisting degenerative disk disease on preoperative anatomical imaging studies. Almost half of all patients and operated segments in the authors’ series had radiographic evidence of heterotopic ossification (HO) at the 8-ye ar follow-up period (Fig. 95.1). We observed a higher rate of HO in bi-level (66.7%) compared with single-level (33.3%) operated segments, which is consistent with the observations of others (9). Nine out of the thirteen (69.2%) segments that developed HO in our series had HO within the intervertebral planes of the prosthesis that either restricted range of motion or caused bony ankylosis. The clinical implications of this are uncertain, since no clear association between development of HO or restricted motion and inferior clinical outcome has been demonstrated in any clinical study on cervical arthroplasty to date.
The results of the 6 patients who received bi-level arthroplasties were compared to 15 patients who underwent single-level procedures. Overall, the arthroplasty group maintained favorable clinical and radiologic results at longterm follow-up, with greater than 90% of patients reporting fair to excellent outcome according to Odom’s criteria and able to perform daily work and/or recreational duties without limitation. There was no significant difference in clinical outcome between bi-level versus single-level cases. No patient had clinical or radiologic evidence of recurrent spondylosis at the operated level, and no patient required revision surgery. Overall, the cervical arthroplasty maintained range of motion in vivo after 8 years in 78% of cases. Functioning prostheses had an average range of movement of 10.6 degrees, which was similar to that of the adjacent nonoperated segments of the cervical spine. Spontaneous fusion associated with bony ankylosis bridging the vertebral bodies above and below the prosthesis of the arthroplasty occurred in six cases (24%), which is slightly greater than the 10% to 17% fusion rates reported by others at 1- and 2-year follow-up (4,7, 8 and 9). The incidence of spontaneous fusion of the arthroplasty was not different in bi-level versus single-level cases. Most of the fused arthroplasties occurred at the C6-C7 level, and of the three fused arthroplasties that occurred in bi-level procedures, the fused prosthesis was always at the inferior of the two levels (Fig. 95.1). Radiographic evidence of adjacent segment degeneration was observed in four patients (19%), including in three patients with immobile arthroplasties; however, all these patients had preexisting degenerative disk disease on preoperative anatomical imaging studies. Almost half of all patients and operated segments in the authors’ series had radiographic evidence of heterotopic ossification (HO) at the 8-ye ar follow-up period (Fig. 95.1). We observed a higher rate of HO in bi-level (66.7%) compared with single-level (33.3%) operated segments, which is consistent with the observations of others (9). Nine out of the thirteen (69.2%) segments that developed HO in our series had HO within the intervertebral planes of the prosthesis that either restricted range of motion or caused bony ankylosis. The clinical implications of this are uncertain, since no clear association between development of HO or restricted motion and inferior clinical outcome has been demonstrated in any clinical study on cervical arthroplasty to date.
In summary, observations from the authors’ 8-year follow-up study suggest that there is no significant difference in clinical outcome at long-term follow-up of bi-level versus single-level cervical arthroplasty. However, multilevel arthroplasty had a higher rate of HO, which may restrict range of movement of the prosthesis in the longer term. There was no significant difference in the spontaneous fusion rate of multi- versus single-level arthroplasty, but when spontaneous fusion of the prosthesis occurred in bi-level cases, it always occurred at the inferior of the two levels.
MULTILEVEL ARTHROPLASTY FOR MYELOPATHY DUE TO CERVICAL SPONDYLOSIS
The clinical outcomes of myelopathic patients with congenital stenosis and hard cervical disks or osteophytes treated with single- or multilevel cervical decompression and total disk replacement are uncertain at this time. Concerns regarding motion preservation may lead to continued microtrauma to the compromised spinal cord, leading to either progression of myelopathy or lack of postoperative improvement of symptoms. Recurrent stenosis may occur as a result of the redevelopment of osteophytes and syndesmophytes as a result of retaining motion. However, neither of these complications has been comprehensively described in the literature to date. Early outcomes are encouraging but currently limited to case series with low patient numbers and limited follow-up. In one study, 106 patients with myelopathy secondary to cervical spondylosis treated with anterior cervical decompression and single- or multilevel arthroplasties had clinical outcomes and average improvement in Nurick grade at 2 years similar to 93 patients treated with arthrodesis (10). In another series of seven myelopathic patients who had anterior cervical decompression and cervical disk replacement, an average Nurick grade improvement of 0.72 occurred at mean 6-month follow-up (11). It is noteworthy that one
patient who had bi-level arthroplasties had temporary short-term worsening of hand and gait dysfunction, attributed to worsening of a preoperative kyphosis at the operated level.
patient who had bi-level arthroplasties had temporary short-term worsening of hand and gait dysfunction, attributed to worsening of a preoperative kyphosis at the operated level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree