and Thomas Verse1
(1)
Department of Otorhinolaryngology Head and Neck Surgery, Asklepios Clinic Harburg, Eissendorfer Pferdeweg 52, 21075 Hamburg, Germany
Abstract
Obesity, a widespread and increasing health problem within the US and Europe, is, among others, associated with OSA. Bariatric surgery encompasses a variety of surgeries. The most important ones are adjustable gastric banding, vertical banded gastroplasty, sleeve gastrectomy, intragastric balloons, jejunal bypass, biliopancreatic diversion, and Roux-en-Y gastric bypass. A significant reduction in BMI is associated with a comparable significant decrease in sleep apnea severity. Bariatric surgery is recommended for patients with a BMI > 35 kg/m2 and an obesity related concomitant disease or for patients with a BMI > 40 kg/m2.
Core Features
Obesity, a widespread and increasing health problem within the US and Europe, is, among others, associated with OSA.
Bariatric surgery encompasses a variety of surgeries. The most important ones are adjustable gastric banding, vertical banded gastroplasty, sleeve gastrectomy, intragastric balloons, jejunal bypass, biliopancreatic diversion, and Roux-en-Y gastric bypass.
A significant reduction in BMI is associated with a comparable significant decrease in sleep apnea severity.
Bariatric surgery is recommended for patients with a BMI > 35 kg/m2 and an obesity related concomitant disease or for patients with a BMI > 40 kg/m2.
Currently, 32.9% of US adults and 13% of US children hold a body mass index above 30 kg/m2 and are obese by definition. In Europe, 15.7% of adults and 4% of children and adolescents are obese. In Germany, 22.9% of adults are obese, while the rate is 6.3% for children and adolescents.
Obesity is increasing worldwide. It is estimated that more than 300 million people are obese [269]. Morbid obesity is growing twice as fast as diabetes mellitus prevalence and will overtake it soon [206, 208, 269, 325, 379, 421–423, 557].
The rise in the prevalence of obesity is also associated with increases in comorbidities (for instance, type 2 diabetes, hypertension, obstructive sleep apnea (OSA), heart disease, stroke, asthma, weight bearing degenerative problems, several forms of cancer, depression, etc.), which are responsible for more than 2.5 million deaths per year worldwide [487, 534, 836].
In the case of extreme obesity (BMI ≥ 45 kg/m2) in young adulthood, life expectancy is reduced by 13 years in men and 8 years in women.
The incidence of OSA has been underestimated in obese patients. A 10% increase in body weight in 4 years is associated with a sixfold higher risk of developing OSA [554]. There is an ongoing debate on whether the correlation between obesity and OSA occurs exclusively because of anatomic factors [652, 713].
Obese OSA patients show 42% more fat in their cervical region as compared with normal individuals [484], thereby causing pharyngeal lumen narrowing and resulting in increased risk of developing OSA [634].
A study has shown that bodyweight loss is related to increase of airway transversal diameter, which could result in Apnea Hypopnea Index (AHI) improvement [630].
Furthermore, obesity may also be involved in the genesis of OSA because of metabolic activity of adipose tissue [780].
12.1 Techniques
Bariatric surgical procedures reduce caloric ingestion by modifying the anatomy of the gastrointestinal tract. These operations can be divided into either restrictive, malabsorptive, or combined varieties.
The restriction is usually done by reduction of the gastric reservoir with a narrow outlet to delay emptying. For this purpose, the neo gastric volume is reduced to approximately 20-25 mL.
Examples of restrictive procedure are the adjustable gastric banding, vertical banded gastroplasty, endoluminal vertical gastroplasty, sleeve gastrectomy, or the intragastric balloon.
12.1.1 Adjustable Gastric Banding (Fig. 12.1)
This laparoscopic procedure divides the upper stomach into a small pouch and a large residual region by placing an adjustable band around the fundus. It consists of a soft silicon ring connected to a port system, placed in the epigastric subcutis. Worldwide, the adjustable band is used in 24% of the surgical procedures with a preponderance to European countries [80]. With an estimated rate of 0-0.5%, it has the lowest mortality rate of all bariatric procedures [517]. Long-term results of a 10-year observation period refer to a 13.2% reduction of the initial weight [682]. Short-term studies, however, suggest much higher reduction rates. Complications such as “band slippage,” pouch complications, and decompression of the esophagus might lead to a reoperation rate up to 17% [804].
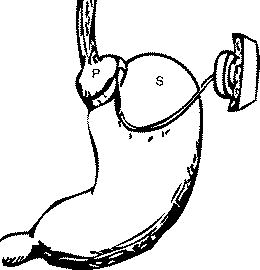
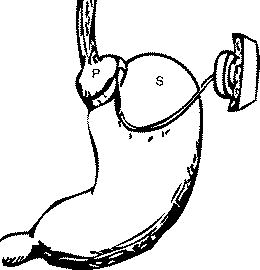
Fig. 12.1
Adjustable gastric banding. P pouch; S stomach
12.1.2 Vertical Banded Gastroplasty (Fig. 12.2)
In this restrictive procedure, the fundus region is divided by a vertical staple line. Additionally, the outlet is wrapped by a band. Long-term weight loss is higher compared to the Adjustable gastric banding [517]. Revision rates of 20-56% mostly affect staple line and band disruption, stomal stenosis, and pouch dilatation [38, 45, 764].
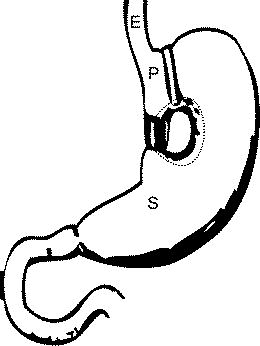
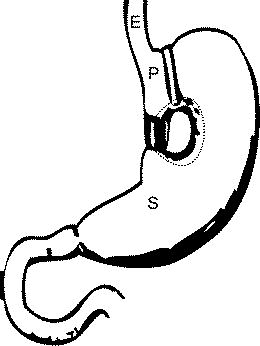
Fig. 12.2
Vertical banded gastroplasty. E esophagus; P pouch; S stomach
12.1.3 Sleeve Gastrectomy
The laparoscopic procedure was originally used as a first-line treatment for super obese patients. It consists of a partial gastrectomy in which the great curvature is stapled off the stomach. As a result of the restrictive technique, the stomach becomes a tube like formation. In addition, ghrelin producing cells of the gastric mucosa are reduced. Compared to adjustable gastric banding, the sleeve gastrectomy results in better hunger control and weight loss. Disadvantage is the irreversible loss of gastric tissue.
12.1.4 Intragastric Balloon
The intragastric balloon (IB) is a temporary device for weight loss in moderate obesity [443]. A balloon is placed endoscopically into the stomach and filled with 500 mL of saline solution. Extensive testing is going on; long-term results are still missing. Nausea, abdominal pain, and balloon migration are adverse effects.
Malabsorptive procedures reduce the caloric intake by shortening the transit time and mucosal surface of the intestine. In general, weight loss with malabsorptive procedures tends to be greater than weight loss with restrictive procedures [80]. Though weight loss is excellent, these procedures are associated with multiple complications such as malnutrition, vitamin, and electrolyte deficiencies, as well as liver failure [141, 241]. Therefore, patients undergoing malabsorptive surgery have to be monitored in a lifetime follow-up.
12.1.5 Jejunal Bypass (Fig. 12.4)
The operation was the first bariatric procedure performed in 1969. It is an end-to-side anastomosis of jejunum to terminal ileum, bypassing most of the small bowel, with the cause of massive malabsorption. Due to its high complication rate and need of revision, the role in up-to-date bariatric surgery is minor.
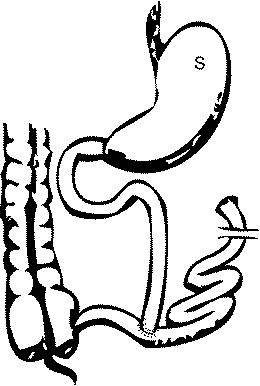
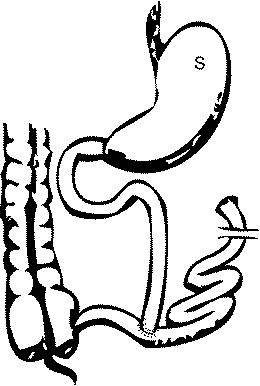
Fig. 12.4
Jejunal bypass. S stomach
12.1.6 Biliopancreatic Diversion (Fig. 12.6)
There are two biliopancreatic diversion (BPD) surgeries: A BPD and a BPD with a duodenal switch (DS) (Fig. 12.3). The BPD consists of a partial gastrectomy and a gastroileostomy. A long segment of the small intestine receives food only; the short common channel receives food and biliopancreatic secretions. The use is limited due to high rates of protein loss, anemia, and stomal ulceration.
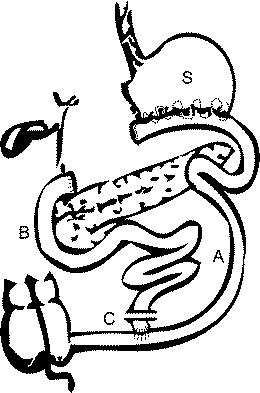
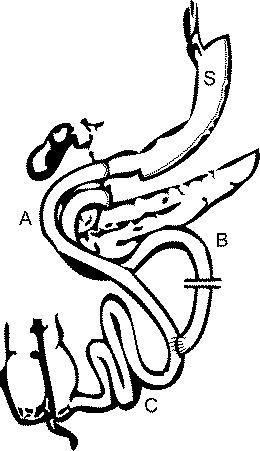
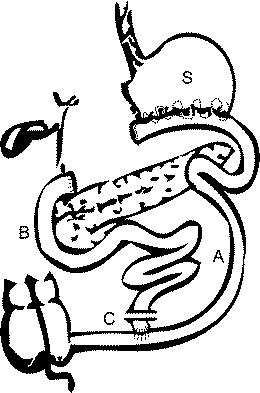
Fig. 12.6
Biliopancreatic diversion. A alimentary limb; B biliopancreatic portion; C common channel; S stomach
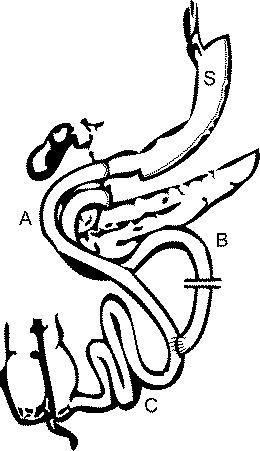
Fig. 12.3
Biliopancreatic diversion with duodenal switch. A alimentary limb; B biliopancreatic portion; C common channel; S stomach
In a BPD with duodenal switch (BPD/DS), a smaller portion of the stomach is removed, the remaining stomach remains attached to the proximal duodenum and is connected in terms of an “alimentary limb” to a 150 cm small intestine segment. The remaining duodenum is connected to the lower part of the small intestine variable at length (“enzyme limb”). The common channel in which food and enzymes encounter measures 100 cm.
These procedures are reserved for patients with super morbid obesity (BMI > 50 kg/m2).
12.1.7 Roux-en-Y Gastric Bypass (Fig. 12.5)
The Roux-en-Y gastric bypass (RYGB) is a typical practice of a combined malabsorptive and restrictive procedure and the most common bariatric operation performed in the US.
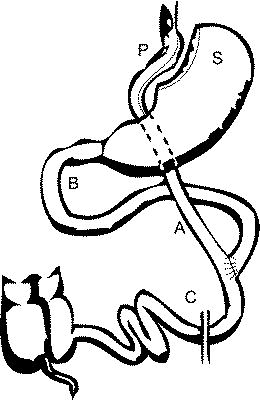
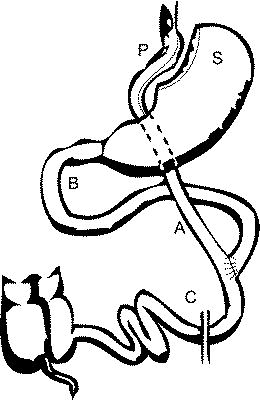
Fig. 12.5
Roux-en-Y gastric bypass (RYGB). A alimentary limb; B biliopancreatic portion; C common channel; P pouch; S. Stomach
The stomach is narrowed by creating a small 25 mL pouch at the fundus region. The smaller stomach is connected directly to the 150 cm measuring “alimentary” jejunal portion of the small intestine, bypassing the rest of the stomach and the upper 50 cm “biliopancreatic” portion of the small intestine. Digestion and absorption occur in the common channel (100-150 cm of length) [73, 111].
Early weight loss is rapid, reaches a plateau usually after 2 years. Long-term reduction of 25% body weight is reported in a 10-year observation study [682].
12.2 Effectiveness for OSA
A metaanalysis has documented the effects of bariatric surgery in 2,399 OSA patients submitted to surgery. For approximately 86% of the cases, OSA was improved or resolved [126]. Continuous positive air pressure (CPAP) treatment could be withdrawn in most patients. As seen in adult patients, pediatric studies generally report good OSA-related outcome after bariatric surgery [342].
The mean BMI changes in OSA patients after bariatric surgeries seem to be similar to patients without sleep apnea [246].
On the other hand, it has to be mentioned that in the long run there are cases of recurrence of sleep apnea without concomitant weight increase, as described in 14 cases 7.5 years after successful weight reduction surgery [563].
The currently still limited polysomnographic data on the effect of bariatric surgery for OSA are listed in Table 12.1.
Table 12.1
Effect of gastric surgery on the severity of obstructive sleep apnea
Author | N | Surgery | Follow-up (month) | BMI pre | BMI post | AHI pre | AHI post | p-Value | EBM |
|---|---|---|---|---|---|---|---|---|---|
Peiser et al. [552] | 15 | GBP (AI) | 2-8 | 48.3 | 33.1 | 82.0 | 15.3 | No data | 4 |
Charuzi et al. [102] | 13 | GBP | 6 | 70.8 | 55.0 | 88.8 | 8.0 | <0.05 | 4 |
Charuzi et al. [101] | 46 | GBP or VBG (AI) | 6 | 47.5 | 32.1 | 58.8 | 7.8 | <0.001 | 4 |
Summers et al. [729] | 1 | VBG | 6 | 54.0 | 37.0 | 40.0 | 5.0 | No data | Casereport |
Sugerman et al. [725] | 40 | GBP or VBG or HG | 69.6 | 56.0 | 40.0 | 64.0 | 26.0 | <0.001 | 4 |
Pillar et al. [563] | 14 | GBP | 90 | 45.0 | 35.0 | 40.0 | 24.0 | <0.05 | 4 |
Scheuller and Weider [647] | 15 | GBP or VBG | 12-144 | 160 kg | 105 kg | 96.9 | 11.3 | <0.0001 | 4 |
Rasheid et al. [591] | 11 | GBP | 3-21 | 62.0 | 40.0 | 56.0 | 23.0 | <0.05 | 4 |
Guardiano et al. [246] | 8 | GBP | 28 | 49.0 | 34.0 | 55.0 | 14.0 | <0.01 | 4 |
Valencia-Flores et al. [761] | 28 | GBP | 13.7 | 56.5 | 39.2 | 53.7 | 8.6 | <0.01 | 4 |
Busetto et al. [85] | 17 | IB | 6 | 55.8 | 48.6 | 52.1 | 14.0 | <0.01 | 4 |
Dixon et al. [154] | 25 | LAGB | 17.7 | 52.7 | 37.2 | 61.6 | 13.4 | <0.01 | 4 |
Fritscher et al. [223] | 12 | GBP | 24.2 | 51.5 | 34.1 | 46.5 | 16.0 | <0.05 | 4 |
Haines et al. [260] | 101 | GBP | 11 | 56.0 | 38.0 | 51.0 | 15.0 | <0.001 | 4 |
All | 331 | 3-144 | 54.51 | 38.39 | 57.91 | 14.80 | C |







