Central Nervous System Infections
Larry E. Davis
key points
Meningitis may be viral, bacterial, or fungal. These different types of meningitis differ in terms of time course, severity, and recommended treatments.
Encephalitis is usually viral. Herpes encephalitis in particular should be treated with acyclovir.
Brain abscesses are usually bacterial and may cause significant symptoms based on mass effect.
Prion diseases (e.g., Creutzfeldt-Jakob) are characterized by rapidly progressive dementia.
Central nervous system (CNS) infections can be caused by viruses, bacteria, fungi, parasites, and prions, but bacteria and viruses are the most common causes. All but one class of human infectious agents (called prions) possess nucleic acid (DNA, RNA, or both) surrounded by a variety of proteins and lipids to create a particle, single cell, or complex cellular organism. Infectious agents enter the body by way of the gastrointestinal tract or respiratory tract or following skin inoculation (animal or insect bite) and set up the initial site of replication in these tissues.
▪ SPECIAL CLINICAL POINT: The majority of organisms then reach the CNS by way of the bloodstream, but occasional organisms reach the brain by way of peripheral nerves or by direct entry through adjacent bone following open skull fracture or from infected mastoid or air sinuses.
Despite the many infections we develop during our lifetimes, organisms rarely reach the brain. For example, transient bacteremias are common following vigorously brushing teeth, yet the bacteria do not cause meningitis. Important protective systems include the reticuloendothelial system (which efficiently removes bacteria and viruses from blood), cellular and humoral immune responses (which destroy organisms from the blood and primary site of infection), and the blood-brain barrier (which prevents entry of organisms into the brain or cerebrospinal fluid [CSF]). Organisms that do enter the brain or CSF from blood do so by infecting endothelial cells of the cerebral blood vessels
(many encephalitis viruses), penetrating the blood-CSF barrier in the meninges or choroid plexus (many bacteria) or occluding small cerebral blood vessels with infected emboli from the blood (brain abscess organisms). Once the invasion has occurred, the brain and CSF have less immune protection than the rest of the body. Normal CSF has about 1/500th the amount of antibody as blood and has few white blood cells (WBCs). Thus, individuals who develop a brain or meningeal bacterial or fungal infection usually die without antimicrobial intervention.
(many encephalitis viruses), penetrating the blood-CSF barrier in the meninges or choroid plexus (many bacteria) or occluding small cerebral blood vessels with infected emboli from the blood (brain abscess organisms). Once the invasion has occurred, the brain and CSF have less immune protection than the rest of the body. Normal CSF has about 1/500th the amount of antibody as blood and has few white blood cells (WBCs). Thus, individuals who develop a brain or meningeal bacterial or fungal infection usually die without antimicrobial intervention.
Inflammation of the meninges or brain is the hallmark of CNS infection. Inflammatory cells may be present in the meninges, in perivascular spaces, or within brain parenchyma such as around an abscess or with encephalitis. The inflammatory monocytes show specific immune activity against the infectious agent.
▪ SPECIAL CLINICAL POINT: The signs and symptoms of a CNS infection depend on the site of the infection—not the organism. The organism determines mainly the time course and severity of the infection.
In general, the time course to develop CNS signs depends on the microorganism class: viruses (hours to 1 day); aerobic bacteria (hours to a few days); anaerobic bacteria, tuberculosis, and fungi (a few days to weeks); parasites and Treponema pallidum (syphilis) (weeks to years).
MENINGITIS
A variety of viral, bacterial, fungal, parasitic, chemical, and neoplastic agents may cause inflammation of the meninges. These patients all have common clinical features:
Early features: Prodromal illness, fever, headache, stiff neck, relative preservation of mental status, no focal neurologic signs, no papilledema.
Later features: Seizures, stupor and coma, cranial nerve palsies, deafness, focal neurologic signs may develop if the etiology is other than viral.
▪ SPECIAL CLINICAL POINT: The time course of the meningitis may give clues as to its etiology. Viral and bacterial meningitis are acute illnesses with symptoms developing over hours to 1 day. Patients with fungal meningitis or tuberculous meningitis develop symptoms over days to 2 weeks.
Common Laboratory Findings
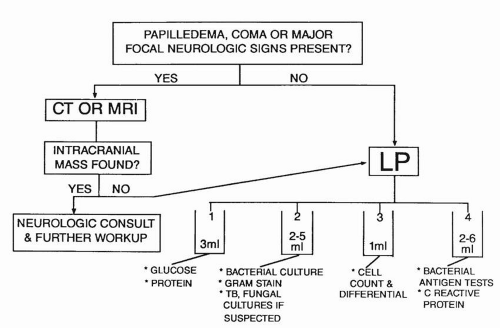
The WBC in blood usually is elevated, as is the erythrocyte sedimentation rate. The CSF examination is the key to the diagnosis of meningitis with ascertainment of the type of infecting agent, establishment of the etiologic agent, and determination of antimicrobial sensitivities (Fig. 24.1). Viral, bacterial, tuberculous, and fungal infections of the meninges have differing CSF profiles (Table 24.1). CSF culture determines the etiology of the infection as well as antimicrobial sensitivities. In general, cultures for bacteria take 1 to 3 days, virus cultures take days to 3 weeks, and tuberculosis and fungi cultures take 1 to 6 weeks. Rapid diagnosis of bacteria can be made by Gram stain of CSF sediment and by testing CSF for common bacterial antigens. The Gram stain will detect bacteria in CSF sediment in more than three fourths of patients with acute bacterial meningitis and often gives clues for initial antibiotic treatment. Latex agglutination antigen tests are commercially available to detect Haemophilus influenzae, Streptococcus pneumoniae, Neisseria meningitidis, and group A beta-hemolytic streptococci. Antigen tests have about the same sensitivity as the Gram stain and may be useful if the patient is already receiving antibiotics. The polymerase chain reaction (PCR) diagnostic test is readily available to rapidly diagnose Mycobacterium tuberculosis, enteroviruses, and herpes simplex virus. Many others are available on a research basis. PCR detects tiny amounts of nucleic acids of these infectious agents in CSF. Advantages of the PCR assay is that it can be performed within hours and can detect nucleic acid from organisms that may be very difficult
to culture. However, the PCR does not give information regarding antimicrobial sensitivities. Thus, the best diagnostic test is still to culture the CSF and blood for an infectious agent and use the isolate to determine antimicrobial sensitivities.
to culture. However, the PCR does not give information regarding antimicrobial sensitivities. Thus, the best diagnostic test is still to culture the CSF and blood for an infectious agent and use the isolate to determine antimicrobial sensitivities.
TABLE 24.1 Spinal Fluid Profiles in CNS Infections | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Viral Meningitis
Enteroviruses (echo viruses and Coxsackie viruses) are the most common cause of viral meningitis. Less common viruses include herpes simplex virus type 2, mumps virus, lymphocytic choriomeningitis, and human immunodeficiency
virus. Typically in viral meningitis, the CSF contains a pleocytosis with predominately lymphocytes, mildly elevated protein, normal glucose, and negative Gram stain of sediment. However, in the first day of the meningitis, there may be a predominance of neutrophils in the CSF. Viruses often can be isolated from CSF early in the meningitis, and PCR analysis of CSF rapidly diagnoses enteroviruses and herpes simplex type 2 viruses. Treatment of most viral meningitis is usually symptomatic and may include analgesics for the headache and antiemetics for nausea and vomiting. In sexually active adults, genital herpes simplex may develop accompanied by meningitis, which can recur for years. If herpes simplex virus is identified in CSF or in herpetic vesicles, use of high-dose acyclovir may shorten the duration of the meningitis.
virus. Typically in viral meningitis, the CSF contains a pleocytosis with predominately lymphocytes, mildly elevated protein, normal glucose, and negative Gram stain of sediment. However, in the first day of the meningitis, there may be a predominance of neutrophils in the CSF. Viruses often can be isolated from CSF early in the meningitis, and PCR analysis of CSF rapidly diagnoses enteroviruses and herpes simplex type 2 viruses. Treatment of most viral meningitis is usually symptomatic and may include analgesics for the headache and antiemetics for nausea and vomiting. In sexually active adults, genital herpes simplex may develop accompanied by meningitis, which can recur for years. If herpes simplex virus is identified in CSF or in herpetic vesicles, use of high-dose acyclovir may shorten the duration of the meningitis.
▪ SPECIAL CLINICAL POINT: Hospitalization for viral meningitis may not be required if the diagnosis is certain, but the patient should be observed at home by a responsible individual. The prognosis of viral meningitis is excellent, and most patients fully recover within 1 to 2 weeks.
Acute Bacterial Meningitis
Both gram-positive and gram-negative aerobic bacteria cause meningitis. S. pneumoniae is the most common bacterium affecting all ages followed by N. meningitidis and H. influenzae. Since the introduction of H. influenzae type B and pneumococcal vaccines to children, the incidence of meningitis in children has decreased dramatically.
▪ SPECIAL CLINICAL POINT: Unlike viral meningitis, patients with bacterial meningitis will progress to death if untreated with antibiotics. Therefore, prompt diagnosis and treatment are essential.
If bacterial meningitis is suspected, the lumbar puncture (LP) becomes an emergency procedure (Fig. 24.1). Although increased intracranial pressure is common in bacterial meningitis, it rarely poses a risk of brain herniation that would prevent an LP. Thus, it seldom is necessary to perform a computed tomography (CT) or a magnetic resonance imaging (MRI) scan before the LP unless the patient is immunosuppressed; is elderly; or presents with coma, focal neurologic signs, or papilledema that places them at increased risk for a focal CNS mass. If there is to be a significant delay before the neuroimaging can be obtained, broad-spectrum antibiotics should be given before the LP. However, one always should obtain a blood culture before administrating the antibiotics. A blood culture is positive in 60% of patients with bacterial meningitis and thus could yield antibiotic sensitivities.
The key to treatment of acute bacterial meningitis is the prompt administration of appropriate antibiotics. General principles involved in the use of antibiotics include the following: (a) the antibiotic should be given early in the clinical course; (b) the bacteria must be sensitive to the antibiotic; (c) the antibiotic must cross the blood-brain barrier and achieve sufficient CSF concentrations to kill the bacteria. Once the diagnosis of bacterial meningitis is made, one should begin treatment with broad-spectrum antibiotics, which later can be modified when antibiotic sensitivities become available. The choice of an antibiotic for initial treatment depends on several factors: age, immune status, and predisposing medical conditions of the patient; results of CSF Gram stain and bacterial antigen tests; knowledge of the types of drug-resistant bacteria in the community; and whether the patient is allergic to any antibiotic. Table 24.2 gives common initial antibiotic regimens, but one should check references such as the Medical Letter for the latest recommendations.
Neurologic injury in bacterial meningitis occurs in up to 20% of patients. Mechanisms of cerebral injury include meningeal vasculitis causing spasm or thrombosis of meningeal arteries, arterioles, veins, or venules. The consequence is ischemia to the underlying brain resulting in infarctions. Second, a variety of toxins are produced within the CSF by the bacteria and inflammatory cells such as endotoxin, reactive oxidizing chemicals from neutrophil granule
release, and cytokines released from mononuclear cells that cross the pial barrier to reach cerebral gray matter causing neuronal necrosis. The third mechanism develops from inadequate cerebral arterial perfusion producing global cerebral ischemia. Cerebral perfusion pressure results from systemic blood pressure minus intracranial pressure. Increased intracranial pressure can result from increased brain water from the first two mechanisms, increased CSF pressure due to obstructive hydrocephalus and from increased cerebral blood from dilated meningeal arteries and veins responding to the inflammation. Systemic hypotension can develop from shock, hypovolemia, dehydration secondary to fever and vomiting, and inadequate fluid replacement in the hospital. Meningeal bacteria do not readily penetrate the pia mater and invade the brain. However, interactions between meningeal bacteria and host result in meningeal inflammation; vascular injury; disruption of the blood-brain barrier; vasogenic, interstitial, and cytotoxic edema; and disruption of normal CSF flow. At present, corticosteroids have been shown to have a modest benefit in preventing neurologic morbidity in children and adults. Dexamethasone (0.15 mg/kg intravenously in children every 6 hours and 10 mg in adults every 6 hours for 2 to 4 days) commonly is administered as early as possible. To minimize risks from administering corticosteroids, dexamethasone should be given only when the illness and CSF findings are highly suggestive of community acquired bacterial meningitis in an immunocompetent patient without contraindications for steroid administration such as a recent GI bleed.
release, and cytokines released from mononuclear cells that cross the pial barrier to reach cerebral gray matter causing neuronal necrosis. The third mechanism develops from inadequate cerebral arterial perfusion producing global cerebral ischemia. Cerebral perfusion pressure results from systemic blood pressure minus intracranial pressure. Increased intracranial pressure can result from increased brain water from the first two mechanisms, increased CSF pressure due to obstructive hydrocephalus and from increased cerebral blood from dilated meningeal arteries and veins responding to the inflammation. Systemic hypotension can develop from shock, hypovolemia, dehydration secondary to fever and vomiting, and inadequate fluid replacement in the hospital. Meningeal bacteria do not readily penetrate the pia mater and invade the brain. However, interactions between meningeal bacteria and host result in meningeal inflammation; vascular injury; disruption of the blood-brain barrier; vasogenic, interstitial, and cytotoxic edema; and disruption of normal CSF flow. At present, corticosteroids have been shown to have a modest benefit in preventing neurologic morbidity in children and adults. Dexamethasone (0.15 mg/kg intravenously in children every 6 hours and 10 mg in adults every 6 hours for 2 to 4 days) commonly is administered as early as possible. To minimize risks from administering corticosteroids, dexamethasone should be given only when the illness and CSF findings are highly suggestive of community acquired bacterial meningitis in an immunocompetent patient without contraindications for steroid administration such as a recent GI bleed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree