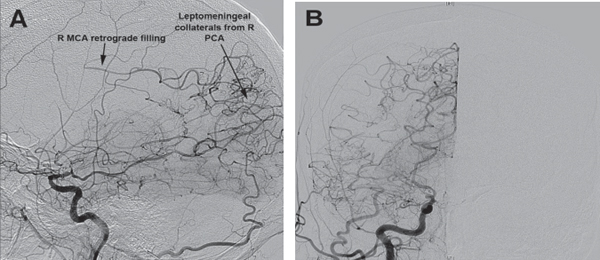
55 When is carotid endarterectomy (CEA) indicated for symptomatic carotid stenosis as opposed to medical management alone? Carotid endarterectomy is indicated for symptomatic stenosis >50% and <99%,1–4 provided that the operative morbidity and mortality is <6%. In symptomatic carotid stenosis of 70 to 99%, CEA resulted in a 9 to 26% reduction in 2-year stroke risk compared with best medical management alone. A marginal but statistically significant reduction was seen in patients with symptomatic carotid stenosis of 50 to 70%.1 When is CEA indicated for asymptomatic carotid stenosis as opposed to medical management alone? CEA is indicated for asymptomatic stenosis of 60 to 99%, provided that surgical morbidity and mortality is <3%. The Asymptomatic Carotid Atherosclerosis Study (ACAS) has shown a 5 to 11% reduction in 5-year stroke risk with CEA and medical management compared with medical management alone in these patients. Better reduction was seen in males than in females.5–8 When is carotid angioplasty or stenting indicated as opposed to CEA? Not well established due to a lack of data.9 Angioplasty may be considered in patients with severe vascular or cardiac comorbidities (e.g., congestive heart failure, recent myocardial infarction, unstable angina) or those who may be at higher risk for complications following CEA (age >80 years, history of radiation therapy to neck, previous CEA with recurrent stenosis, high lesion, contralateral carotid occlusion).10–12 What is the most common operative positioning and approach? Anterolateral cervical approach with patient supine and neck slightly extended and rotated away from the operative side The incision should not extend closer than 1 cm to the mandible to prevent damage to what nerve during retraction? The facial nerve (marginal mandibular branch) Retractors poorly placed below the platysma can damage what nerve lying between the esophagus and trachea? Cranial nerve (CN) X (recurrent laryngeal branch) Which structures are important to identify during CEA dissection? • Common facial vein (crosses over the carotid bifurcation and must be ligated and divided) • Internal jugular vein • Vagus nerve (CN X) • Ansa cervicalis (aka ansa hypoglossi) travels superficial to the ICA • Hypoglossal nerve (CN XII) (often arises in vicinity of common facial vein) • Branches of the common carotid artery In what order is the carotid division clamped during CEA? Most common order: ICE (internal, common, external) In what order are the vessel clamps removed during CEA? External, common, internal What are some of the complications associated with CEA? • Failure of arterial closure (hematoma, dysphagia, hoarseness, difficulty breathing, tracheal deviation) • Stroke (5% incidence after CEA13 and TIA) • Seizures • Restenosis (25% within 1 year14) • Normal perfusion pressure breakthrough (aka cerebral hyperperfusion syndrome) may present as ipsilateral headache and eye pain15 • Hoarseness (due to laryngeal edema or recurrent laryngeal nerve damage) • Cranial nerve injury (CNs VII, X, and XII) (incidence 8 to 10%16) What are some of the most important components of the postoperative management of CEA patients? Physical exam: pronator drift, tongue deviation, vocal-cord paralysis, pupillary changes (Horner’s syndrome), lip depressor strength (damage to mandibular branch of VII may produce weakness) History: headache, eye pain, dysphagia, difficulty breathing, hoarseness What is arterial dissection? Extravasation of blood between layers of the arterial wall. This has the potential to expand and narrow or occlude the vessel lumen. What are the characteristics of cerebral arterial dissections? Dissection is most commonly subintimal. Extra-cranial vessels typically dissect at the media or between the media and the adventitia. How are dissections classified? • Spontaneous • Traumatic (more common) Where do intracranial dissections most commonly occur? Vertebral >> basilar > internal carotid > MCA > ACA, PCA, PICA What diseases impart an elevated risk of spontaneous arterial dissection? • Fibromuscular dysplasia (15% incidence)17 • Marfan syndrome • Saccular aneurysm • Vasculitis (Takayasu’s, polyarteritis nodosa [PAN], syphilitic arteritis) • Moyamoya disease18 How do spontaneous dissections present? Vertebral artery: neck pain, generalized severe headache, stroke, TIA, SAH ICA: ipsilateral headache (often orbital), and incomplete Horner’s syndrome (aka oculosympathetic palsy; ptosis and miosis without anhidrosis), bruit What radiographic sign assists with the diagnosis of arterial dissection? Angiogram or CTA: “String sign” (irregular luminal stenosis over arterial segment) or “double lumen sign” (intramural false lumen with intimal flap in addition to the true vessel lumen) MRI/MRA: “crescent sign” on T2-weighted imaging (bright signal in ICA wall due to hematoma) What mechanism is responsible for the majority of posttraumatic carotid and vertebral dissections? Neck hyperextension with lateral rotation (e.g., motor vehicle accidents), cervical manipulation (e.g., therapeutic spinal manipulation) or direct blow What is the most common site for vertebral artery dissection? Between C2 and occiput What is the most common site for carotid artery dissection? 2 cm distal to the ICA origin Describe the protocol for conservative management of arterial dissections. If no bleeding occurs, heparinize the patient for 1 to 2 weeks, then prescribe Coumadin for up to 6 months. Repeat the angiogram to assess healing prior to suspending treatment. When is intervention indicated? Dissections presenting with SAH, intradural dissections, persistent symptoms, angiographically progressive dissections, or if conservative management fails What are the treatment options for carotid dissections? • Endovascular stent • Graft interposition • Extracranial-intracranial bypass • Carotid ligation (rare) What is moyamoya disease? A disease of unknown etiology with a poor prognosis19 characterized by intimal thickening without inflammation and progressive bilateral narrowing of the carotid arteries with subsequent development of a capillary collateral network resembling a “puff of smoke” (moyamoya in Japanese) Which ethnic groups are most commonly affected? Japanese, Haitian, and Hispanic populations How does moyamoya disease commonly present? Headache, seizures, focal neurological deficit, hemorrhage (more common in adult presentation), ischemic stroke (more common in pediatric presentation)20 What is the preferred imaging modality for diagnosis? Conventional digital subtraction angiography (DSA) is the gold standard, and it also facilitates treatment planning (identification of donor vessels for revascularization procedures).21 What are the six angiographic stages (“Suzuki stages”) of moyamoya disease? Stage I: stenosis (typically bilateral) of suprasellar ICA Stage II: early development of collateral (moyamoya) vessels at the brain base; ACA, MCA, and PCA are often dilated Stage III: increased ICA stenosis and moyamoya vessel prominence Stage IV: occlusion of the entire circle of Willis and PCAs, moyamoya vessels begin to diminish, extracranial collaterals appear Stage V: further progression of findings seen in stage IV Stage VI: complete absence of major cerebral arteries and moyamoya vessels22 Fig. 55.1 Lateral (A) and anteroposterior (B) digital subtraction angiography views of a patient with moyamoya disease. The right internal carotid artery is completely occluded immediately distal to the anterior choroidal artery. Robust leptomeningeal collaterals originating from the right posterior cerebral artery can be seen filling the right middle cerebral artery in retrograde fashion.
Cerebro-Occlusive Disease
55.1 Carotid Arterial Stenosis
55.2 Arterial Dissection
55.3 Moyamoya Disease
Cerebro-Occlusive Disease
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






