Cervical Degenerative Disk Disease: Overview and Epidemiology
Andrew J. Schoenfeld
Christopher M. Bono
The terms “cervical degenerative disease” or “cervical spondylosis” broadly refer to normal age-related changes that may occur within the cervical spine. Degenerative changes in the cervical spine can be identified in the majority of individuals beyond the fifth decade of life, yet most are asymptomatic. Symptoms attributable to cervical degeneration may be present in as much as 5% of the general population at any time (1, 2 and 3) and exist along a wide spectrum, from axial neck pain to cervical radiculopathy and spondylotic myelopathy. Multiple conditions may also be present simultaneously with overlapping symptomatologies.
Due to the high prevalence of cervical degeneration within the adult population, a systematic approach to complaints attributable to this condition is warranted. Findings from a focused history and physical examination can be correlated with the results of imaging studies, including plain films and advanced modalities, such as computed tomographic or magnetic resonance imaging (MRI). A comprehensive understanding of the natural history, pathoanatomy, and indications for treatment is necessary in order to fashion an appropriate treatment algorithm for any patient.
It is the authors’ hope that this chapter will serve as a general guide to the broad scope of cervical degenerative disease with an emphasis on epidemiology, pathophysiology, and natural history.
HISTORICAL BACKGROUND
Paleopathologic examinations of skeletal remains from the ancient and medieval periods have revealed that the cervical degenerative process has not changed substantially over the last 1.5 millennia (4, 5, 6 and 7). While certain functions of the spinal cord were known to the ancient Egyptians, it was not until the time of Herophilus of Chalcedon (fourth century BCE) that the origin of nerves was traced to the spine (6,7). The Byzantine physician, Paul of Aegina, understood the pathoanatomy enough to recommend cervical decompression via laminectomy in the setting of cord compression, but limitations in operative techniques, as well as surgical technology, prevented widespread application of this maxim until the modern period (7).
It was not until the 19th century that associations were made between degenerative changes in the cervical spine and neurologic symptoms in the arms or legs (8). In 1928, Stookey (9) first reported cervical cord and nerve root compression from the presence of “soft” and “hard” disk herniations. He would subsequently follow this landmark article with another that highlighted three different clinical syndromes resultant from cervical disk herniations (10).
By the mid-1950s, a more modern understanding of the spectrum of cervical degenerative disorders, and their disparate etiologies, had been attained. In 1947, the work
of Brain (11) differentiated the symptoms encountered in acute disk herniations from those found in spondylotic radiculopathy. Brain et al. (12) also first presented the concept of cervical spondylotic myelopathy in a series of 45 patients in 1952. The pathophysiology and etiology of cervical spondylosis was elaborated in the works of Taylor (13) and Payne and Spillane (14), while the scope of cervical degeneration was further defined by Friedenberg et al. (15). The work of Clarke and Robinson (16) contributed to a more thorough understanding of the underlying pathology responsible for spondylotic myelopathy.
of Brain (11) differentiated the symptoms encountered in acute disk herniations from those found in spondylotic radiculopathy. Brain et al. (12) also first presented the concept of cervical spondylotic myelopathy in a series of 45 patients in 1952. The pathophysiology and etiology of cervical spondylosis was elaborated in the works of Taylor (13) and Payne and Spillane (14), while the scope of cervical degeneration was further defined by Friedenberg et al. (15). The work of Clarke and Robinson (16) contributed to a more thorough understanding of the underlying pathology responsible for spondylotic myelopathy.
At approximately the same time as Stookey’s work regarding cervical spondylosis, Mixter and Barr (17) were describing the first successful surgical interventions for relief of symptoms caused by degenerative disease. These physicians advocated for a posterior approach to decompression. As the understanding of cervical anatomy continued to advance, however, anterior approaches for decompression and fusion in the cervical spine were described by several investigators (18, 19 and 20). With the advent of cervical laminoplasty techniques in the early 1980s (21,22) and total disk arthroplasty in the late 1990s (23, 24 and 25), the current armamentarium of surgical intervention for the treatment of cervical spondylosis was completed.
The goals of all operative interventions are to limit further disability and, wherever possible, reverse radicular or myelopathic symptoms (26). Such goals are achieved through the decompression of the spinal cord and nerve roots, as well as stabilization of the spine when instability appears to be contributing to the pathology or is the byproduct of decompression.
PATHOPHYSIOLOGY OF CERVICAL DEGENERATION
There is no true consensus regarding the exact pathophysiologic mechanisms leading to cervical degenerative disk disease, although a number of postulates have been advanced. Modern thought considers cervical disk degeneration to be a normal part of aging, although factors such as trauma, repetitive motion, and certain occupations (27, 28, 29, 30 and 31) may accelerate the condition. No single factor likely triggers the degenerative process. Rather, multiple aspects of normal aging contribute over time to cervical spondylosis. While it is difficult to distinguish pathologic processes from the effects of normal aging, a working diagnosis of cervical degenerative disk disease may include early, extensive, or symptomatic degeneration (26,32, 33 and 34).
As individuals reach the third decade of life, there is often a reduction in the peripheral blood supply surrounding the intervertebral disk (34). This, combined with sclerosis of the vertebral end plates, leads to impaired nutrition and waste diffusion for the cells within the intervertebral disks (34,35). Such environmental stresses cause the cells to become senescent and begin secreting less proteoglycan (35,36).
Cellular senescence and reduced levels of proteoglycan result in decreased hydration of the nucleus pulposus, which, in turn, leads to altered structural and load-bearing properties of the disk. Transfer of loads to the annulus fibrosus causes fissuring and a loss of elasticity, which contributes to disk collapse and potentiates herniation. Loss of disk height also causes increased motion and wear at the posterior facet joints, culminating in facet arthropathy and hypertrophy of the posterior ligamentous structures, including the ligamentum flavum. Inflammation and excessive motion produce osteophytic complexes at the disk margins, uncovertebral joints, and the facets. Osteophytes, herniated disk material, or hypertrophic soft tissue structures can all exert pressure on the nerve roots or spinal cord, leading to symptoms of radicular pain or myelopathy.
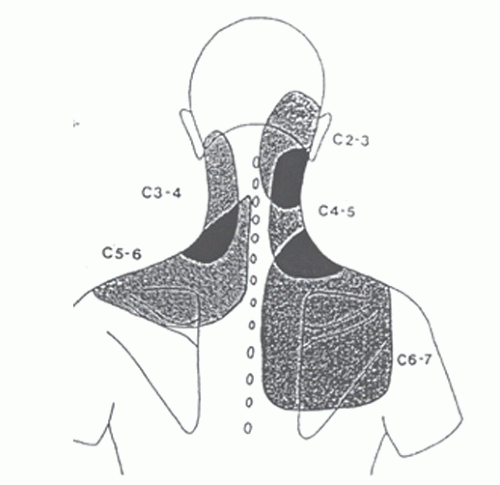
Degeneration of the cervical spine may manifest as only neck pain if no impingement of the spinal cord, or nerve roots, is present. Inflammation of a cervical nerve root due to extrinsic compression can result in discrete patterns of pain in the occipital region, posterior neck, or shoulders or radicular pain in the arms (Fig. 67.1). Similar symptoms of nerve root irritation also occur due to the inflammation produced by cytokines, such as interleukins, tumor necrosis factor-alpha, and substance P that are released from a herniated nucleus pulposus (Table 67.1) (34,37,38). Mechanical compression of the spinal cord, perhaps in
the setting of an already congenitally narrowed canal, can trigger vasospasm and cord ischemia (39). Animal models have demonstrated that myelopathic symptoms develop beyond a threshold of 40% spinal canal compromise (33).
the setting of an already congenitally narrowed canal, can trigger vasospasm and cord ischemia (39). Animal models have demonstrated that myelopathic symptoms develop beyond a threshold of 40% spinal canal compromise (33).
TABLE 67.1 Inflammatory Mediators of Radicular Pain | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Degenerative changes can be present at all levels of the cervical spine but are most commonly encountered at C5-C6, followed by C6-C7 and C4-C5.(34) Anterior cord compression usually occurs from herniated nucleus pulposus (“soft disk herniation”), bulging desiccated disks (“hard disk herniation”), end plate osteophytes, and ossified posterior longitudinal ligament. Posterior impingement often results from infolding of the ligamentum flavum and facet arthropathy. In many instances, anterior and posterior processes are both involved in narrowing the spinal canal and impinge on the cord in a so-called pincer effect.
HERNIATION OF THE NUCLEUS PULPOSUS
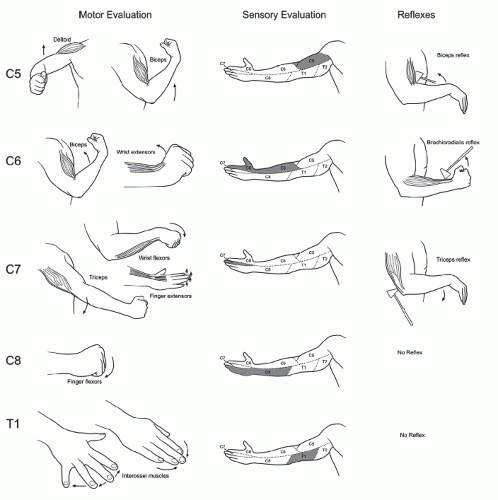
In some younger individuals, tears in the annulus fibrosus may precede desiccation of the nucleus pulposus. In such instances, prolapse of disk contents into the spinal canal, or foramen, can occur analogous to disk herniation in the lumbar spine. Chemical mediators released with the nuclear tissue (38), as well as mechanical displacement of the cervical nerve root, produce symptoms of radiating pain and sensory or motor dysfunction (Fig. 67.2). In a review of 736 patients with cervical radiculopathy, Henderson et al. (40) reported that 99.4% of patients had radicular arm pain, 85.2% had sensory abnormalities, 68% exhibited motor dysfunction, 9.7% had chronic headaches, and 1.3% complained of cervical angina (left-side chest and arm pain).
C5-C6 is the level most likely to exhibit a disk herniation (41), and the C6 nerve root is usually affected. A review of 561 patients with cervical radiculopathy revealed the C7 nerve root to be the most commonly involved, however (42). Deficits on physical examination can be attributed to the herniated level in 80% of cases (40). Radicular symptoms may be exacerbated during Valsalva maneuvers or the performance of Spurling’s test (37,43). Relief of radicular pain can often be achieved by Davidson’s ipsilateral shoulder abduction maneuver (44). Shoulder abduction reduces tension and shifts the nerve root away from sites of compression. Additionally, constricted epidural veins may be decompressed, contributing to symptom resolution (32).
CERVICAL SPONDYLOSIS: AXIAL NECK PAIN AND RADICULOPATHY
In more advanced stages of cervical degeneration, reduction in disk height, disk bulging, osteophyte formation, and facet arthrosis can impinge on exiting nerve roots, producing symptoms of radiculopathy. In the absence of frank compression, such degenerative changes may be responsible for symptoms of axial neck pain.
Branches of the sinuvertebral nerve innervate the intervertebral disk while other nociceptive fibers are present in the facet joints and capsule (45,46). Investigations utilizing provocative diskography and facet joint injections have demonstrated the potential for both intervertebral disks and facet joints to produce characteristic patterns of axial neck pain (47,48). Subaxial pain may also be due to muscle and ligamentous strain that results from attempts at splinting painful degenerative segments.
Stenosis within the neural foramina of the subaxial spine leads to radicular symptoms similar to those produced by a herniated nucleus pulposus, including pain, and sensory or motor deficits. Degenerative changes in the upper cervical spine produce suboccipital pain with radiation into the neck or ear (49). Symptoms in spondylotic radiculopathy often appear in a more gradual manner than those attributable to “soft disk herniations.” Patients with spondylotic radiculopathy are also more likely to have bilateral symptoms, as well as symptoms at multiple cervical levels (41,50). The differential diagnosis of cervical radiculopathy can include epidural abscess, rotator cuff/shoulder abnormalities, peripheral nerve entrapment syndromes, brachial plexopathy, herpes zoster, cardiac ischemia, or thoracic outlet syndrome (33,37).
CERVICAL SPONDYLOTIC MYELOPATHY
Prolonged compression of the central spinal canal leads to symptoms of cervical spondylotic myelopathy, including gait imbalance or ambulatory difficulty, loss of fine motor coordination, sensory disturbances in the extremities, and urinary difficulties (26,33,51). In the Asian population, myelopathy is most often attributable to stenosis caused by ossification of the posterior longitudinal ligament (OPLL) (52).The histopathology of myelopathy includes prolonged compromise of the microvasculature in the anterior spinal cord, causing axonal demyelinization, cell necrosis, scarring, and cystic cavitation in the gray matter (53).
Myelopathy is the most common cause of spinal cord dysfunction in patients over the age of 55 (26,51). Symptoms of cervical myelopathy usually present in the sixth decade of life and are most common at C5-C6, followed by C4-C5 and C6-C7. Symptoms can vary on an individual basis and may be subtle or stable for long periods of time. Physical examination often reveals positive upper-motor neuron, or long tract findings, including Hoffman and Babinski signs. Intrinsic wasting in the hand and the small finger escape sign can also be noted. Some individuals describe the Lhermitte’s sign: the sensation of “electric shocks” in the extremities produced by neck flexion. In their study of 62 patients with cervical myelopathy, Crandall and Batzdorf (54) found that only 38% had radicular symptoms and less than 50% complained of neck pain. Only 27% of patients exhibited the Lhermitte’s phenomenon.
Many patients remain asymptomatic, however, and exhibit no physical exam findings. Referral to a spine specialist in these instances is often due to incidental findings of myelomalacia on MRI. Delayed diagnosis of myelopathy can occur due to the fact that the condition may be painless and symptoms might be ignored by patients until they become severe. The classic “stepwise progression” exhibited by the condition can evolve over years (16,55), but myelopathy can also present as catastrophic quadriparesis within a matter of hours (32). In their review of 120 patients with cervical myelopathy, Clarke and Robinson (16) reported that 75% of patients exhibited stepwise deterioration after long periods of stable neurologic function. Twenty percent of patients had slow steady progression of their symptoms without stabilization, and 5% presented a rapid deterioration in function (16).
TABLE 67.2 Nurick Classification of Disability due to Cervical Myelopathy | |||||
|---|---|---|---|---|---|
|
Five categories of cervical spondylotic myelopathy were described by Crandall and Batzdorf (54) in 1966. The most common manifestation is the transverse lesion syndrome, which involves the corticospinal and spinothalamic tracts. Symptoms include upper motor neuron findings, weakness, and lower extremity spasticity. Central cord syndrome results from compression of the central gray matter and leads to motor and sensory involvement in the upper extremities with painful dysethesias. The lower extremities are usually spared. Brown-Sequard syndrome, similar to the incomplete spinal cord injury of the same name, manifests as ipsilateral loss of motor function with contralateral pain and temperature deficits. This myelopathic syndrome has the best prognosis for recovery. Motor system syndrome is caused by pure anterior compression on the anterior horn cells and corticospinal tracts. Symptoms of this condition are limited to motor weakness and gait abnormalities. Brachialgia cord syndrome is a combination of radicular and myelopathic symptoms. Patients have radicular pain in the upper extremities combined with weakness and lower extremity spasticity.
Ferguson and Caplan (56) subsequently divided cervical spondylotic myelopathy into four, presumably simpler, classifications. These include medial syndrome, which consists primarily of long tract symptoms; lateral syndrome, which is radicular in nature; combined medial and lateral syndrome; and vascular syndrome, a rapidly progressive form of the disease that results from cord ischemia. In the Ferguson and Caplan system, combined medial/lateral syndrome was the most commonly encountered form of myelopathy. The ambulatory abnormalities encountered in myelopathy have also been classified in the work of Nurick (Table 67.2) (57).
CLASSIFICATION OF CERVICAL DEGENERATIVE DISK DISEASE
While a number of authors have sought to categorize the myelopathic manifestations of cervical spondylosis, attempts to classify the degenerative appearance of the cervical spine did not appear until recently. The ideal
classification scheme should provide a comprehensive, yet simple, means of categorization with the goals of facilitating physician communication and informing treatment. To this effect, Hilibrand et al. (58) described a relatively simple three-stage grading scale based on radiographic signs of degeneration. These authors relied on the presence of osteophytes, as well as reduction of disk height, to categorize disease severity.
classification scheme should provide a comprehensive, yet simple, means of categorization with the goals of facilitating physician communication and informing treatment. To this effect, Hilibrand et al. (58) described a relatively simple three-stage grading scale based on radiographic signs of degeneration. These authors relied on the presence of osteophytes, as well as reduction of disk height, to categorize disease severity.
While Hilibrand et al. based their rating scale on radiographic imaging, most subsequent classifications have attempted to categorize cervical degeneration using MRI. Christe et al. (59) proposed a system where degenerative grade was determined by the sum of four factors visible on MRI, including presence of osteophytes and disk space narrowing, disk prolapse, annular tears, and loss of disk signal intensity. At the same time, Kolstad et al. (60) devised a classification based on three factors: nuclear signal intensity, disk prolapse, and bone marrow signal of the adjacent vertebral bodies. The system of Kolstad et al. ultimately included 12 comprehensive categories (A to L). The classification itself is quite complex and has demonstrated only moderate interobserver reliability (60,61). Additionally, the systems proposed by Christe et al. and Hilibrand et al. have not been tested for validity or reproducibility (58,59).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree