35 Cervical Laminectomy with or without Fusion
I. Key Points
– Conservative therapy is the initial, primary treatment modality for neck pain and/or radiculopathy caused by degenerative cervical spine disease.
– The surgical goal should be to decompress the neural elements and, when clinically warranted, provide stabilization via instrumentation/fusion.
– Focal pathology may be better treated via anterior cervical approaches or posterior foraminotomy.
II. Indications
– Multilevel degenerative disc disease causing cervical stenosis and myelopathy
– Cervical stenosis due to diffuse ossification of the posterior longitudinal ligament (OPLL)
– Epidural abscess
– Tumor
III. Technique
– Place patient in prone position.
• Awake, fiberoptic intubation may be necessary in cases of severe stenosis or instability.
– Mayfield head fixation or the use of skull tongs to apply 5 to 10 lb of inline cervical traction is optional.
– Localize with fluoroscopy and make appropriate-length midline incision.
– Even if localization is not needed (e.g., for long occipital-cervical incisions), it is advisable to obtain at least a lateral fluoroscope shot pre-incision with patient in the prone position to (1) appreciate alignment and (2) determine if lower cervical levels can be visualized.
– Dissecting down to the spinous processes in the midline avascular plain maintains the integrity of posterior neck muscles and minimizes bleeding.
– Perform subperiosteal dissection to expose the spinous processes, the lamina, and the lateral masses of the desired levels.
• It may be desirable to reduce the monopolar cautery level as dissection is carried laterally toward the edge of the lateral mass to avoid denervation/atrophy of neck muscles.
– Perform the posterior cervical laminectomy.
• One technique is to use an AM-8 drill bit to create bilateral troughs at the laminar–lateral mass junction and remove the posterior elements “en bloc.”
 Advantage: no need to place instrument under the lamina and risk cord compression
Advantage: no need to place instrument under the lamina and risk cord compression
 Disadvantage: requires proficiency with the drill and places the lateral mass at risk if the troughs are too lateral
Disadvantage: requires proficiency with the drill and places the lateral mass at risk if the troughs are too lateral
• A second technique is to use a combination of Leksell and Kerrison instruments (manual laminectomy).
 Advantage: technique more familiar as it is widely used in the lumbar spine
Advantage: technique more familiar as it is widely used in the lumbar spine
 Disadvantage: potential risk of neural injury with instruments placed under lamina in severe stenosis
Disadvantage: potential risk of neural injury with instruments placed under lamina in severe stenosis
• The third technique is to use a footplate craniotome to create bilateral troughs (no significant advantage and may carry higher risks in authors’ opinion).
– Perform cervical lateral mass fixation (if necessary) (Fig. 35.1).
• Magerl technique
 The lateral mass is divided into quadrants.
The lateral mass is divided into quadrants.
 The entry point is at the superior medial quadrant and the trajectory is toward the superior lateral quadrant (“up and out”) (Fig 35.2).
The entry point is at the superior medial quadrant and the trajectory is toward the superior lateral quadrant (“up and out”) (Fig 35.2).
 Usually achievable for C3-C6
Usually achievable for C3-C6
• Roy-Camille technique
 The entry point is at the midpoint of the lateral mass.
The entry point is at the midpoint of the lateral mass.
 The trajectory is 10 degrees lateral in the same axial plane.
The trajectory is 10 degrees lateral in the same axial plane.
 Typically employed at the C7 level
Typically employed at the C7 level
• If C7 is included in the fixation, pedicle screws are typically used.
 A laminotomy to palpate the medial edge of the pedicle is useful.
A laminotomy to palpate the medial edge of the pedicle is useful.
 The entry point is in line with lateral mass entry points at superior levels.
The entry point is in line with lateral mass entry points at superior levels.
 Slight medial angulation is necessary to enter and traverse the pedicle.
Slight medial angulation is necessary to enter and traverse the pedicle.
• Lateral mass screw size is typically 3.5 or 4.0 mm by 12 to 16 mm.
• C7 pedicle screw size is typically 3.5 or 4.0 mm by 16 to 24 mm.
– Insert appropriate-length rods and secure with set screws/caps.
• Ensure proper application of anti-torque when securing caps to prevent lateral mass fracture/screw pullout.
• Decortication is performed using a high-speed drill; ideally, decorticate facets.
• Bone graft material (autograft plus carrier) is placed along the lateral mass edges bilaterally.
• Ensure that no graft material is left within the canal or foramen.
– Place subfascial drain and close muscle, fascia, and skin layers.
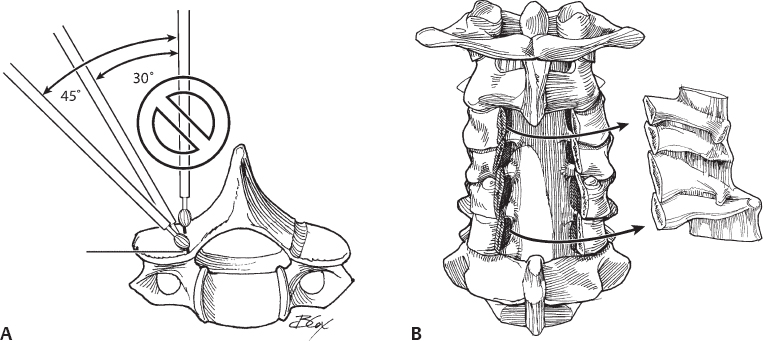
Fig. 35.1 Laminectomy. (A) The burr must be directed approximately 30 to 45 degrees in the sagittal plane to avoid burring into the facet joint. Doing so may risk loss of orientation and cause one to burr too deeply, endangering the dural sac or spinal cord. (B) En bloc removal of laminae. (From Vaccaro AR, Albert TJ, Spine Surgery: Tricks of the Trade 2nd ed, Thieme; pg. 6, Fig. 2.2B,C.)
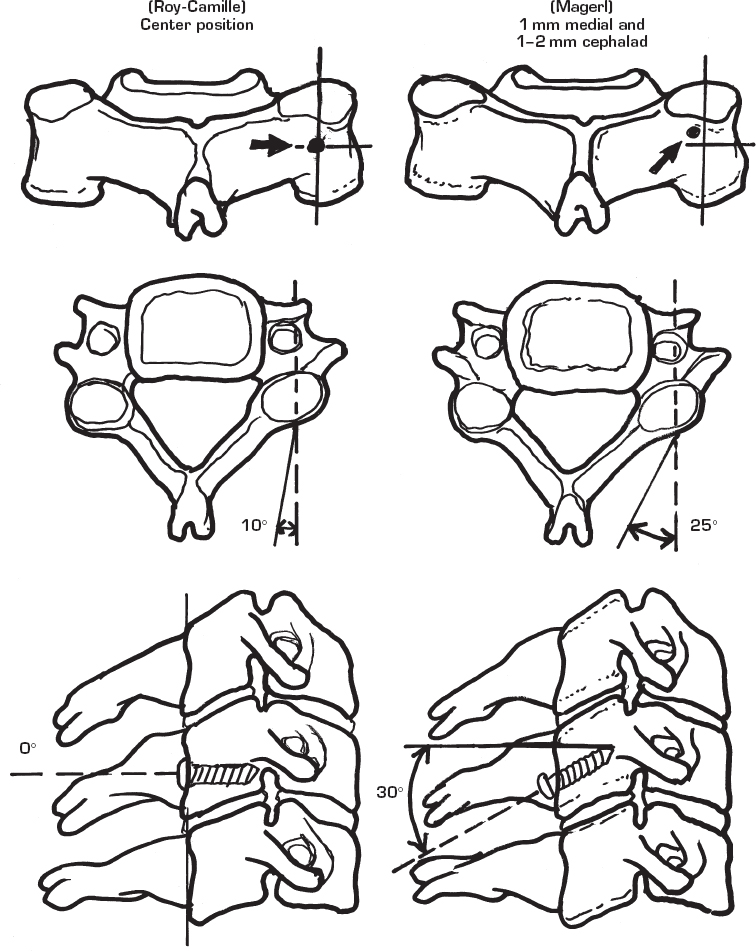
Fig 35.2 The Magerl and Roy-Camille techniques for placement of lateral mass screws in the subaxial cervical spine.
IV. Complications
– Cerebrospinal fluid (CSF) leak
• Attempt primary repair using nonabsorbable suture.
• Alternatively, cover with Gelfoam (Pfizer, New York) and/or fibrin glue.
– Nerve root injury
• May result either directly during foraminotomy or screw placement or indirectly from stretching/recoiling
• C5 palsy: Incidence and etiology not well understood. May be due to traction, given that the C5 root is shortest. Often transient but noticeable immediately post–cervical laminectomy.
– Vertebral artery injury
• Typically results from misplaced lateral mass screw
• Screw should remain in place and postoperative angiogram used to delineate type of injury (e.g., occlusion, dissection).
– Wound infection
V. Postoperative Care
– Mobilize early with (typically in case of trauma) or without cervical collar.
– Obtain postoperative (PO) upright anteroposterior (AP)/lateral C-spine x-rays.
– Remove drain when output becomes less than 50 ml per 8-hour shift (typically PO day 1 or 2).
– Discharge home when patient meets discharge criteria.
VI. Outcomes
– Class III evidence shows that 70 to 95% of patients show post-operative neurologic improvement after cervical laminectomy and fusion for myelopathy.1
VII. Surgical Pearls
– Preoperative cervical kyphosis and loss of lordosis are relative contraindications to posterior laminectomy without instrumentation.
– Focal disc bulges/herniations should be treated via anterior approaches.
– Positioning multiple lateral mass entry points in line facilitates rod placement (often the frustrating step of the procedure).
Common Clinical Questions
1. In the Magerl technique why is the trajectory of lateral mass screws “up and out”?
2. Which nerve root is most prone to indirect injury during posterior cervical laminectormy?
3. Why is preoperative cervical spine alignment an important consideration?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







