41 Thoracic Pedicle Technique
I. Key Points
– Transpedicular instrumentation allows for anterior and posterior column spinal fixation for a more rigid construct that is biomechanically superior to the use of thoracic hooks.
– Thoracic pedicles are smaller and more variable in size than pedicles of the lumbar spine.1
– Sagittal pedicle height gradually increases from upper to lower thoracic spine.
– Transverse pedicle width decreases from the upper thoracic spine to the mid-thoracic spine (T5-T6) before gradually increasing through the lumbar spine.
– The transverse pedicle angle decreases from T1 to T12.
– Straightforward screw trajectories are associated with higher pullout strengths than anatomic trajectories, although anatomic trajectories may allow for a larger pedicle screw diameter.2
– Extrapedicular screws are biomechanically inferior to intrapedicular screws but are an excellent alternative when anatomy dictates their use.3
II. Indications
– Reduction and stabilization of traumatic fractures
– Stabilization for tumor resection, infection, or spinal inflammatory disease (i.e., ankylosing spondylitis)
– Correction of spinal deformity such as kyphosis or scoliosis
III. Technique
– The authors use a free hand technique4 and prefer to place the pedicle screw parallel to the superior end plate with appropriate medial angulation. Fluoroscopy and image guidance may be used at the discretion of the surgeon.
– Exposure
• Soft tissues are meticulously cleared from the posterior elements of the levels to be fused, and the levels above and below, including their facet capsules, are spared.
• Exposure extends from the spinous process, lamina, and facet medially to the tips of the transverse processes laterally.
– Facetectomy
• The facet capsules are cleared of soft tissue to expose the “plateau” ridge of the thoracic lamina above the “valley” of the superior facet. At the intermediate levels the inferior facet may be removed with an osteotome to assist with visualization of the superior facet.
– Starting point (Fig. 41.1)
• Cortical burr holes are made in the thoracic lamina ridge (plateau) 1 to 2 mm lateral to the midpoint of the superior facet (valley).
• Starting points are generally more lateral at the upper thoracic spine and become more medial toward the mid-thoracic spine (T7) before once again becoming more lateral in the distal thoracic spine.
• Look for a cortical “blush” after the burring, which suggests entry into the cancellous portion of the pedicle.
– Pedicle probe
• We use a 35 mm pedicle probe having a blunt 2 mm tip with a slight curve.
• The probe is initially pointed laterally to avoid medial wall violation and inserted to a depth of 15 to 20 mm. A hole probe is then used to assess for a floor, and all four walls (superior, inferior, medial, and lateral) are assessed for breaches.
• The probe is then reinserted with the curve pointed medially into the vertebral body at an appropriate depth based on computed tomography (CT) scan (average of 30 mm in the upper levels and 40 to 45 mm in lower levels). The probe is removed and the hole probe is inserted to again assess the four walls and the floor for violations of the cortex.
– Tapping
• The tract is then under-tapped using a tap diameter 1 mm smaller than that of the planned screw. If the tract is small or if there is any concern about deviation, the tract may be tapped using a cannulated tap over a K-wire.
• After the tap is removed, the hole is probed again for breaches. The depth of the hole probe is measured and compared with the preoperative length of the planned screw before a decision is made on the appropriate screw length.
– Screw placement
• The screw is slowly placed into the pedicle tract with close attention paid to make sure it does not deviate from the planned trajectory.
– Screw confirmation
• Screw placement can be assessed using intraoperative anteroposterior (AP) and lateral x-ray, fluoroscopy, or CT scanning.
• Triggered electromyography (EMG) from intercostal and abdominal muscles can be used to test screws prior to placing the rods, although this method is not as reliable as it is for the lumbar spine
– Salvage techniques
• New tracts in different trajectories can be made using the same technique as described above. K-wires and cannulated taps may be used to avoid entry into the original tract, and care must be taken when placing the tap or screw over the K-wire to prevent the K-wire’s advancement due to binding.
• Extrapedicular screws can be placed by starting more laterally and using a “in-out-in” technique through the transverse process and then back into the vertebral body.
• Pedicle, infralaminar, and transverse process hooks and sublaminar wires can also be utilized if necessary.
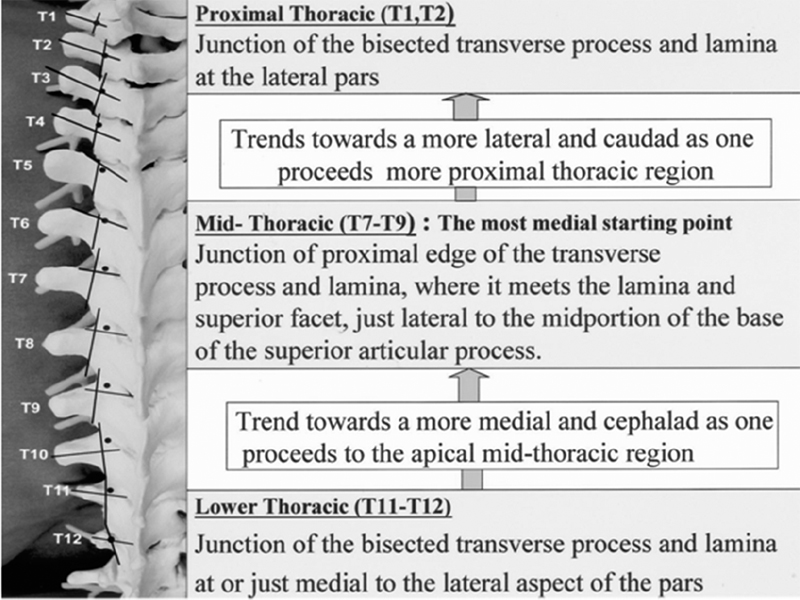
Fig. 41.1 Pedicle screw starting points with 3.5 mm acorn-tipped burr. The posterior elements are burred to create a posterior cortical breach roughly 5 mm in depth. (From Kim YJ et al, Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29(3):333-342. Reprinted with permission.)
IV. Complications
– Medial breach rates range from 0.04 to 24%. Breaches as great as 2 to 4 mm (similar to the volume taken up by a thoracic hook) may be tolerated without injury to the spinal cord, which lies 2 to 4 mm medial to the pedicle at some levels.4
– Lateral breach rates range from 0.4 to 29% and may result in injuries to the aorta, segmental vessels, lung parenchyma, or visceral structures, or pneumothorax.
– Anterior cortical breaches range from 0 to 8% and have the potential to cause injuries to the esophagus, aorta, or vena cava.
– Both proper screw placement and the ability to detect a breach in the pedicle using a probe have been shown to be dependent on the level of training of the surgeon. Medial breaches are more difficult to detect than lateral breaches. Breaches of the anterior cortex are easiest to detect.
V. Postoperative Care
– Follow-up imaging is done at the discretion of the surgeon. The authors prefer early postoperative CT scanning to evaluate placement if an intraoperative CT scan was not performed.
VI. Outcomes
– Multiple clinical and biomechanical studies have shown that properly placed pedicle screw constructs are superior to hook or hybrid constructs in terms of rigid fixation, the ability to correct coronal and sagittal deformities, and preventing loss of correction.
– Experienced spine surgeons report malpositioning of screws at rates of 1.5 to 6.2%. CT scans detect pedicle perforation at higher rates than x-rays.4
– Neurologic, vascular, and visceral injuries are rare (<1%) but can be devastating.
VII. Surgical Pearls
– A thin-cut CT scan is helpful for reviewing the anatomy of thoracic pedicles and their relationship to neurovascular structures prior to surgery.
– Pedicle screws may be augmented by injections of polymethylmethacrylate (or hydroxyapatite, calcium phosphate, or carbonated apatite) in patients who are at risk for screw pullout (i.e., those with osteoporosis).
– Extrapedicular screws (using the “in-out-in” technique) are a viable option when the pedicles are too small to accept a screw or for revision instrumentation cases.
– Limit soft-tissue exposure to the levels being fused and avoid disrupting the facet capsules at the levels above and below the fusion.
– Any change in resistance upon insertion of the pedicle probe should raise suspicion of a tract violation, and the tract should be probed immediately. Medial breaches are located in the first 10 to 15 mm of the tract.
Common Clinical Questions
1. Extrapedicular thoracic screws (i.e., those that use the “in-out-in” technique):
A. Are biomechanically stronger than intrapedicular screws
B. Are biomechanically equivalent to intrapedicular screws but carry a higher risk of injury
C. Are biomechanically weaker than intrapedicular screws
D. Cannot be used as a salvage technique for a missed screw
2. True or false: Tapping the screw tract is not a useful technique in the thoracic spine due to the small pedicle size.
3. True or false: CT scanning is the most accurate indicator of appropriate screw positioning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







