Chapter 139 Cervical Spine Fusion Using Dynamic Ventral Cervical Plating
The benefits of rigid implants (i.e., internal fixation) in the axial skeleton include rigid stabilization, maintenance of alignment, minimal postoperative immobilization, earlier return to function, and potentially enhanced fusion rates.1 A potential shortcoming of rigid implants is that they may stress-shield the bone graft and result in nonunion or implant failure or both. Stress-shielding refers to an implant-induced reduction of bone healing–enhancing stresses and loads, resulting in stress reduction osteoporosis or nonunion (Fig. 139-1). This hypothesis is in keeping with Wolff’s law, which postulates that the form and function of bone is a result of changes in the internal architecture according to “self-ordered” mathematical rules.2 In contemporary terms, skeletal morphology is substantially controlled by mechanical function, and bone remodeling, both locally and throughout the skeleton, is influenced by the level and distribution of the functional strains within the bone.3,4 A corollary to Wolff’s law is that bone heals optimally under compressive, as opposed to tensile, forces. Experimental studies in the thoracolumbar spine show that a 70% or greater axial load should be transmitted through the spine, not the implant, optimally to enhance arthrodesis and provide acute stability.5
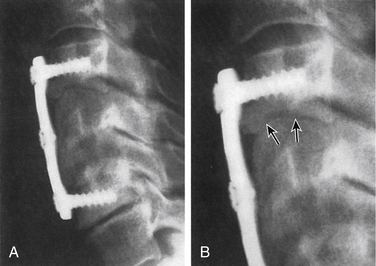
In an attempt to improve on the shortcomings of rigid implants, there has been a resurgence of interest in dynamic implants, in particular, for use in the cervical spine. The concept of dynamic implants is not new. Dynamic hip arthroplasties have been employed successfully for femoral neck fractures. These dynamic implants allow for the femoral neck to shorten or collapse along its axis so that the bone is subject to optimal bone-healing compressive forces.6 Advocates of dynamic implants hypothesize that implants that permit a limited and controlled type of deformation may be desirable. Some experts have termed this controlled dynamism. In the spine, allowing for some axial deformation but not angular deformation (kyphosis) may be optimal. Occasionally, the failure of a rigid implant may permit fusion because the bone graft and vertebral bodies are subsequently exposed to the appropriate bone healing–enhancing forces. In this case, the implant has “dynamized by failing” (Fig. 139-2).
The first ventral cervical plate and screw system was introduced by Bohler7 in 1964. This system ultimately culminated in the development of the Caspar (Aesculap, Center Valley, PA) and Orozco (Synthes, West Chester, PA) plate systems in the early 1980s. These early ventral cervical plates were dynamic implants and are classified as having unrestricted backout properties (i.e., nonlocking and nonrigid) because of a lack of fixation at the screw-plate interface. These implants permit a significant transfer of load through the bone graft, increasing the likelihood of fusion. The nonfixed moment arm nature of the screw causes degradation of the screw-bone interface with cyclic loading. This effect can be minimized with bicortical screw purchase, which requires C-arm fluoroscopy. The main disadvantage of these plates is that the nonlocking and nonrigid (i.e., variable angle) screws led to high rates of screw backout and screw breakage with graft subsidence (Fig. 139-3).
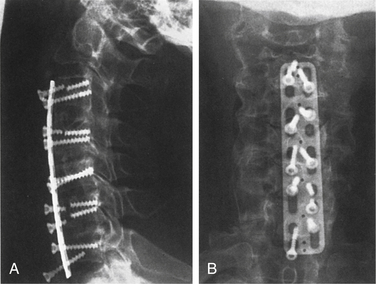
The next generation of ventral cervical plates included CSLP (Synthes) and Orion (Sofamor Danek, Memphis, TN). The CSLP was developed by Morscher in Europe in the early 1980s and introduced in the United States in the early 1990s. The major advantage of this generation of devices is that they do not require bicortical screw purchase. The CSLP uses a titanium expansion screw that rigidly secures the screw to the plate, greatly reducing the incidence of screw backout. In contrast to the Caspar plate where screw angulation could be varied, the CSLP has a predetermined (rigid) screw trajectory: perpendicular at the caudal end and 12 degrees rostrally. It has been suggested that these types of restricted, constrained plate-screw configurations are preferable in trauma cases, in which obtaining immediate stability is desired; however, this concept remains unproven.
One concern with rigid plates such as CSLP and Orion is that they are thought to stress-shield the bone graft by reducing the compressive forces that the bone graft experiences and result in increased rates of nonunion (pseudarthrosis).8 This concern led to interest in the design of dynamic implants. These newer-generation dynamic implants improved on the Caspar plate design by preventing screw backout, while allowing for some movement at the plate-screw interface. This dynamism allowed for compressive forces to be shared between the implant and the bone graft—so-called load sharing. Dynamic cervical plates can be classified into rotational or translational, depending on the type of movement that is permitted at the plate-screw interface. The translational dynamic plates also can be subdivided further into internally and externally dynamized plates.
Rotational Toggle Dynamic Plates
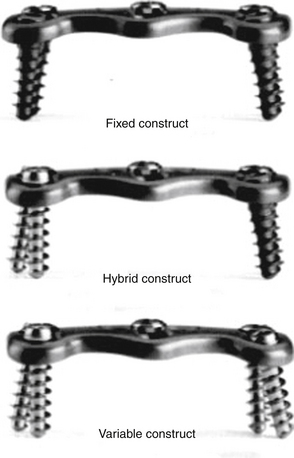
The original Codman plate system, now called Skyline (Depuy, Johnson & Johnson, Raynham, MA), uses screws that “toggle” at the screw-plate interface, increasing the load on the graft and allowing for controlled subsidence. As with the Caspar plate, variable screw trajectories can be used; however, a built-in cam-locking mechanism restricts the screws from backout.9,10 The Atlantis cervical plating system (Medtronic, Memphis, TN) features a floating washer design that prevents screw backout. The Atlantis plate incorporates the most beneficial aspects of several types of cervical plate design. It uses either a variable (i.e., nonfixed) angle cantilever screw or a fixed-angle cantilever screw (Fig. 139-4). As a result of this flexibility, one can create a rigid construct (similar to CSLP or Orion) or a pivot rotational construct (similar to the Codman plate) or a hybrid construct with both fixed and rigid qualities. The fixed-angle screws using the Atlantis system are directed 12 degrees rostrally or caudally or both and 6 degrees medially. The hybrid Atlantis construct, with fixed-angle screws inferiorly and variable angle screws superiorly, may have the advantage of allowing for “controlled subsidence;” the rostral screws are allowed to pivot, while the caudal screws remain fixed. In this way, the graft is subjected to compressive forces as the construct settles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree