40 Cervical-Thoracic Junction Technique
I. Key Points
– The cervical-thoracic junction (CTJ) is an anatomically and biomechanically unique region of the vertebral column that is particularly susceptible to traumatic injury, intervertebral disk and zygapophyseal joint degeneration, and iatrogenic (postsurgical) deformity.1,2
– Reconstruction and fixation at the CTJ must be carefully planned, with key anatomic and biomechanical principles taken into account.
• The CTJ is a transitional zone between the mobile, lordotic cervical spine and the relatively rigid, kyphotic thoracic spine.
• Posterior element morphology transitions from large lateral masses and small pedicles in the cervical spine to larger pedicles and indistinct lateral masses in the thoracic spine, with implications for posterior fixation.
– Several surgical approaches exist for accessing pathology at the CTJ, and the choice of the most appropriate approach requires a comprehensive preoperative workup.
• Thorough history with attention to pulmonary status, overall cardiac health, prior neck surgery or radiation therapy (ear, nose, and throat [ENT]evaluation of vocal cords and recurrent laryngeal nerve function should be considered for these patients), and prior thoracic surgery
• Physical examination with attention to signs of myelopathy but also to body habitus and sagittal balance to identify any relevant deformity such as thoracic hyperkyphosis
• Multimodality radiographic evaluation
 Standing anteroposterior (AP) and lateral radiographs with swimmer’s view (consider placing a radiopaque marker in the manubrial notch)
Standing anteroposterior (AP) and lateral radiographs with swimmer’s view (consider placing a radiopaque marker in the manubrial notch)
 Magnetic resonance imaging (MRI) for assessment of the neural elements and discoligamentous structures
Magnetic resonance imaging (MRI) for assessment of the neural elements and discoligamentous structures
 Computed tomography (CT), especially in trauma and for assessment of posterior element morphology when posterior fixation is planned (thin cuts and three-dimensional reconstructions may further aid preoperative planning)
Computed tomography (CT), especially in trauma and for assessment of posterior element morphology when posterior fixation is planned (thin cuts and three-dimensional reconstructions may further aid preoperative planning)
 Consider a vascular study (e.g., CT angiography) to delineate vertebral artery anatomy
Consider a vascular study (e.g., CT angiography) to delineate vertebral artery anatomy
– The superior mediastinum is unfamiliar territory for most spine surgeons. It contains critical structures such as the thoracic duct, azygos vein, great vessels and their branches, the sympathetic chain, and the pleural apices, thus carrying the potential for catastrophic visceral injury.
II. Indications
– Fractures
• Unstable traumatic fracture/dislocation
• Osteoporotic fracture causing neurologic deficit, deformity, or persistent pain refractory to less invasive treatments
– Neoplasms
• Vertebral/epidural metastases
• Intradural-extramedullary tumors
• Intramedullary tumors
– Infection
• Osteomyelitis/discitis meeting criteria for surgery
• Spinal tuberculoma (Pott disease)
– Deformity
• Post-laminectomy kyphosis
• Chin-on-chest deformity
• Degenerative kyphoscoliosis
• Posttraumatic kyphosis
– Symptomatic herniated nucleus pulposus in the upper thoracic spine (C7-T3)
• Radiculopathy (after 6 to 8 weeks of failed conservative therapy)
• Neurologic deficit from spinal cord compression
III. Technique
– Three principal approaches to the CTJ
• Anterior
• Anterolateral
• Posterior
• Options
 Suprasternal (i.e., conventional low cervical or “Smith-Robinson”) approach: use preoperative mid-sagittal cervical-thoracic MRI or CT to determine the lowest vertebra and intervertebral disc accessible without sternotomy.
Suprasternal (i.e., conventional low cervical or “Smith-Robinson”) approach: use preoperative mid-sagittal cervical-thoracic MRI or CT to determine the lowest vertebra and intervertebral disc accessible without sternotomy.
 Transclavicular (not discussed here; see Kurz et al5)
Transclavicular (not discussed here; see Kurz et al5)
 Transmanubrial/sternal splitting (Fig. 40.1)
Transmanubrial/sternal splitting (Fig. 40.1)
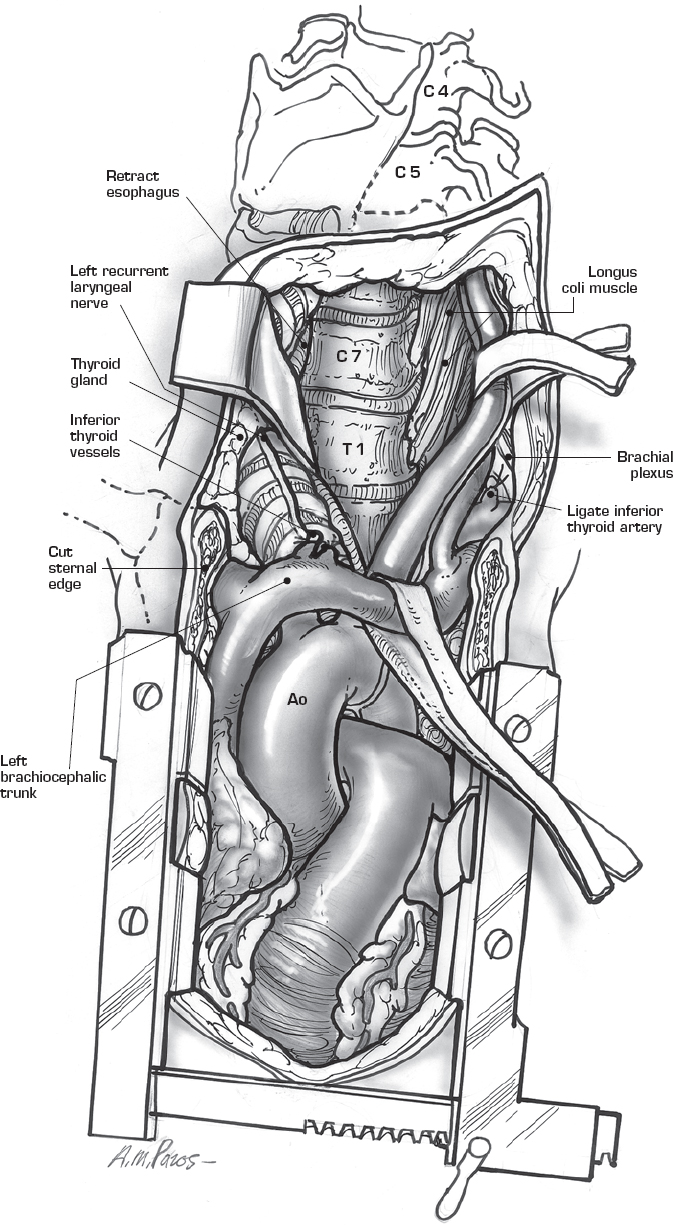
Fig. 40.1 Sternal splitting approach and exposure. (From HaherR, Merola A,Surgical Technique for the Spine, Thieme; pg. 74, Fig. 15-2B.)
• Advantages
 Permits direct visualization of ventral pathology
Permits direct visualization of ventral pathology
 Ideal for approaching a midline ventral lesion causing cord compression, and for performing an anterior release for correction of deformity
Ideal for approaching a midline ventral lesion causing cord compression, and for performing an anterior release for correction of deformity
• Disadvantages
 Superior mediastinum is unfamiliar anatomy and may require the assistance of an access surgeon, particularly for transsternal approach.
Superior mediastinum is unfamiliar anatomy and may require the assistance of an access surgeon, particularly for transsternal approach.
 Risks injury to recurrent laryngeal nerve, thoracic duct, and sympathetic chain (Fig. 40.2)
Risks injury to recurrent laryngeal nerve, thoracic duct, and sympathetic chain (Fig. 40.2)
 Sternal splitting adds significant morbidity.
Sternal splitting adds significant morbidity.
– Anterolateral (transthoracic) approach2
• Advantages
 Permits visualization of anterior pathology from anterior vantage point
Permits visualization of anterior pathology from anterior vantage point
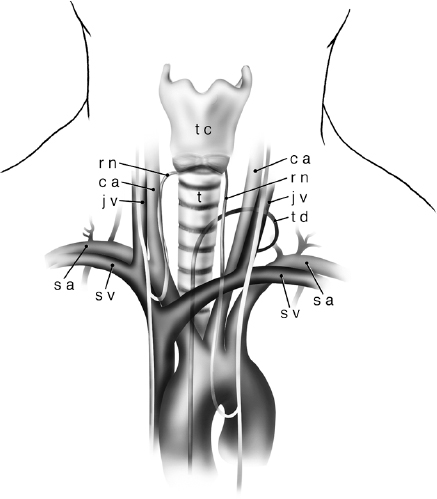
Fig. 40.2 Surgical anatomy relevant to an anterior cervical discectomy. Subclavian artery (sa), subclavian vein (sv), carotid artery (ca), jugular vein (jv), recurrent laryngeal nerve (rn), thoracic duct (td), trachea (t), and thyroid cartilage (tc) (with permission from Barrow Neurological Institute).
 Permits anterior column reconstruction with less risk to neural elements
Permits anterior column reconstruction with less risk to neural elements
• Disadvantages
 Typically requires the assistance of an access surgeon
Typically requires the assistance of an access surgeon
 Violation of thoracic cavity and attendant pulmonary morbidity
Violation of thoracic cavity and attendant pulmonary morbidity
• Options
 Straight midline approach (cervical-thoracic laminectomy, with possible addition of pedicle screw fixation)
Straight midline approach (cervical-thoracic laminectomy, with possible addition of pedicle screw fixation)
 Lateral extracavitary approach
Lateral extracavitary approach
 Transpedicular approach
Transpedicular approach
 Costotransversectomy
Costotransversectomy
 Pedicle subtraction/Smith-Peterson osteotomy
Pedicle subtraction/Smith-Peterson osteotomy
• Advantages
 Does not require the assistance of an access surgeon
Does not require the assistance of an access surgeon
 Dissection is entirely extrapleural
Dissection is entirely extrapleural
 Single approach allows for both decompression and stabilization
Single approach allows for both decompression and stabilization
• Disadvantages
 Ventral pathology may be obscured by the spinal cord and nerve roots.
Ventral pathology may be obscured by the spinal cord and nerve roots.
 Does not permit correction of a fixed kyphotic deformity
Does not permit correction of a fixed kyphotic deformity
 Muscle atrophy and/or proximal junctional instability may result from overly aggressive dissection during exposure.
Muscle atrophy and/or proximal junctional instability may result from overly aggressive dissection during exposure.
 Anterior column reconstruction through posterior approach places the neural elements at risk.
Anterior column reconstruction through posterior approach places the neural elements at risk.
– Special considerations in performing posterior fixation at the CTJ
• Screws in this region are under significant stress and at greater risk of pullout or breakage.1,2,6
 Avoid stopping a construct at the CTJ (C6-T2).
Avoid stopping a construct at the CTJ (C6-T2).
 Consider bicortical fixation.
Consider bicortical fixation.
• Rods must be carefully contoured with attention to differences between the patient’s preoperative curvature and the desired final result.6
 Ensure that sagittal balance and horizontal gaze are preserved or restored.
Ensure that sagittal balance and horizontal gaze are preserved or restored.
 Limit the prominence of the rod ends (particularly in thinner patients).
Limit the prominence of the rod ends (particularly in thinner patients).
• The transition from lateral mass screws in the low cervical spine to pedicle screws in the thoracic spine complicates rod contouring and placement.6
 Consider cervical pedicle screw fixation.
Consider cervical pedicle screw fixation.
 Use polyaxial screws for fixation at—and immediately adjacent to—the CTJ.
Use polyaxial screws for fixation at—and immediately adjacent to—the CTJ.
 Dual-diameter rods are available to accommodate the larger heads of lower thoracic pedicle screws.
Dual-diameter rods are available to accommodate the larger heads of lower thoracic pedicle screws.
 For some long constructs and difficult deformity cases, cross-connectors may be used to connect noncollinear rods.
For some long constructs and difficult deformity cases, cross-connectors may be used to connect noncollinear rods.
Anterior (Transmanubrial) Approach1,2
– Place patient in supine position on radiolucent table.
• Consider electrophysiologic monitoring such as somatosensory and motor evoked potentials (SSEPs, MEPs), particularly in cases of spinal cord compression and/or myelopathy.
• Preoperative reduction with traction may be beneficial in cases of severe kyphosis (obtain initial baseline SSEPs and MEPs prior to attempting reduction).
– Sterile prep and drape.
– Incision (Fig. 40.1)
• May use T-shaped incision on the anterior chest wall or an oblique supraclavicular incision beginning just anterior to the (left) sternocleidomastoid muscle and extending inferomedially over the sternum for a variable length depending on the level of the pathology.
 Manubrium typically corresponds to T2-T3 level (correlate with preop imaging).
Manubrium typically corresponds to T2-T3 level (correlate with preop imaging).
 Left-sided approach may facilitate avoidance of recurrent laryngeal nerve injury.
Left-sided approach may facilitate avoidance of recurrent laryngeal nerve injury.
– Divide platysma and perform sharp dissection to define sternocleidomastoid and strap muscles superiorly.
• Transection of the omohyoid muscle may permit additional retraction.
– Identify the manubrium inferiorly and perform subperiosteal dissection posteriorly, taking care to protect the brachiocephalic veins.
– Using a sternal saw or high-speed drill, split the manubrium.
• Take care to preserve muscular attachments.
– Perform blunt dissection of the potential space medial to the carotid sheath and lateral to the strap muscles, down to the prevertebral fascia.
• Take care to avoid injury to the thoracic duct (typically on the left and at C7-T1, but may extend up to C6 in some cases).
– Confirm pathologic level using fluoroscopy or plain radiography.
– Perform decompression (discectomy, corpectomy) and stabilization.
• Use long-handled, angled instruments to overcome the long distance from the anterior chest wall to the anterior thoracic spine, and to avoid line-of-sight issues.
• Options for anterior column reconstruction
 Iliac crest autograft (“gold standard” but associated with donor site morbidity)
Iliac crest autograft (“gold standard” but associated with donor site morbidity)
 Allograft strut
Allograft strut
 Polyetheretherketone (PEEK) or titanium cage (avoid titanium in osteoporotic patients due to large discrepancy in modulus of elasticity and possibility of settling)
Polyetheretherketone (PEEK) or titanium cage (avoid titanium in osteoporotic patients due to large discrepancy in modulus of elasticity and possibility of settling)
 Typically supplement with anterior plate fixation
Typically supplement with anterior plate fixation
– Fill wound with saline and watch for bubbles (the presence of bubbles indicates transgression of the apical visceral pleura and necessitates placement of a chest tube through a separate incision).
– Leave a drain in the prevertebral space.
– Close in layers (wire manubrium).
IV. Complications
– Minor
• Superficial wound dehiscence
• Injury to strap muscles (exacerbating preexisting respiratory compromise)
• Nonunion of the clavicle/manubrium
• Traction injury to the recurrent laryngeal nerve
– Major
• Injury to carotid sheath
• Injury to azygos vein
• Injury to thoracic duct (chyle leak)
• Injury to great vessels in the mediastinum
• Injury to the sympathetic chain (Horner syndrome)
• Injury to pleural apices (hemopneumothorax)
• Perforation of trachea or esophagus
• Deep wound infection
• Cerebrospinal fluid (CSF) leak
• Injury to spinal cord or exiting nerve roots
V. Postoperative Care
– Consider monitoring patient in the intensive care unit, particularly in cases of lengthy operative time, significant blood loss, and preoperative pulmonary or cardiac compromise.
– Perioperative hypotension should raise concern of great vessel injury after an anterior approach.
– For anterior approaches, monitor drain output for evidence of chyle leak.
– Consider maintaining patient in cervical-thoracic orthosis for 8 to 12 weeks in patients with poor bone quality or when fixation is otherwise felt to be suboptimal.
VI. Outcomes
– No long-term studies or large series have been reported.
– Small series report anterior approach–related mortality of 0 to 40%, but comprise different patient populations with widely varying pathology and premorbid status.1,2
– Posterior approaches are probably associated with decreased morbidity.
VII. Surgical Pearls
– Preoperative workup is critical, with special attention paid to body habitus and sagittal balance, cardiopulmonary comorbidities, and appropriate imaging, including the anterior chest wall (when anterior approach is being considered).
– Assistance of an access surgeon is advisable for work in the superior mediastinum.
– Avoid stopping a construct at the CTJ and consider bicortical screws for greater strength.
– Anterior column reconstruction is essential, since it is responsible for 80% of load bearing.
– Posterior approaches are probably associated with less morbidity but place the neural elements at increased risk when pathology is wholly ventral, or when one is placing an anterior graft.
Common Clinical Questions
1. What elements of the patient history and physical examination are uniquely important when one is considering a surgery at the cervical-thoracic junction?
2. What are the advantages and disadvantages of the anterior approach to the cervical-thoracic junction?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






