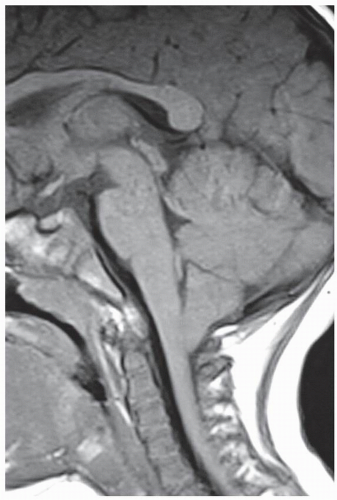
CHIARI I
The clinical presentation and symptomatology of the Chiari I malformation is varied. The most common symptom is headache. Also, ocular, otoneurologic, brainstem, lower cranial nerve, cerebellar, and spinal cord disturbances can occur. The headache is mostly described to range from a light pressure to an intense suboccipital pounding that mostly radiates upward toward the vertex and retro-orbital region and downward toward the neck and shoulders. Characteristically, the headaches tend to worsen with Valsalva maneuvers, by lowering the position of the head and/or by sudden changes in body position, and with exercise.
The ocular symptoms that have been found in these patients are (
Table 39.2) photophobia, blurred vision, diplopia, phosphenes, visual blackouts, and visual field cuts. On the fundoscopic examination, papilledema and decreased or absent venous pulsations in one or both eyes can be found; extraocular muscle palsy can also occur. The otoneurologic symptoms may include loss of equilibrium, vertigo, tinnitus, dizziness, nausea and vomiting, oscillopsia, and hypoacusia or hyperacusia. On the examination, nystagmus can also be found (lateral, downbeat, and/or rotary) (
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27 and
28).
The brainstem, lower cranial nerve, and cerebellar symptoms that can occur are sleep apnea, dysphagia, syncope, hoarseness/dysarthria, facial pain/numbness, throat pain, palpitations, shortness of breath, and various degrees of incoordination. On the exam, an impaired gag reflex, vocal cord paralysis, decreased trapezius muscle strength, hypertension, dysmetria, and truncal ataxia can be found.
The symptoms related to the spinal cord, caused by ventral spinal cord compression, dorsal cord compression, and/or a cord syrinx, are motor (spasticity, muscular weakness, and atrophy), sensory (hyperesthesia, hypoalgesia, anesthesia, burning dysesthesia, decreased positional sense, and temperature sensation), urinary and/or fecal incontinence, and impotence. On the exam, muscular weakness, muscular atrophy, decreased hand fine-motor ability, trophic phenomena dissociated sensory loss, hyperreflexia or hyporeflexia, and Babinski sign can be found. Scoliosis from syringomyelia can occur; a left thoracic curve as well as abnormal abdominal cutaneous reflexes sometimes can differentiate it from an idiopathic-type scoliosis.
CHIARI II
The Chiari II is only found and universally associated with the myelomeningocele patient population. Therefore, one can make a diagnosis of a Chiari II, even if no symptoms are present, in a newborn with a myelomeningocele. In the neonate with either Chiari I or Chiari II, the most common signs that can be found are stridor, apnea, poor feeding, and opisthotonos. In the Chiari II, within the respiratory difficulty complex, the most noticeable sign is inspiratory stridor. This is produced by a dysfunctional 10th cranial nerve and thus manifests in vocal cord paralysis.
In infants and young preschoolers, the symptomatology of the Chiari II malformation is most frequently related to brainstem compression and therefore can be a neurosurgical emergency. There can be respiratory difficulties, inspiratory stridor, apnea, aspiration pneumonia, nasal regurgitation, weight loss, prolonged feeding time, achalasia, extremity paresis, hypotonia, and opisthotonos (
29,
30,
31,
32,
33 and
34).
In older children and adults, the most common symptoms are those caused by a cervical myelopathy, and therefore, one can find spasticity and upper-extremity weakness, occipitocervical pain, changes in their handwriting, and loss of muscle bulk. Also, there can be truncal and appen-dicular ataxia, dysarthria, nystagmus, difficulty in convergence, and Parinaud’s syndrome. Scoliosis, disassociated thermoalgesia, and back pain should prompt suspicion for syringomyelia.