Chapter 62 Classification of Thoracolumbar Spine Fractures
Review of Thoracolumbar Classification Schemes
The biomechanical force vectors acting on the spine can be either rotational or linear. Among the rotational forces are flexion, extension, lateral bending, and torsional forces. Linear forces include compression, translational, and distraction forces. These forces can act alone or in combination, resulting in different and diverse fracture patterns.1 Although not always possible, categorizing a fracture based on a classification system is crucial to aid the clinician in selecting the appropriate management strategy. An effective classification system should be comprehensive, easy to apply, and directive of appropriate treatment.2
Current classification systems base their algorithms on the stability of different fracture patterns. The earliest attempt to classify thoracolumbar spine fractures was reported by Boehler in 1929.2 He grouped thoracolumbar fractures into five entities: compression, flexion-distraction, extension, shear, and rotational fractures. In 1938, Watson-Jones3 divided these fractures into simple wedge fractures, comminuted fractures, and fracture-dislocations. He introduced the concept of instability and was the first to associate the integrity of the posterior ligamentous complex (PLC) with spinal stability. In 1949, Nicoll4 categorized fractures into stable and unstable fractures. He ascribed four structures as contributing to spinal stability: the vertebral body, the disc, the facets, and the interspinous ligaments. In his view, the integrity of the latter was the major determinant of stability. He classified thoracolumbar spine fractures into anterior wedge, lateral wedge, fracture-dislocations, and neural arch fractures.
In his landmark 1963 paper, Holdsworth introduced the two-column theory of spinal stability.5 He recognized five mechanisms of injury: flexion, flexion-rotation, extension, compression, and shear forces. His classification scheme included anterior compressions; fracture-dislocations; rotational fracture-dislocations; and extension, shear, and burst fractures. He then categorized fractures as stable or unstable. According to his model, the spine was divided into anterior and posterior columns. The anterior column consisted of the vertebral body and the intervertebral disc, and the posterior column consisted of the neural arch, facet joints, and PLC (interspinal and supraspinal ligaments and ligamentum flavum). Fractures that included posterior column injury were unstable. His model thus defined burst-type fractures, which he was the first to describe, as stable.
In a sometimes controversial formulation, White and Panjabi in 1978 defined clinical instability as the inability of the spine under physiologic loads to maintain relationships between vertebrae such that there is neither acute nor subsequent neurologic injury, deformity, or pain.6 In addition to neurologic deficit, motion, and disruption of the anterior and posterior “elements,” their algorithm recognized the significance of pain and the anticipated loading of the spine. The latter, although significant, had not been identified in previous paradigms of fracture severity.
The three-column theory of the spine was introduced by Francis Denis in 1983.7 He added a third or middle column to Holdsworth’s two-column model. According to Denis, the anterior column of the spine comprised the anterior longitudinal ligament and the anterior half of the vertebral body, anulus, and disc. The middle column included the posterior half of the vertebral body, anulus, and disc, in addition to the posterior longitudinal ligament. The posterior column incorporated the neural arch, facets, and PLC, which consisted of the supraspinal and interspinal ligaments, ligamentum flavum, and facet capsules (Fig. 62-1). The middle column was important because for dislocation to occur, it was necessary to disrupt the middle column along with the anterior or posterior column, or both. Denis defined stability based on the integrity of two of the three columns. His classification included four groups: compression fractures resulting from failure of the anterior column under compression, burst fractures resulting from failure of the anterior and middle columns secondary to fractures of the vertebral body under axial loads, flexion-distraction injuries secondary to failure of the posterior and middle columns, and fracture-dislocations resulting from failure of all three columns. Under this scheme, flexion-distraction injuries or seat belt-type injuries were considered unstable in the first degree. Burst fractures with deficit were considered unstable in the second degree, and fracture-dislocations were unstable in the third degree. This classification system was later supported by in vitro biomechanical studies.8
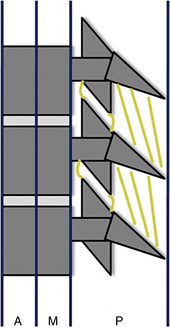
FIGURE 62-1 Denis’s three-column model of the spine: anterior column (A), middle column (M), posterior column (P).
As opposed to Denis, who subdivided basic injury patterns based on review of mostly radiographs of 412 fractures (53 were CT images), McAfee et al. in 1983 based their classification on an examination of CT scans with sagittal reconstruction from 100 patients.9 They recognized six fracture patterns: wedge compression, stable burst, unstable burst, Chance fracture, flexion-distraction, and translational. They linked the stability of burst fractures with the integrity of the PLC, emphasizing the PLC as the major factor in fracture stability. Shortly afterward, in 1984, Ferguson and Allen10 introduced the “mechanistic classification.” They classified fractures into seven categories: compressive flexion, distractive flexion, lateral flexion, torsional flexion, translation, vertical compression, and distractive flexion injuries.
In 1989, Magerl et al.11 introduced the AO (Arbeitsgemeinschaft für Osteosynthesefragen) classification system, based on a 10-year review of 1445 thoracolumbar fractures. They recognized three main fracture types: type A (compression), type B (distraction), and type C (fracture-dislocation). Subdivisions were created according to the severity of the fracture, resulting in 53 fracture patterns, with A1 being the least severe and C3 the most severe. This schema was generated based on review of radiographs, and as a result of their diligence, the schema was extensive and not always user friendly.
The load-sharing classification, introduced by McCormack et al. in 1994,12 was derived from analysis of failures of thoracolumbar spine fractures treated with transpedicular short-segment arthrodesis. Fractures were graded according to the degree of comminution of the body, apposition of the fracture fragments, and deformity. A point system from 1 to 3 was applied to each fracture, with a higher number indicating greater severity. Fractures with a score greater than 7 had a high risk of short-segment fixation failure. This algorithm was intended to aid in the surgical decision of whether to use short-segment arthrodesis or anterior column graft support. The classification was validated biomechanically in vitro.13
In 2005, the Spine Trauma Study Group introduced the Thoracolumbar Injury Severity Score (TLISS) as a new classification system.13–15 The system was based on three injury characteristics: mechanism of injury, neurologic status, and integrity of the PLC. Pertaining to the mechanism of injury, compression injuries are assigned one point; compression fractures with coronal plane deformity greater than 15 degrees and burst fractures are assigned two points. Translational or rotational injuries receive three points, and distraction injuries, being the most unstable, receive four points. The severity of neurologic injury is scored based on a five-category system. Patients with a negative neurologic examination receive zero points. In the presence of nerve root injury or complete spinal cord injury, the fracture is assigned two points. Patients with an incomplete spinal cord injury or cauda equina syndrome are assigned three points. The integrity of the PLC can be assessed clinically by the presence of a palpable interspinous gap, by separation of the spinous processes on plain radiographs, or by MRI. Patients with an intact PLC receive zero points. Those in whom the integrity of the PLC is indeterminate receive two points, and those with confirmed injury receive three points.
Based on a study that showed fair to moderate inter-rater agreement,16 the TLISS system, which emphasizes the mechanism of injury, was modified into the Thoracolumbar Injury Classification and Severity Score (TLICS), which emphasizes the morphology of fractures. In cases of multiple mechanisms involving one or more levels, the TLICS, as opposed to the TLISS, would consider only the most severe injury mechanism. Moreover, the one-point addition for coronal plane deformity was eliminated. Subsequent studies showed that both the TLISS and TLICS were comparable.17,18 Moreover, Lenarz et al.19 showed that the interobserver reliability of the TLISS system was comparable to that of the Denis and AO systems. The TLICS algorithm encompasses radiographic or mechanistic criteria, clinical criteria, and the integrity of the PLC assessed on MRI. No weight is given to the presence of pain, however.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







