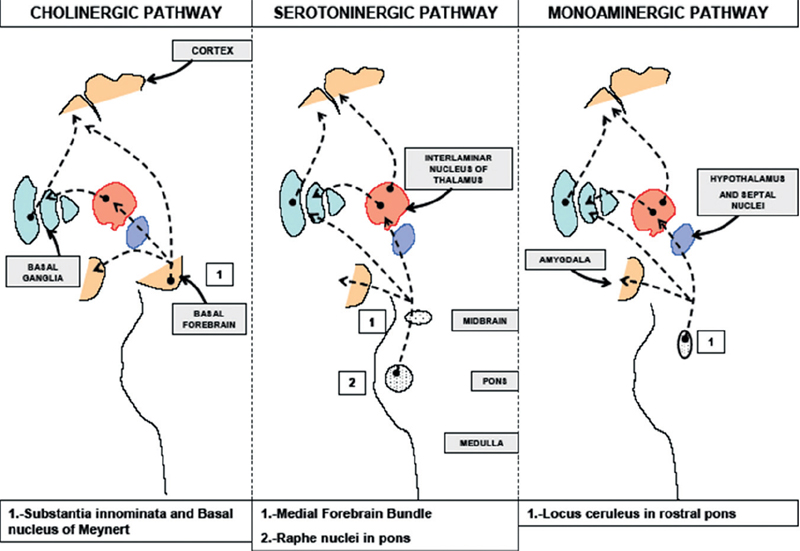
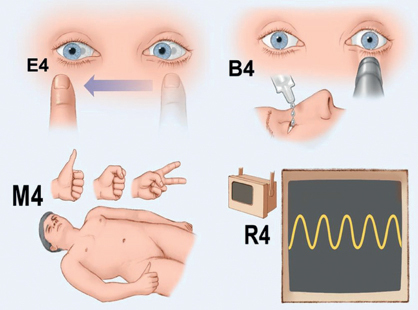
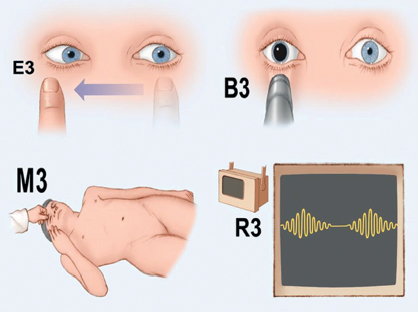
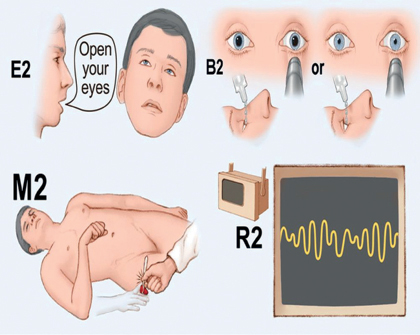
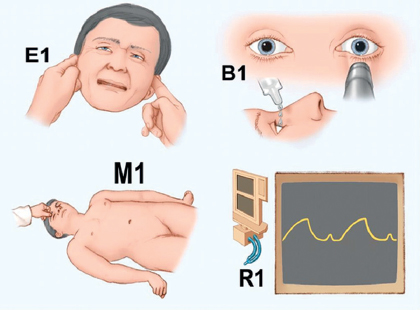
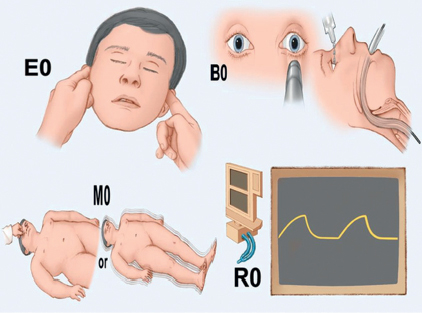
32 Define arousal and content of consciousness. Arousal is related to wakefulness and the level of alertness. The content of consciousness is composed of the sum of cognitive and affective mental functions.1,2 Where is the ascending arousal system located? Rostral pons, midbrain, thalamus, and hypothalamus1 Which pathways participate in the ascending arousal system? As demonstrated in the graph in Fig. 32.1, three systems are involved: cholinergic pathway, serotoninergic pathway and monoaminergic pathway.1 Fig. 32.1 Three systems are involved in the ascending arousal system: cholinergic pathway, serotoninergic pathway and monoaminergic pathway. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) What characterizes the level of alertness? The intensity of the stimulus needed to elicit a meaningful response Define stupor. A state where the patient appears asleep, but can be awakened with vigorous stimulation and returns to sleep when the stimulation ceases1 What is the definition of lethargy and obtundation? Lethargy is mild reduction in alertness, whereas obtundation is moderate reduction in alertness. Both of these terms are subjective and should be used only when additional clarification is given. Define vegetative state. A subset of coma patients in which sleep-wake cycles have returned (or were preserved) but a total lack of cognitive function remains. Approximately what percentage of comatose patients enter a persistent vegetative state (PVS)? Less than 1% The Multi-Society Task Force, established in 1991, has made criteria for diagnosis of the vegetative state. What are they? Multi-Society Task Force diagnostic criteria: 1. No evidence of awareness of self or environment and inability to interact with others 2. No evidence of sustained, reproducible, purposeful, or voluntary behavioral responses to visual, auditory, tactile, or noxious stimuli 3. No evidence of language comprehension or expression 4. Intermittent wakefulness manifested by the presence of sleep-wake cycles 5. Sufficiently preserved hypothalamic and brainstem autonomic functions to permit survival with medical and nursing care 6. Bowel and bladder incontinence 7. Variably preserved cranial nerve reflexes and spinal reflexes What distinguishes persistent vegetative state from permanent vegetative state? What is the prognosis of each? Persistent vegetative state: When the vegetative state exceeds 1 month; there is potential for recovery, most often in traumatic causes Permanent vegetative state: >1 year after traumatic causes and >3 months after nontraumatic causes; recovery is rarely ever seen Patients in a persistent vegetative state typically have what type of eye opening? Eyes open with spontaneous blinking. These patients do NOT track objects. Sleep-wake cycles are followed. What are the neuropathological causes thought to be responsible for the vegetative state? Diffuse axonal injury in traumatic cases and laminar cortical necrosis in anoxic–ischemic injury What is the definition of minimally conscious state? A state of severely altered consciousness where minimal behavioral evidence of self or the environment exists What is the definition of akinetic mutism? Patients are immobile, have sleep-wake cycles, typically lie with eyes closed, and display little or no vocalization. There is minimal to no response to noxious stimuli. Patients are tracking the examiner and fixating objects. What is psychogenic unresponsiveness? A very rare cause of coma: a psychologically based state in which the patient is not responsive. Typically lasts 1 to 2 days and has a “sudden awakening.” Amnesia of prior events can occur. What is locked-in syndrome (LIS)? A nearly uncommunicative state that closely resembles persistent vegetative state, with which it can easily be mistaken. How does LIS differ from persistent vegetative state? It is set apart from PVS by the ability to communicate through moving the eyes up and down. Unlike PVS, patients suffering from LIS can interact with and communicate with their environment and exhibit awareness. What is the structural lesion responsible for LIS? Acute structural lesion in the pons (usually ventral pons). The usual cause is infarction. What pathways are spared, allowing for the communicative ability of LIS? Pathways to the oculomotor nuclei of the mesencephalon and reticular formation. True or false: LIS patients can hear and feel everything. True. What syndrome can be a complication of central pontine myelinolysis and lesions in the base of the pons? Locked-in syndrome. Cognition is intact in this syndrome. True or false: Coma depth scores (such as Glasgow Coma Scale [GCS] score) can indicate prognosis. True, especially the initial value, prior to the use of sedatives. This area, however, is controversial because some studies have failed to show correlation with outcome of the GCS. What are the components of the GCS? Eye Opening (1 to 4 points) Motor Response (1 to 6 points) Verbal Response (1 to 5 points) What are the highest and lowest possible scores attainable on the GCS? Highest: 15 (spontaneous eye opening, obeying commands, oriented by verbal response) Lowest: 3 (no response in any category) How is eye opening scored on the GCS? 4, spontaneous 3, opens to speech 2, opens to pain 1, no response How is motor response scored on the GCS? 6, obeys commands 5, localizes to pain 4, withdraws from pain 3, abnormal flexor response 2, extensor response 1, no response How is verbal response scored on the GCS? 5, oriented 4, confused conversation 3, inappropriate 2, incomprehensible 1, no response What would be the verbal score of an intubated patient? VT (and still counts as 1!) What is the Full Outline of UnResponsiveness (FOUR)? A scale that has four components (FOUR) instead of the three as on the GCS: 1. Eye 2. Motor 3. Brainstem reflexes 4. Respiration (breathing patterns) Each component has a maximal score of 4 (E4,M4,B4,R4) and minimal score of 0 (E0,M0,B0,R0)3 When should one consider using this scale? In patients with a low GCS score What is an important difference? Each component of GCS starts with 1 as the lowest score, whereas FOUR scale starts with 0. What are some advantages? It has the ability to recognize different stages of herniation. Also, the lowest score, 0, in this scale correlates better with mortality than the lowest score of 3 on the GCS Which findings obtain a score of 4? E: Eyelids open/ed, tracking, or blinking to command M: Thumbs up, fist, or peace sign B: Pupil and corneal reflexes present R: Not intubated, regular breathing pattern Fig. 32.2 A score of 4 on FOUR. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) Which findings obtain a score of 3? E: Eyelids open but not tracking M: Localizing to pain B: One pupil wide and fixed R: Not intubated, Cheyne-Stokes breathing pattern Fig. 32.3 A score of 3 on FOUR. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) Which findings obtain a score of 2? E: Eyelids closed but open to loud voice M: Flexion response to pain B: Pupil or corneal reflexes absent R: Not intubated, regular breathing pattern Fig. 32.4 A score of 2 on FOUR. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) Which findings obtain a score of 1? E: Eyelids closed but open to pain M: Extension response to pain B: Pupil and corneal reflexes absent R: Breathing above ventilator rate Fig. 32.5 A score of 1 on FOUR. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) Which findings obtain a score of 0? E: Eyelids remain closed with pain M: No response to pain or generalized myoclonus status B: Absent pupil, corneal reflex, and cough R: Breathes at ventilator rate or apnea Fig. 32.6 A score of 0 on FOUR. (From Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a New Coma Scale: the FOUR score. Ann Neurol 2005;58:585–593. Reprinted by permission from Mayo Foundation for Medical Education and Research. All rights reserved.) What is the problem with asking a patient to “squeeze my hand” to assess motor response? Reflex grasping. The patient can be squeezing in response to sensing a physical stimulus instead of following a verbal command. Instead, simple verbal commands such as “Show me a thumbs up or two fingers” should be used. When localizing to pain, a patient’s arm ideally should… …either cross midline toward the contralateral noxious stimulus or reach above the mammary line level toward the stimulus applied. What is another term for abnormal flexor response? Decorticate rigidity What is another term for abnormal extensor response? Decerebrate rigidity True or false: Decerebrate and decorticate rigidity are nonlocalizing responses. True. What type of injuries (location) do decerebrate and decorticate rigidity indicate? These responses indicate bilateral hemisphere diencephalic or brainstem lesions. Decerebrate indicates more severe dysfunction, but does not portend a worse prognosis necessarily. What are the characteristic movements of the arms and legs of patients displaying decorticate rigidity? Stereotyped, slow flexion of the arm, wrist, and fingers, along with adduction of the arm. The legs are extended, internally rotated, and plantar flexed. What are the characteristic movements of the arms and legs of patients displaying decerebrate rigidity? Their arms are adducted and the shoulder is internally rotated. Their legs are the same as those with decorticate rigidity, but the hands are pronated in decerebrate rigidity. What can twitching eyelids indicate? Seizures What does a unilateral, dilated, fixed pupil often indicate? Uncal herniation What do bilateral, fixed, midposition pupils often indicate? Diencephalic herniation Intoxication with scopolamine Brain death Atropine intoxication Glutethimide intoxication Methanol intoxication What do pinpoint pupils often indicate? Intoxication with narcotics Acute pontine lesion Argyll Robertson pupils (syphilis) Hypercapnia Nonketotic hyperglycemia A unilateral dilated pupil can be a side effect of what commonly used drug? Scopolamine patch for motion sickness or atropine eye drops for corneal abrasions. Patients can often get the drug on their hand by application or scratching a patch and then touching their eye. It is important to ask patients about its use when an acute dilated pupil is noted. The condition is benign and will wear off. What is the appearance of the pupils in Horner syndrome? Unilateral miotic (pinpoint) pupil What can Horner syndrome indicate? Carotid dissection Evolving medulla stroke due to vertebrobasilar artery occlusion Traumatic sympathetic lesion from catheter in jugular vein Oculomotor (CN III) palsy is often due to what three major causes? Acute intracranial mass Bulbus oculi contusion (late phenomenon) Anticholinergics When the etiology of coma is unclear, what can a physician do to attempt to reverse this condition, given his or her knowledge of common but sometimes occult cause of coma? Administer concentrated dextrose (50% dextrose, 50 mL, 25 g IV). This reverse hypoglycemic episodes that can be less apparent when progressive. In patients with impaired consciousness in which increased intracranial pressure (ICP) is of concern, what initial action can a physician take to help guide management? Place an ICP monitor. What is the management for an acute posterior fossa lesion that leads to progressive obtundation from brainstem compression? Immediate neurosurgical evacuation What serum levels of sodium, calcium, magnesium, carbon dioxide, and glucose are associated with marked impairment of consciousness? Substance Serum Levels Sodium ≤110 mmol/L or ≥160 mmol/L Calcium ≥3.4 mmol/L Magnesium ≥5 μg/L Carbon dioxide ≥70 mm Hg Glucose ≤40 mg/dL ≥800 mg/dL What are the major endocrine-metabolic causes of coma? The 7 H’s: 1. Hypoglycemia 2. Hyponatremia 3. Hepatic failure 4. Hyperosmolar (nonketotic) coma 5. Hashimoto’s thyroiditis (thyroid coma) 6. Hypoadrenalism (Addison’s disease) 7. Hypopituitarism (three or more deficient hormones) What are some acute structural causes of coma? Hemorrhage, infarct, and abscess1,2,4,5 In what manner do tumors or masses typically result in coma? By the local spread of an infiltrating mass or compression of important structures by an enlarging mass What will intracranial lesions below the lower pons cause? Acute dysfunction of autonomic nuclei, resulting in respiratory failure and/or loss of vascular tone How can tegmental pontine lesions result in coma? These lesions interrupt the ascending reticular activating system (ARAS) midway, but must be bilateral to result in impaired consciousness. Mesencephalic damage most commonly occurs as a consequence of what two events? 1. From extension of a lesion from the thalamus (i.e., a destructive intracranial hematoma) or 2. From stenosis of the basilar artery tip, which produces similar infarctions in bilateral thalami and the mesencephalic tegmentum Bilateral thalamic damage that results in coma typically involves what nuclei? Paramedian, but damage to intralaminar, ventral lateral, or lateral posterior nuclei can also impair consciousness By what mechanism do the above lesions result in coma? By interrupting the thalamic cortex and thalamocortical projections What is the most common cause of bilateral thalamic damage? Infarcts of the penetrating thalamogeniculate or anterior thalamic perforating arteries (polar artery and paramedian thalamic perforating arteries of Percheron) True. How can basal ganglia hemorrhages cause coma? By extension into the thalamus, resulting in compression of the contralateral thalamus; or by extension into the ventricles, causing acute obstructive hydrocephalus What are the two major mechanisms by which an acute hemispheric mass can result in coma? 1. Direct (primary) destruction of the brain parenchyma 2. Distant (secondary) effects from herniation and/or compression of otherwise normal tissue A frontal lesion that can have delayed detection is most likely located on what side? On the nondominant hemisphere What are common cerebral herniations? 1. Cingulate (subfalcine) 2. Thalamic (central/diencephalic) 3. Uncal 4. Tonsillar 5. Upward (upward cerebellar or upward transtentorial) 6. Transcalvarial What occurs during central (diencephalic) herniation? A medial force pushes the thalamus and midbrain through the tentorial opening, and during this event the brainstem caves inward. Shearing of the penetrating vessels from the basilar artery results in irreversible brainstem damage. What is the progression of clinical manifestations of central herniation? 1. Midposition, bilateral small pupils that are sluggish to react 2. Cheyne-Stokes breathing (intermittent rapid, apneic) 3. Barely localize to pain or can show withdrawal response 4. Extensor posturing, midposition 5- to 6-mm pupils that are nonreactive; irregular gasping and lack of oculocephalic reflexes develop. To where is the uncus displaced during an uncal herniation? The uncus is herniated into the incisura tentorii. What is the presentation of an uncal herniation? 1. Abrupt appearance of a large pupil that is nonreactive (“blown”) due to initial CN III palsy (which can progress) 2. Decreased level of consciousness, can be secondary to: a. Midbrain compression b. Hydrocephalus due to occlusion of the aqueduct of Sylvius c. Duret hemorrhages of the midbrain and upper pons 3. Hemiparesis 4. Bradycardia and systemic hypertension if triggered by elevated ICP (Cushing’s triad) 5. Visual field defect: compression of ipsilateral posterior cerebral artery resulting in medial temporal or occipital lobe infarction On which side is the hemiparesis and why? • Compression between the midbrain and edge of tentorium can occur sometimes ipsilateral to the lesion, causing a contralateral hemiparesis. • Alternatively, the midbrain can be compressed all the way to the opposite side, the crus cerebri can be compressed against the contralateral tentorium causing paresis, which is contralateral to the damaged crus cerebri but ipsilateral to the mass lesion (this is known as Kernohan’s phenomenon and is a false localizing sign). What is the danger of the improvement of a fixed pupil during uncal herniation? The midbrain can displace horizontally and rotate if compression is not centered. This allows for either vertical extension or buckling of the brainstem with subsequent compression. Compression of the brainstem can result in constriction of the pupils, which can be attributed to false “improvement.” How can cerebellar masses result in altered level of consciousness? Upward or tonsillar herniations can occur. What clinical manifestations typically precede changes in level of consciousness in acute cerebellar masses (i.e., hematomas)? Acute inability to walk or ataxia, gaze palsy, severe headache, vomiting, nystagmus What are predictors of poor outcome in the setting of acute cerebellar hematomas? SBP >200 mm Hg Pinpoint pupils with abnormal brainstem/oculocephalic reflex Size >3 cm Vermian or intraventricular extension Hydrocephalus Brainstem distortion Upward herniation What occurs during an “upward herniation?” Brainstem is pushed upward or cerebellar tissue (especially the vermis) is pushed through the tentorial notch into the supracerebellar cisterns. When can you produce iatrogenic upward herniations? Placing a ventriculostomy catheter prior to adequately decompressing a posterior fossa lesion with impending herniation What are the clinical manifestations of an upward herniation? Progressive paralysis of upward gaze and progression into deeper coma Anisocoria with eventual pinpoint constriction as compression of pons worsens What is the prognosis of patients suffering from hypoxemic-ischemic coma? Undetermined prognosis; overall mortality rate is high mostly due to withdrawal of support6 What physical exam abnormality correlates indirectly with prognosis in hypoxemic coma (the more abnormalities, the worse the prognosis)? The number of abnormal brainstem reflexes; the more abnormal brainstem reflexes, the worse the prognosis. What are the major mechanisms of hypoxia induced by drugs? 1. Interference of oxygen transport 2. Interference of tissue utilization of oxygen 3. Displacement of oxygen by another gas 4. Acute pulmonary edema (e.g., from cocaine) 5. Aspiration pneumonitis (e.g., following seizures) What are the preferred sources of oxygen for the patient with impaired consciousness and hypoxemia? 1. Nasopharyngeal catheters deliver 60% oxygen when the tip of the catheter is above the soft palate. 2. Resuscitation bags are optimal sources of oxygen, providing FiO2 of 0.9 when oxygen flow is 10 mL/min. These methods are preferred over nasal cannula, which deliver only 30% oxygen and easily dislodge. What odorless gas is the leading causes of death by poisoning in the U.S.? Carbon monoxide (CO)7 What are common exposure sources? Old stoves, poorly ventilated fireplaces, furnaces, and combustion engines without adequate ventilation What is the pathophysiological mechanism of CO poisoning? CO bonds hemoglobin (Hb) with 210 times greater affinity than does O2. This causes a left shift of the Hb dissociation curve, resulting in a reduction of O2 unloading to tissues (Haldane effect). CO can also bind myoglobin, which can trigger arrhythmias, hypotension, and hypoxemia from pulmonary edema.7 What are the neuropathological changes from CO poisoning? Predominantly white matter, with demyelination and edema, and in the hippocampus, cerebellum, and globus pallidus Which affected anatomical location is most likely to be seen on CT? Globus pallidus7 What is the presentation of CO poisoning? Symptoms preceding coma are nonspecific and vague, including headache, dizziness, shortness of breath, cherry red lips/skin (rare and usually indicated near-fatal levels of exposure), retinal hemorrhages, dark color of retinal arteries and veins, and pulmonary edema. What is the management of CO poisoning? Measurement of carboxyhemoglobin levels is of paramount importance. Administration of oxygen or time elapse of >6 hours (half-life of carboxyhemoglobin) can result in “falsely low” levels. Can administer 100% oxygen by sealed face mask. If available, hyperbaric O2 decreases the duration of coma by increasing the amount of dissolved oxygen approximately 10-fold. What completely reversible event occurs during hypothermia when core body temperature reaches 27°C? Loss of all brainstem reflexes, which can return with warming. What is the best method to warm core body temperature given the following specific ranges of hypothermia: >32° to 35°C? 30° to 32°C? <30°C? Degree of Hypothermia Method of Rewarming >32° to 35°C Blankets 30° to 32°C IV infusions <30°C Peritoneal lavage with heated dialysate What are four major causes of hyperthermia (temperature >40°C) in the comatose patient? Acute bacterial Meningitis/encephalitis Massive pontine hemorrhage Aneurysmal subarachnoid hemorrhage Traumatic head injury (via direct compression, ischemia, or contusion of hypothalamus) What are five major causes of hypothermia (temperature <35°C) in the comatose patient? Exposure to cold environment Systemic illness Intoxication Traumatic brain injury (systemic sign of brain death) Acute spinal cord transection Mydriasis can indicate what common conditions and drug use? Dilated pupils can be seen in: 1. Anxiety 2. Delirium 3. Pain 4. Seizures 5. Botulism Drugs: 1. Atropine 2. Amyl nitrate 3. Magnesium excess 4. Norepinephrine 5. Tetracycline overdose 6. Aminoglycoside 7. Dopamine Persistent or unexplained surges of hypertension in the comatose patient can indicate what condition? Potential poisoning or overdose of various drugs, including amphetamines, cocaine, phenylpropanolamine, hallucinogens, and sympathomimetics What are complications of alcohol (ETOH) intoxication/overdose? 1. Reduced arousal (depressant effects) 2. Fatality (see below) 3. Ataxia, dysarthria, increased reaction time, euphoria, loss of judgment, loss of inhibition, aggression, irritability 4. Seizures (typically secondary to hyponatremia, rarely a direct result of ethanol intoxication) 5. Stupor and coma What is the management for a patient in a stupor or coma from ethanol intoxication? 1. Endotracheal intubation to protect airway 2. IV thiamine 3. Rewarming as needed 4. Adequate hydration 5. Prevention of recurrent seizures (if present) 6. Management and continual reassessment of hypoglycemia Bullae and/or excoriated blisters in the comatose patient can indicate an overdose of what class of drugs? Barbiturates In barbiturate overdose, what often determines the time spent on mechanical ventilation? The duration of action of the agent. Below are common barbiturate and their duration of action: Ultrashort-acting (0.3 hour): 1. Thiopental 2. Thiamylal 3. Methohexital Short-acting (3 hours): 1. Hexobarbital 2. Pentobarbital (“Yellow Jackets”) 3. Secobarbital (“Red Devils”) Intermediate-acting (3–6 hours): 1. Amobarbital (“Blue Heavens”) 2. Aprobarbital 3. Butabarbital Long-acting (6–12 hours): 1. Barbital 2. Mephobarbital 3. Phenobarbital (“Purple Hearts,” “Goofballs,” “Downs”) 4. Primidone What is the presentation of a barbiturate coma? 1. Flaccid coma with initially small reactive pupils that progress to nonreactive, dilated pupils in near-fatal doses 2. Profound hypotension from direct myocardial depression and clammy skin with hypothermia can also be seen. 3. “Coma blisters,” which are bullous skin lesions, can be present at pressure points. How can the depth of a barbiturate coma be estimated? 1. Measurement of barbiturate levels 2. EEG, which can show isoelectric tracing in severe cases that mimics brain death, but more commonly shows a burst suppression pattern What is the management of barbiturate-induced coma? Supportive: full mechanical ventilation until cough reflexes return, vasopressors (i.e., dopamine) to support BP, and hemodialysis if indicated in long-acting barbiturate ingestion What should you suspect if coma is mixed with abnormalities in the ECG? Have a low threshold to suspect tricyclic antidepressant (TCA) overdose What are the most common ECG findings with TCA overdose? Sinus tachycardia Atrioventricular (AV) block (first-degree) Bundle or branch block (wide QRS)8,9 What is one of the primary causes of death in the ICU setting related to drug overdosing? TCA overdose With what skin and vital sign manifestations does TCA overdose present? Dry skin, tachycardia, fever, and cardiac arrhythmias; ECG changes can be present. What is the main toxicity of TCAs that results in rapid death? Cardiotoxicity as a result of: 1. Impaired contractility (due to inhibition of Na+ channels) 2. Hypotension (due to vasodilation and norepinephrine depletion)8,9 What is the extreme presentation (short of death) of TCA overdose? Loss of all brainstem reflexes and apnea, a condition mimicking brain death What is the management of TCA overdose? 1. GI decontamination with activated charcoal10 2. Administer sodium bicarbonate (50 mEq NaHCO3, 1 mEq/mL) to produce alkalosis to inhibit Na+ channel blockade by TCAs10,11 3. Seizure prevention and treatment At what level is lithium toxicity serious? 2.5 mEq/L What is the management? Restoration of sodium and water balance that has been dysregulated due to Li-induced nephrogenic diabetes insipidus and immediate hemodialysis or peritoneal dialysis12 What is the common presentation of benzodiazepine overdose? Coma and extreme flaccidity What is the management of benzodiazepine overdose? Flumazenil13,14 and supportive measures (respiratory support if needed based on pulse oximeter) What is the presentation of phencyclidine intoxication? Lack of pain sensation, hypertension, tachycardia, salivation, sweating, bidirectional nystagmus, bizarre behavior, endless speech, violence and aggression, vivid visual hallucinations, catatonia, rhabdomyolysis, deep anesthesia and coma (with cholinergic signs of frothing, flushing, miosis)15 What is the management of phencyclidine intoxication? Respiratory support (ventilator); chronic users can go through withdrawal that is schizophrenia-like. What is the presentation of cocaine intoxication? Hypertension, dilated pupils, tachypnea, seizures that can progress to generalized tonic-clonic status epilepticus, and coma What is the management of cocaine intoxication? Cooling blankets or fans to manage hyperthermia, beta-blockers or lidocaine for ventricular tachycardia, and monitor for acute MI and status epilepticus What is the presentation of opiate overdose? Miosis, hypoventilation, flaccidity; may have loss of brainstem reflexes, and pupillary light reflexes can be hard to discern16 Which two opiates can lower the seizure threshold? Meperidine and propoxyphene What is the management of opiate overdose? 1. Naloxone (Narcan) or naltrexone. Both are opioid antagonists and result in rapid reversal of coma. 2. Supportive measures (don’t forget ABCs to monitor hypoxia and hypercapnia from hypoventilation). What is the presentation of cyanide poisoning? Hypoventilation, severe lactic acidosis, bradycardia, hypotension, rapidly developing pulmonary edema, coma, and “bitter almond” or a musty smell17 What is the management of cyanide poisoning? Treat with Lilly™ cyanide antidote kit (Eli Lilly, Indianapolis, IN). This contains amyl nitrite, sodium nitrite, and sodium thiosulfate (IV 50 mL of 25% solution). Bilateral necrosis of the putamen is highly characteristic of ingestion of what toxic alcohol? Methanol What is the presentation of methanol intoxication? Latency period of up to 12 hours, followed by sudden lapse into coma. Restlessness, vomiting, “fetal positioning” from abdominal cramps, and seizures can precede coma.18 What is the management of methanol intoxication? Management: treat acidosis with bicarbonate and dialysis for comatose patients. A patient presents to the ER after a suicide attempt by consuming antifreeze. Describe his likely presentation. Ethylene glycol is the major component of antifreeze. Presentation: gait ataxia, nystagmus, paralysis of extraocular muscles, ocular bobbing, generalized tonic-clonic seizures or profound myoclonus, tetanic contractions from hypocalcemia, lactic acidosis, and osmolar gap.18 What is the management of the above patient? Confirm diagnosis with finding of calcium oxalate crystals in urine. Treat by hemodialysis and large amounts of ethanol (even up to intoxication levels, 1000 μg/mL target level). Fomepizole can be used in the place of ethanol.19 A patient presents to the ER with rapid onset of coma and acetone breath. What is the likely toxic poisoning? What is your next step? Isopropyl alcohol Begin gastric lavage after ruling out DKA (diabetic ketoacidosis). What is the presentation of salicylate ingestion? Restlessness, hyperventilation, hyperthermia, purpura (due to platelet dysfunction), pulmonary edema, severe academia, increased anion gap, metabolic acidosis, respiratory alkalosis20 What is the management of salicylate ingestion? Measurement of serum salicylate levels or ferric chloride testing of urine (purple color is diagnostic). A plasma level of 6 mg/dL is typical in patients with seizures and coma. What is the management? Gastric lavage, activated charcoal, and forced alkaline diuresis with sodium bicarbonate or acetazolamide promotes excretion21 What is the antidote for acetaminophen? N-acetylcysteine22 What are the clinical manifestations of toxic levels of phenytoin (>50 μg/mL)? Ataxia, dysarthria, combative behavior, hallucinations, and rarely generalized tonic-clonic seizures that progress to flaccid coma23 What is the appropriate management? Supportive: ventilator for respiratory support and charcoal to minimize further absorption (if necessary); lorazepam or phenobarbital if seizures have occurred What is the “coma cocktail” composed of? Hypertonic dextrose, thiamine hydrochloride, naloxone hydrochloride, and flumazenil24,25 What are the possible complications? Naloxone and flumazenil have the major complication of possible aspiration during the rapid arousal from coma. Naloxone also has a withdrawal syndrome associated.25 Flumazenil can result in seizures when high doses are administered.24 If focal neurological signs are present in a comatose patient with fever and meningeal irritation, what three steps should be taken? This is a comatose patient with infectious disease, evident by fever and meningeal irritation. The focal neurological signs warrant the following investigations: 1. Immediate IV antibiotics 2. CT scan to rule out abscess 3. Lumbar puncture and culture to identify organism True or false: Meningeal irritation is easily assessed in patients in deep coma. False. Meningeal irritation is less apparent in patients in deeper stages of coma. What are the three major determinants of outcome in nontraumatic coma? 1. Underlying cause 2. Severity 3. Duration What cause of coma carries the worst prognosis, with a mortality rate greater than 70%? Cerebrovascular disease, including hemorrhagic and ischemic syndromes Fat emboli from long bone fracture What are “raccoon eyes” and Battle’s sign and what do they suggest? Raccoon eyes are periorbital ecchymosis and Battle’s sign is retroauricular ecchymosis. They are suggestive of midface/anterior cranial fossa or middle cranial fossa fractures, respectively. In a patient in whom alcoholism can play a role in the cause of coma, what should accompany glucose infusion to prevent precipitation of acute Wernicke’s encephalopathy? 100 mg IV thiamine administered slowly over 5 minutes or intramuscularly. Thiamine should not be used unless this is a potential cause of coma because acute anaphylactic reactions and acute pulmonary edema have been reported with its use. Why is the immediate infusion of IV acyclovir important in comatose patients when herpes encephalitis is suspected? Outcome is largely determined by early treatment. Full recovery, however, is unlikely in most patients in stupor or coma. Profound hypertension can result in what CNS problem? Diffuse encephalopathy. It can occur with documented seizures and papilledema, which are often preceded by visual hallucinations. What is PRES? Posterior reversible encephalopathy syndrome What is the typical constellation of symptoms in PRES? The clinical spectrum typically includes headaches, seizures, altered mental status, and visual complaints that can progress to a comatose state. What is the suggested physiopathology? Hypertension as a cause for predominantly posterior circulation vascular dysautoregulation Why does this occur predominantly in the posterior circulation? Suggested to be due to lower density of sympathetic supply of the posterior circulation What are the frequent causes of PRES? Hypertensive encephalopathy Eclampsia and preeclampsia Immunosuppressive drugs Miscellaneous (postoperative, infectious) What are the most relevant radiological findings of PRES? Vasogenic edema predominantly in parieto-occipital areas, but other lobes, deep white matter, basal ganglia, and infratentorial structures can be affected. What is the correct management of PRES? Adequate blood pressure control, and suppress the causative agent (drugs, infection) 1. Suarez J. Critical Care Neurology and Neurosurgery. Totowa, NJ: Humana Press, 2004 3. Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: The FOUR score. Ann Neurol 2005;58:585–593 PubMed 4. Wijdicks EF. Neurologic complications in critically ill patients. Anesth Analg 1996;83:411–419 PubMed 5. Wijdicks EF, Cranford RE. Clinical diagnosis of prolonged states of impaired consciousness in adults. Mayo Clin Proc 2005;80:1037–1046 PubMed 6. Zandbergen EG, de Haan RJ, Stoutenbeek CP, Koelman JH, Hijdra A. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet 1998;352:1808–1812 PubMed 7. Prockop LD, Chichkova RI. Carbon monoxide intoxication: an updated review. J Neurol Sci 2007;262:122–130 PubMed 8. Bradberry SM, Thanacoody HK, Watt BE, Thomas SH, Vale JA. Management of the cardiovascular complications of tricyclic antidepressant poisoning: role of sodium bicarbonate. Toxicol Rev 2005;24:195–204 PubMed 9. Thanacoody HK, Thomas SH. Tricyclic antidepressant poisoning: cardiovascular toxicity. Toxicol Rev 2005;24:205–214 PubMed 10. Haddad LM. Managing tricyclic antidepressant overdose. Am Fam Physician 1992;46:153–159 PubMed 11. Miller J. Managing antidepression overdoses. Emerg Med Serv 2004;33:113–119 PubMed 12. Waring WS. Management of lithium toxicity. Toxicol Rev 2006;25:221–230 PubMed 13. Hoffman EJ, Warren EW. Flumazenil: a benzodiazepine antagonist. Clin Pharm 1993;12:641–656, quiz 699–701 PubMed 15. Brust JC. Other agents. Phencyclidine, marijuana, hallucinogens, inhalants, and anticholinergics. Neurol Clin 1993;11:555–561 PubMed 16. Foley KM. Opioids. Neurol Clin 1993;11:503–522 PubMed 17. Borron SW. Recognition and treatment of acute cyanide poisoning. J Emerg Nurs 2006;32(4, Suppl)S12–S18 PubMed 18. Jammalamadaka D, Raissi S. Ethylene glycol, methanol and isopropyl alcohol intoxication. Am J Med Sci 2010;339:276–281 PubMed 19. Mégarbane B, Borron SW, Baud FJ. Current recommendations for treatment of severe toxic alcohol poisonings. Intensive Care Med 2005;31:189–195 PubMed 20. Pearlman BL, Gambhir R. Salicylate intoxication: a clinical review. Postgrad Med 2009;121:162–168 PubMed 21. Sallis RE. Management of salicylate toxicity. Am Fam Physician 1989;39:265–270 PubMed 22. Brok J, Buckley N, Gluud C. Interventions for paracetamol (acetaminophen) overdoses. Cochrane Database Syst Rev 2002; 3:CD003328 PubMed 23. Craig S. Phenytoin poisoning. Neurocrit Care 2005;3:161–170 PubMed 24. Bartlett D. The coma cocktail: indications, contraindications, adverse effects, proper dose, and proper route. J Emerg Nurs 2004;30:572–574 PubMed 25. Hoffman RS, Goldfrank LR. The poisoned patient with altered consciousness. Controversies in the use of a ‘coma cocktail’. JAMA 1995;274:562–569 PubMed
Coma
32.1 Basic Concepts: Consciousness
32.2 Grades of Consciousness
32.3 Electrolyte/Metabolic
32.4 Structural Coma
32.5 Hypoxic Injury
32.6 Temperature
32.7 Drugs/Toxins
32.8 Infectious
32.9 Miscellaneous
32.10 Encephalopathic Coma
References
Coma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






