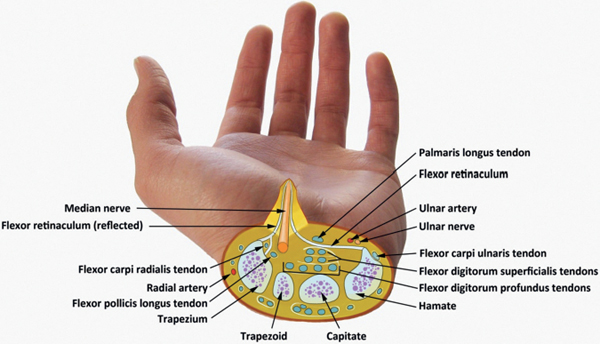
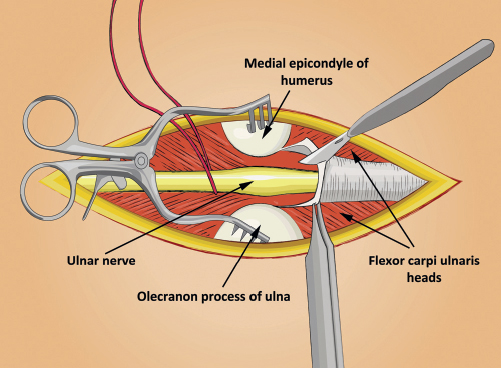
68 What is the most likely pathophysiology of idiopathic nerve compression? Mechanical obstruction of venous return from the nerve secondary to local anatomy leads to venous congestion, circulatory compromise, and relative anoxia. Clinical corollary: patients with carpal tunnel syndrome (CTS) who are able to “shake off” paresthesias when awakened from sleep. Over time, persistent endoneurial edema induces fibrosis, which acts as a barrier to exchange of oxygen and nutrients within the nerve, causing loss of axonal transport and demyelination.1 What are the known anatomical sites of median n. compression? The median n. is formed from contributions of both the medial and lateral cords (C5-T1). It travels with the brachial artery extending medially as it descends toward the cubital fossa. 1. Distal third of humerus beneath supracondylar process and the ligament of Struthers 2. In antecubital fossa, deep to bicipital aponeurosis 3. In forearm, between ulnar and humeral heads of the pronator teres 4. Underneath the aponeurotic arch of the FDS 5. In carpal tunnel, underneath the transverse carpal ligament What is supracondylar process syndrome? Rare entrapment of the median nerve at the distal humerus under the ligament of Struthers. Patients present with localized aching pain referable to the elbow. Pronator teres weakness distinguishes this syndrome from more distal entrapments. Treatment consists of sectioning the ligament of Struthers.4 General term describing entrapment of the median nerve at any of the three known sites in the elbow What are the signs of pronator syndrome? Symptoms include pain over the volar surface of the proximal arm and forearm as well as diminished sensation in the radial 3½ digits. Symptoms are less commonly noted at night and are often exacerbated by provocative maneuvers (including elbow flexion). Phalen’s and Tinel’s tests at the wrist are notably negative. Operative release involves detailed exploration of all potential sites of compression. Which structures form the boundaries of the carpal tunnel? • Roof: thick fibrous transverse carpal ligament • Radial: transverse carpal ligament (TCL) attaches to scaphoid tuberosity and part of trapezium. • Ulnar: TCL attaches proximally to the pisiform and distally to the hook of the hamate. • Floor: Carpal bones and deep volar radiocarpal and volar interosseous ligaments What are the contents of the carpal tunnel? The median n. and the nine digital flexor tendons (FDS, FDP, and FPL) Fig. 68.1 Median nerve decompression in the carpal tunnel. What systemic conditions are associated with carpal tunnel syndrome? Female gender, family history, diabetes, renal failure, obesity, rheumatoid arthritis, polymyalgia rheumatica, menopause, oral contraceptive use, pregnancy, acromegaly, hyper/hypothyroidism, amyloidosis, prior Colles’ fracture5 What are the presenting symptoms of carpal tunnel syndrome? Patients most commonly present with paresthesias and pain over the distal median n. distribution. Symptoms are particularly worse at night. If longstanding, may also have weakness and atrophy of the thenar musculature.6 Name three provocative maneuvers for the diagnosis of carpal tunnel syndrome. Phalen’s test, Tinel’s sign, and carpal tunnel compression test What is Phalen’s test? Complete and forced flexion of the wrist (typically for about 1 minute). A positive test involves recurrence of typical symptoms. How is carpal tunnel syndrome treated? A trial of conservative management (wrist splinting, avoidance of exacerbating postures/activities, medications such as antiinflammatories) is warranted for mild/moderate CTS prior to considering surgery. Open or endoscopic release involves division of the transverse carpal ligament over its entire extent.7 What are the known anatomical sites of ulnar n. compression? The ulnar n. is the main continuation of the medial cord and consists of C7-T1 roots. It travels medial to the brachial artery down until it pierces the medial intermuscular septum at the mid-arm level. The anatomical sites are as follows: 1. At the arcade of Struthers, located approximately 8 cm proximal to the medial epicondyle 2. If the nerve subluxes anteriorly, it can be compressed by the edge of the thick medial intermuscular septum. 3. Under a subluxing medial head of the triceps 4. Within the cubital tunnel between the olecranon and medial epicondyle and underneath the transversely extending Osborne’s ligament (which joins the two heads of the FCU); this is the most common site of entrapment. 5. Under a fascial arcade formed by the two heads of the FCU 6. In Guyon’s canal What is the difference between the ligament of Struthers and the arcade of Struthers? The ligament of Struthers extends from the supracondylar process of the distal humerus to the medial epicondyle and forms a potential site of compression of the median n. and brachial artery. The arcade of Struthers is a fascial arcade of the intermuscular septum that the ulnar n. traverses on its course from the anterior to the posterior compartment of the arm. Which structures form the boundaries of the cubital tunnel? • Anterior: medial epicondyle • Lateral and floor: elbow joint and medial collateral ligament • Medial: heads of the FCU origin • Roof: Osborne’s ligament (extends from medial epicondyle to the olecranon) What is cubital tunnel syndrome? Represents the second most common upper extremity entrapment neuropathy. It occurs from compression of the ulnar nerve as it passes through the fibro-osseous cubital tunnel. More common in men (3:1 ratio).8 How does cubital tunnel syndrome present? Insidious onset of paresthesias/numbness over ulnar border of forearm, hand, and 4th and 5th digits. Hand weakness/clumsiness (“difficulty buttoning shirt”). May see hypothenar atrophy. May also complain of pain over medial elbow. How is cubital tunnel syndrome treated? Conservative management warranted with mild symptoms and no atrophy (elbow pad, avoidance of precipitating positions). However, threshold for operative intervention should be lower than with CTS as only approximately 15% improve spontaneously. Operative options include in-situ decompression ± subcutaneous or submuscular transposition, and medial epicondylectomy. Still controversial whether functional outcomes significantly different among various procedures.9 Fig. 68.2 Ulnar nerve decompression in the cubital tunnel.
Common Entrapment Neuropathies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






