Complications Related to the Management of Odontoid Fractures
Paul Kraemer
Rick C. Sasso
Care of the patient with an odontoid fracture continues to be fraught with difficulty. Complications may arise during diagnosis, nonoperative management, decision-making regarding operative management technique, or by execution of the chosen surgical method. As our society ages, the special dilemma and specific complications of elderly patients with dens fractures is becoming more common. This chapter outlines the range of complications related to the management of odontoid (dens) fractures and offers guidance to minimize the impact and frequency of possible complications.
ANATOMY
Many complications related to the management of dens fractures stem from an underappreciation of the complex anatomy of the occipitocervical junction. The upper cervical spine represents a transition zone between the rigid skull base and the mobile cervical spinal column. It consists of the occiput and paired occipital condyles, the foramen magnum, C1 (atlas), C2 (axis), and an interconnected array of stabilizing ligaments. As a result, C2 fractures should be viewed not as an isolated bony injury but as an injury of the occipitocervical junction.
The odontoid process extends as a vertical post from the body of the axis and serves as the primary bony stabilizer of the atlantoaxial complex. It articulates with the dorsal aspect of the ventral arch of the atlas through a synovial joint. The C1-C2 facet joints, in conjunction with the odontoid, form a unique architecture, which allows about 50% of all cervical axial rotation and 12% of cervical flexion/extension (1).
Embryologic development of the axis is also complex. Three different sclerotomes contribute to C2. The lowest occipital sclerotome (proatlas) forms the tip of the dens, whereas the body of the C1 sclerotome separates during ontogeny to join with the axis, forming the odontoid process. Finally, the C2 sclerotome forms the remaining body of the axis.
The primary ligamentous stabilizers of the occipitocervical complex include the transverse atlantal ligament (which passes immediately dorsal to the dens and attaches to tubercles on the inner aspect of each lateral mass of the atlas) and the tectorial membrane (a continuation of the posterior longitudinal ligament, attaching to the ventral aspect of the foramen magnum). Accessory ligaments include the paired alar ligaments (attaching the superior lateral aspect of the dens to the inner aspect of the occipital condyles) and the rudimentary apical ligament (attaching the tip of the dens to the ventral margin of the foramen magnum).
A thorough understanding of the bony anatomy of the dens is particularly important to avoid complications of ventral or dorsal instrumentation. Histomorphometric analysis has revealed high-density trabecular bone located in the center tip of the dens as well as in the weight-bearing lateral masses beneath the superior facets. The ventral base of the body of C2, where the anterior longitudinal ligament attaches, is composed of thickened cortical bone. However, the upper portion of the C2 body and the base of the dens consist of relatively weaker, fine trabecular bone (2). Because bone quality is a crucial determinant of screw purchase, these factors affect direct odontoid fracture fixation (3). Optimal ventral odontoid screw placement requires strong purchase at the entry point (ventral-caudal border of C2 body) and distal point of fixation (odontoid tip), traversing the weak, hypodense bone in the body of C2. If the entry site is too cephalad along the ventral body of C2, the screw may cut out of this weak bone. If the screw does not engage the cortical bone at the tip of the dens, poor purchase of the dens fragment may result.
The projection angle of the odontoid is the most variable anatomic dimension of the axis, ranging from -2 degrees (tilting ventrally) to 42 degrees (tilting dorsally), with a mean of 13 degrees (4). This variability can make the assessment of fracture reduction difficult. The diameter of the odontoid may be less than 6 mm, preventing placement of two 3.5-mm ventral odontoid screws (4,5). Patient body size correlates poorly as a predictor of the odontoid size (6).
The vascular supply of the odontoid is provided primarily by the paired right and left dorsal and ventral ascending
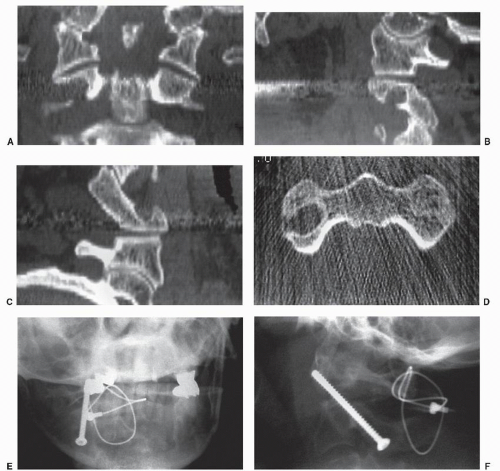
arteries of the axis, which are branches of the vertebral arteries between the second and third cervical vertebrae (7). These also anastomose with horizontal arteries from the internal carotid arteries, forming a rich local vascular network, leading some investigators to conclude that an odontoid fracture nonunion is not primarily due to an inadequate vascular supply (8,9). On the axis, the vertebral artery groove is located near the pars, along the inferior portion of the superior facet. Because the C2 body is relatively narrow compared to the subaxial vertebrae, the vertebral artery enters more medially in the axis, ultimately traveling laterally as it heads rostral into the transverse foramen of the atlas. Paramore et al. (10) showed that up to 18% of patients have unilateral anomalous vertebral artery locations, forming a high-riding transverse foramen that substantially narrows the pedicle and lateral mass of C2. This effectively precludes safe placement of a dorsal C1-C2 transarticular screw on the affected side (Fig. 105.1).
arteries of the axis, which are branches of the vertebral arteries between the second and third cervical vertebrae (7). These also anastomose with horizontal arteries from the internal carotid arteries, forming a rich local vascular network, leading some investigators to conclude that an odontoid fracture nonunion is not primarily due to an inadequate vascular supply (8,9). On the axis, the vertebral artery groove is located near the pars, along the inferior portion of the superior facet. Because the C2 body is relatively narrow compared to the subaxial vertebrae, the vertebral artery enters more medially in the axis, ultimately traveling laterally as it heads rostral into the transverse foramen of the atlas. Paramore et al. (10) showed that up to 18% of patients have unilateral anomalous vertebral artery locations, forming a high-riding transverse foramen that substantially narrows the pedicle and lateral mass of C2. This effectively precludes safe placement of a dorsal C1-C2 transarticular screw on the affected side (Fig. 105.1).
BIOMECHANICS
The great mobility of the atlantoaxial articulation results in substantial forces being imparted to the odontoid, especially at the extremes of motion. Human cadaveric testing has demonstrated that dens fractures occur as a result of a combination of horizontal shear and vertical compression force (8). When the shear component is applied in a direct sagittal plane (extension), a type III fracture pattern is created (11). Mouradin et al. (12) believed this was due to simultaneous forces exerted by the alar, apical, and tectorial membrane ligaments. When the shear force is applied more obliquely (laterally), a type II fracture occurs, possibly owing to the lateral mass of the atlas impinging on the base of the odontoid (11,12). A forward flexion moment, with resultant ventral displacement, is believed to account for 60% to 80% of odontoid fractures (13, 14 and 15). Similarly, an extension moment has been shown to lead to dorsal displacement, found more commonly among elderly patients (14—17).
A finite element model of the occipitoatlantoaxial complex predicts that force loading with the head in extension, coupled with lateral shear or compression, leads to a type I fracture (18). This finite element analysis also showed that axial rotation and lateral shear can produce type II fractures. Moreover, flexion provided a protective mechanism against force application that would otherwise cause a higher risk for odontoid failure (18).
The biomechanics of dens fracture internal fixation deserves special attention. The strength of the ventral dens screw construct is dependent on the interdigitation of the fracture fragments. An anatomically reduced fracture with the fracture fragments maximally lagged together provides stability in excess of the isolated strength of the screw. It is thus very important to ensure that anatomic reduction is present if internal fixation is performed. Even 1 mm of displacement profoundly diminishes the surface area available for interdigitation. Also, it is important that the fracture fragments are strongly lagged together. This can be done by a lag technique with the body fragment overdrilled to the outer diameter of the screw or by using a partially threaded screw. If a partially threaded “lag” screw is used, however, it is important that all of the threads be in the odontoid fragment to ensure compression across the fracture.
EPIDEMIOLOGY
Odontoid fractures represent a common spinal injury, constituting nearly 60% of axis fractures and 7% to 18% of all traumatic cervical spine fractures. Despite their relative frequency, significant controversy remains regarding appropriate surgical and nonsurgical treatment options in the management of these injuries.
Because there is a proportionally greater amount of space available for the spinal cord in the upper cervical spine, the reported prevalence of neurologic deficit in dens fractures is relatively low (18% to 26%). Neurologic injuries can range from greater occipital nerve injury (C2 nerve root) to a high tetraparesis with respiratory dysfunction (15,16,19,20).
Although dens fractures occur in all age groups, there tends to be a bimodal distribution, with a mean age of 47 years. In younger patients, this injury is usually secondary to high-energy trauma, with motor vehicle crashes being the most common cause (15,19,20). Among this group, concomitant spinal injuries are present in up to 34% of patients. Of the concomitant fractures, 85% occur in the cervical spine, with the atlas being the most common second injury site (16,21,22). A frequent source of complications related to the management of dens fractures is either missing a noncontiguous spinal injury or not appreciating the severity of a contiguous injury. Atlas fractures and transverse atlantal ligament injuries in particular are major factors in the prognosis and treatment options for type II dens fractures.
Dens fractures are even more common among the elderly, accounting for the second prevalence peak (23). Although the prevalence of subaxial spine fractures decreases with age, frequency of dens fractures increases with age (24), representing the most common cervical spine fracture in patients older than 70 years (17,25, 26 and 27). These injuries are usually the result of low-energy trauma, such as ground-level falls in which the forehead strikes an object resulting in a hyperextension injury. In these instances, associated spinal trauma is much less common (21,28).
CLASSIFICATION
The most widely used classification system for dens fractures is that of Anderson and D’Alonzo (20). This system divides fractures into three types based on the anatomic location of the fracture. Type I is a small, oblique fracture of the tip of the dens, believed to be due to avulsion by the alar ligament. This may be confused with an ossiculum terminale, a congenital anomaly in which the previously discussed proatlas fails to fuse with the dens. This is a rare fracture pattern, accounting for 1% to 5% of dens fractures, with some authors doubting its existence. However, if present, it may be associated with an atlantooccipital dislocation (29). Type II is the most common (38% to 80%), a horizontal fracture occurring transversely across the junction of the odontoid process with the C2 body. Hadley and colleagues proposed an additional IIA subtype, defined as a type II fracture with marked comminution at the base, due to its inherently increased instability (30). Finally, a type III fracture extends into the body of C2, accounting for 15% to 40% of all dens fractures.
The Anderson and D’Alonzo (25) classification has remained popular due to its anatomic simplicity and correspondence with treatment methods and outcomes. Nonetheless, it appears to be susceptible to issues of interobserver agreement, especially when based on plain radiography rather than reformatted computed tomography (CT) scans, particularly mistaking high type III fractures for a type II (31).
ERRORS IN EVALUATION
Initial evaluation and management of patients with suspected odontoid process fractures is identical to that of many cervical spine trauma patients. This includes
employing early cervical orthosis immobilization (usually with a rigid cervical collar) and maintaining spinal immobilization during airway management and particularly during transfers for radiographic evaluation. A halo traction ring or a Gardner-Wells tong may be placed to apply 10 to 15 pounds of traction (starting with 5 to 10 pounds and radiographically verifying that occipitocervical instability is not present). This is particularly useful if there is displacement of the dens in order to obtain reduction and to verify that closed reduction, in fact, can be accomplished. If it cannot be reduced with adequate traction and surgery is contemplated, this may preclude some instrumentation options, such as a ventral dens screw or dorsal C1-C2 transarticular screws. If a halo ring or tongs are applied before complete imaging, magnetic resonance imaging (MRI)-compatible devices should be chosen as MRI may be required to assess for associated upper cervical ligamentous injury or cord compression/contusion.
employing early cervical orthosis immobilization (usually with a rigid cervical collar) and maintaining spinal immobilization during airway management and particularly during transfers for radiographic evaluation. A halo traction ring or a Gardner-Wells tong may be placed to apply 10 to 15 pounds of traction (starting with 5 to 10 pounds and radiographically verifying that occipitocervical instability is not present). This is particularly useful if there is displacement of the dens in order to obtain reduction and to verify that closed reduction, in fact, can be accomplished. If it cannot be reduced with adequate traction and surgery is contemplated, this may preclude some instrumentation options, such as a ventral dens screw or dorsal C1-C2 transarticular screws. If a halo ring or tongs are applied before complete imaging, magnetic resonance imaging (MRI)-compatible devices should be chosen as MRI may be required to assess for associated upper cervical ligamentous injury or cord compression/contusion.
A comprehensive diagnostic approach in the assessment of suspected upper cervical spine injuries remains controversial, particularly in the presence of polytrauma or an obtunded patient. Initial cervical spine imaging typically consists of the three-view trauma series: anterodorsal, lateral, and open-mouth view radiographs (32). This series reveals 65% to 90% of axis fractures (33, 34 and 35). Several studies have demonstrated that the anteroposterior view provides little additional information (36,37). As noted previously, careful evaluation of the entire upper cervical and subaxial spine is required because of the substantial prevalence of associated spinal injuries (16,21,22,32). Some studies have reported up to a 16% rate of noncontiguous fractures (38).
Thin-slice helical CT scanning has been shown to be the best study for evaluating C2 bony injuries in patients with inadequate plain films and for differentiating acute dens fracture from chronic nonunion and congenital anomalies (39,40). This imaging study has been found to be more sensitive than plain films in the C1-C2 area, which is the location of most initially undetected cervical fractures (40). CT scanning has also been shown to improve the reliability of dens fracture classification (31). However, CT scans may underestimate soft tissue and associated ligamentous injuries.
MRI, like CT, has been shown to be more sensitive than radiographs in revealing some forms of subtle C2 trauma and is especially effective in assessing ligamentous structures (40, 41 and 42). In one recent review, 10% of all dens fracture patients had an associated transverse atlantal ligament disruption (42). Evaluating the integrity of the transverse atlantal ligament in dens fractures is important because its incompetence alters treatment options and substantially increases the risk for dens nonunion (42). While ventral dens screw fixation may achieve osseous union in these patients, it will not restore atlantoaxial stability, leading the surgeon toward atlantoaxial arthrodesis as the most appropriate treatment option in order to avoid neurologic injury.
TREATMENT
A variety of treatment methods are available for management of dens fractures, both surgical and nonsurgical. These include rigid cervical orthoses, SOMI (skull, occiput, mandibular immobilization) and Minerva jackets, halo vest orthoses, ventral dens screw fixation, and dorsal atlantoaxial arthrodesis (AAA). Specific treatment choice should be guided by a number of factors, including fracture type, presence of associated injuries, patient age, and medical comorbidity.
TYPE I
The rare type I fracture is a stable injury, with several of the accessory ligaments remaining intact, including the transverse atlantal ligament. Isolated type I fractures may be managed by simple cervical collar immobilization. Initial assessment, however, should include careful evaluation for possible association with an occipitoatlantal dislocation (19, 20 and 21,29). Devastating neurologic complications may occur if occipitocervical instability is overlooked.
TYPE III
Because of their large cancellous fracture surface, type III injuries generally heal uneventfully with nonoperative management, provided adequate reduction is maintained (16). Immobilization in a halo vest or rigid cervical orthoses for 8 to 14 weeks has been reported to result in successful union in 92% to 100% of cases (20,22,43,44). Clark and White (15), however, described a nonunion rate of up to 13% for these fractures, with a trend toward nonunion in fractures with more than 5 mm of displacement. These authors recommended treatment with halo immobilization. Given the less frequent availability of CT scans at the time, this series may have contained a significant number of patients with a high type III fracture subtype, with a shallow base that may act like a type II fracture. These fractures have been reported to have a higher complication rate and increased incidence of nonunion without operative treatment (45).
TYPE II
Despite the relative frequency of type II injuries, their treatment remains highly controversial (24,26). Substantial complications can occur in management of these fractures either operatively or nonoperatively.
Nonoperative Treatment
Nonoperative management yields reported rates of nonunion ranging from 26% to 85% (9,15,19,23,26). Although some studies suggest this high rate of nonunion is secondary to the disruption of the vascular supply to the dens (7), other investigators have demonstrated adequate blood flow from above and below the odontoid base (8,9). Other factors potentially contributing to nonunion include the difficulty of maintaining an adequate fracture reduction of the dens relative to the body of the axis as well as the predominantly intersynovial location of the dens itself (16,25,46). The prevalence of type II fracture nonunion has been shown to correlate with initial displacement of 4 to 6 mm (15,19,47,48), with several studies concluding such displacement to be the most important
single factor in determining the success of nonsurgical management. Other factors including dorsal displacement, patient age over 60 years, delay in diagnosis greater than 3 weeks, and angulation greater than 10 degrees have also been associated with an increased rate of nonunion (9,15,19,22,23,43,48,49).
single factor in determining the success of nonsurgical management. Other factors including dorsal displacement, patient age over 60 years, delay in diagnosis greater than 3 weeks, and angulation greater than 10 degrees have also been associated with an increased rate of nonunion (9,15,19,22,23,43,48,49).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree