Congenital Cervical Deformity
Dheera Ananthakrishnan
Reginald S. Fayssoux
Spinal deformity resulting from abnormal embryonic vertebral development is uncommon in the cervical spine. Consequently, the management of these patients is based on consideration of relevant principles and anecdotal experience rather than a rigorous evidence-based approach. Proper management requires consideration of the presenting chief complaint, the degree of neurologic involvement, the type of vertebral anomaly, the resulting curve pattern, and the potential for curve progression. Evaluation for coexisting abnormalities in other organ systems is also important as these are not uncommon and can have significant clinical implications. In this chapter, the embryology relevant to vertebral formation, the classification of congenital spinal deformity, the natural history of patients with congenital cervical spine deformity, and the principles of evaluation and treatment of these disorders are reviewed.
EMBRYOLOGY
Management of vertebral anomalies requires an understanding of vertebral development. Vertebrae begin forming during the embryonic period of development between 3 and 8 weeks of gestation simultaneous with the development of other major organ systems such as the genitourinary, cardiopulmonary, and nervous systems. The concurrent development of these organs is important because of the potential for concomitant pathology of these organ systems. Genetic factors have an unclear role in the development of spinal anomalies. While a genetic locus on chromosome 8 has been linked to a familial form of Klippel-Feil syndrome, evidence in support of a clear genetic etiology for congenital anomalies is lacking (1). Homeobox genes, a family of genes that regulate differentiation and segmentation of the axial skeleton, may play a role as mutations in this family of genes are thought to be responsible for certain congenital abnormalities of the spine. The true cause of congenital cervical spinal anomalies is likely multifactorial in nature.
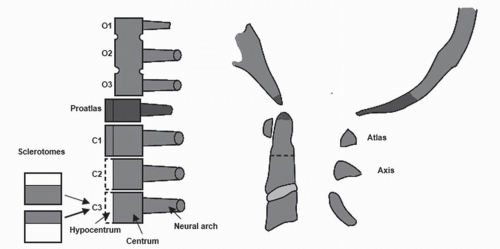
The early embryonic process of neurulation results in the formation of the notochord and adjacent neural tube, the precursors to the spinal column and neural elements, respectively. Mesodermal tissue immediately adjacent to the notochord and developing neural tube organize into primitive divisions referred to as somites by the end of the 3rd week of gestation. Initially, there are 42 somites: 4 occipital, 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 8 to 10 sacrococcygeal pairs. Each somite undergoes further differentiation into their respective dermatome, myotome, and sclerotome by the beginning of the 4th week of gestation, with the sclerotome being ultimately responsible for formation of the vertebral body and dorsal elements. Segmentation of the spinal column occurs after initial development of the sclerotome during the process of metameric shift. Each sclerotome is divided into cranial and caudal halves via formation of the fissure of Ebner. The cells immediately adjacent to the fissure differentiate to become the intervertebral disk. The caudal half of one sclerotome fuses with the cranial half of the next lower adjacent sclerotome to form the centrum, the embryologic precursor to the vertebral body. The anlagen of the neural arch ossify and fuse dorsally to form the complete arch of the dorsal elements. Thus, each vertebra develops from fusion of the cranial and caudal halves of adjacent sclerotomes. Development of the upper cervical spine follows a similar pattern that is slightly more complex because of the unique anatomy of the region (Fig. 90.1)
The cranial and caudal halves of adjacent sclerotomes fuse to form the future vertebral body or centrum. The first four sclerotomes contribute to the craniovertebral junction. Persistence of the hypocentrum of the proatlas forms the basion (tip of the clivus). The centrum of the proatlas becomes the apical dens and its ligaments (apical, alar, and transverse). The neural arch of the dens splits into a dorsal half that forms the foramen magnum and occiput and a ventral half that contributes to the superior atlantal facet joints. Persistence of the hypocentrum of C1 forms the anterior arch of the atlas. The caudal half of the fourth occipital sclerotome, the proatlas, forms the basion, occipital condyles, and the cranial half of the dorsal arch of the atlas. The proatlas is also responsible for the cranial tip of the odontoid process; failure of fusion with the first spinal sclerotome results in an ossiculum terminale. The first spinal sclerotome is responsible for the ventral arch of the atlas, the centrum of the atlas that ultimately becomes the odontoid process, and the caudal half of the dorsal arch of the atlas.
This systematic process of organogenesis ultimately results in the fully segmented spinal column. Anomalies
occur when these orderly and systematic process go awry. A variety of spinal conditions can result, including occipitocervical synostosis, hypoplasia of the atlas, odontoid anomalies, wedge and hemivertebrae, and Klippel-Feil syndrome.
occur when these orderly and systematic process go awry. A variety of spinal conditions can result, including occipitocervical synostosis, hypoplasia of the atlas, odontoid anomalies, wedge and hemivertebrae, and Klippel-Feil syndrome.
CLASSIFICATION
Classification of congenital cervical spinal deformity is based on the type of anomaly present and the pattern of deformity that results (1). Anomalies may be divided into failures of formation and failures of segmentation, both resulting from disruption of the normal sequence of events that occur during somitogenesis.
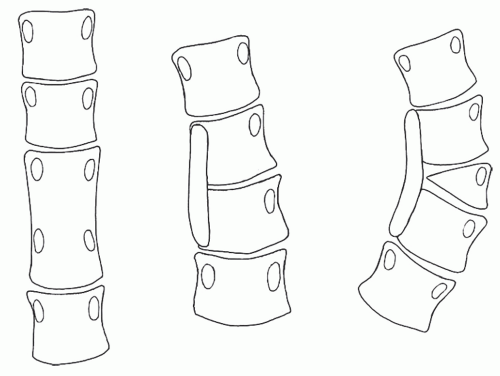
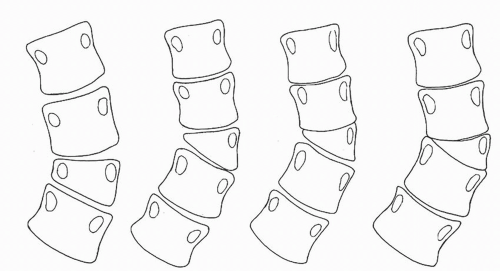 Figure 90.2. Failure of formation anomalies. These include, from left to right, wedge vertebra, fully segmented hemivertebra, partially segmented hemivertebra, and unsegmented hemivertebra. |
Failures of formation are the more common type with the most common anomaly being a hemivertebra (Fig. 90.2). Failure of formation anomalies result from abnormal growth potential due to an area of missing bone in the involved area of the spine. These can be partial failures of formation (e.g., wedge vertebrae) or complete failures of formation (e.g., hemivertebrae).
Failures of segmentation result from absent growth potential due to missing growth plates in the involved area of the spine (Fig. 90.3). Bilateral involvement results in formation of a block vertebra. Unilateral involvement results in the formation of a vertebral bar, which can act as a tether and prevent normal longitudinal spinal growth. The resulting asymmetry from unchecked growth of the nontethered segments may manifest as spinal deformity.
The type of deformity that develops depends on the type and location of the anomaly within the cervical spine. Unilateral anomalies can result in coronal curvatures (i.e., scoliosis). Ventral or dorsal lesions can lead to sagittal curvatures (i.e., kyphosis or lordosis, respectively). Mixed deformities are common as most anomalies are not purely unilateral, ventral, or dorsal. The level at which anomalies occur plays a role in the type of deformity as well. Anomalies that develop within the upper cervical spine, especially unilateral anomalies, can result in torticollis. Involvement of the subaxial cervical spine can result in shortened necks and abnormal cervical postures. Lesions such as scoliosis and kyphosis at the cervicothoracic junction can result in shoulder asymmetry, chest deformities, and torticollis (2).
NATURAL HISTORY
The potential for progression of deformity is dependent on the age at presentation, the specific anomalies present, the curve pattern, and the degree of curvature. In a study of primary congenital scoliosis with thoracolumbar involvement, McMaster and Ohtsuka (3) found that 11% of congenital spinal deformities were nonprogressive, 14% were slightly progressive, and the remaining 75% were significantly progressive. Although vertebral abnormalities are present at birth, clinical deformities often do not become apparent until curve progression occurs during growth spurts. Patients presenting during these periods of growth should be followed closely for progression. The behavior of the spinal deformity during growth and later life is also dependent on the type of anomaly. The anomalies most commonly associated with progression in the subaxial spine are unilateral bars with contralateral hemivertebra, as in this situation one side is tethered while the other side is free to grow. The incidence of curve progression with this type of anomaly approaches 100% in growing patients and often immediate surgical intervention is recommended. The growth potential of most other anomalies is variable and thus warrant close observation especially through the critical periods of rapid growth during adolescence. In older patients, congenital spinal deformities are commonly an incidental finding. These patients can present with complaints related to degeneration resulting from the abnormal biomechanics related to deformity.
UPPER CERVICAL SPINE
Occipitocervical synostosis or assimilation of the atlas is a failure of segmentation defect involving the proatlas (i.e., fourth occipital sclerotome and the first cervical sclerotome) that results in partial to complete union between the skull and atlas. With complete synostosis, the atlas is “assimilated” into the skull, and only rudimentary vestiges of the atlas can be found. Incomplete unions can result in a progressive torticollis. Generally, occipitocervical synostosis is asymptomatic and diagnosed incidentally. Because the anomaly can result in excessive load transfer to the atlantoaxial motion segment, instability can occur, especially when concomitant segmentation failures of the second and third cervical vertebra exist. A reducible atlantoaxial instability may result that can manifest clinically as torticollis. With time, this instability can become fixed and lead to basilar invagination. These patients may be at increased risk for catastrophic spinal cord injury as fusion of the occipitoatlantal joints transfers the stresses to the
atlantoaxial articulation; consequently, occipitocervical synostosis is a relative contraindication to participation in high-energy contact sports. Pizzutillo et al. (4) found that patients with hypermobility of the upper cervical spine are at increased risk for neurologic problems, whereas those with involvement of the lower cervical spine are at increased risk for early degenerative disease.
atlantoaxial articulation; consequently, occipitocervical synostosis is a relative contraindication to participation in high-energy contact sports. Pizzutillo et al. (4) found that patients with hypermobility of the upper cervical spine are at increased risk for neurologic problems, whereas those with involvement of the lower cervical spine are at increased risk for early degenerative disease.
Hypoplasia of the atlas is a rare failure of formation defect that can be asymptomatic or can result in primary basilar impression, torticollis, or both. Dubousset (5) described three forms of the anomaly. Type I is characterized by an isolated hemiatlas; type II, by partial or complete aplasia of one hemiatlas with congenital fusions in the cervical spine; and type III, by partial or complete occipitoatlantal fusion and symmetrical or asymmetrical hemiatlas aplasia with or without anomalies of the odontoid or other cervical vertebrae.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree