Corpus Callosotomy and Multiple Subpial Transections
Michael C. Smith
Richard Byrne
Andres M. Kanner
CORPUS CALLOSOTOMY
Corpus callosotomy was first introduced as a surgical treatment for medically intractable epilepsy by Van Wagenen and Herren in 1939 (1). The ultimate goal of callosal section is to abolish the bilateral synchrony (or near synchrony) of cortical epileptiform activity, which can result in seizures with bilateral motor manifestations, such as atonic, tonic, myoclonic, and tonic-clonic seizures. However, synchronous corticofugal epileptic discharges can also disrupt brainstem mechanisms that affect posture and tone of proximal limb and axial muscles, leading to atonic or akinetic seizures (2). The following section briefly reviews some of the more relevant studies that have played an important role in the development and refinement of the techniques used in corpus callosotomy.
Neurophysiologic Basis
The corpus callosum is the most important interhemispheric commissural connection in the brain, with approximately 180 million axons in humans (3). These axons connect homotopic as well as heterotopic cortical regions (4), and exert inhibitory as well as excitatory effects (5). This latter property of the corpus callosum has been suggested as an explanation for the clinical reports of increased partial seizures following callosotomy in humans (6,7) and in animals (8). Studies in rhesus monkeys show that section of the two-thirds anterior corpus callosum results in the development of partial seizures five times faster than in nonbisected animals (9). In the amygdala kindling model of the cat, Wada and Sato (10) reported that section of the corpus callosum accelerated the final stages of generalized convulsions.
The corpus callosum provides interhemispheric connection, unifying certain motor functions and sensory perceptions of the axial or midline visual and somatosensory world. Axons connecting the frontal lobes occupy a rostral position, whereas those connecting parietal, temporal, and occipital cortices are positioned more caudally, in that order.
The role of the corpus callosum in epileptogenesis is evident from various studies in animals. In the feline model of generalized epilepsy, Musgrave and Gloor (11) demonstrated the loss of bilateral synchrony of spike and slow-wave discharges following total section of the corpus callosum, and anterior commissure. Callosal section in the photosensitive baboon Papio papio resulted in a decrement in the synchronization of epileptiform discharges and of seizures triggered by photic stimulation (12,13). In a 1950 study of four monkeys by Kopeloff and colleagues (8), seizures generated by unilateral application of aluminum oxide cream had a bilateral motor expression. Following callosal section, the clinical manifestations were restricted to a distribution contralateral to the seizure focus.
It must be remembered that although the corpus callosum may be the most important anatomic structure for the interhemispheric spread of epileptic activity, it is not the only one. Anterior and posterior commissures and thalamus and brainstem structures may all play a role in the spread of discharge from one hemisphere to the other. Suppression of synchronized epileptic activity is routinely and repeatedly seen in acute models of generalized seizures. However, in most models of chronic epilepsy, synchronized
epileptic activity returns over months following callosotomy. This suggests that the epileptic activity uses alternate pathways over time. In patients who demonstrate lateralized epileptic activity postoperatively, there is a general tendency for these discharges to synchronize again over the first postoperative year.
epileptic activity returns over months following callosotomy. This suggests that the epileptic activity uses alternate pathways over time. In patients who demonstrate lateralized epileptic activity postoperatively, there is a general tendency for these discharges to synchronize again over the first postoperative year.
Studies in Humans
The first series of 10 patients was published in 1940 by Van Wagenen and Herren (1). However, the real interest in this procedure developed almost 30 years later, when Wilson reported on the Dartmouth series of callosotomies (14). In general, the clinical series have repeated the animal studies, demonstrating the efficacy of callosotomy in treating seizures requiring bilateral synchrony for their clinical expression. In 1985, Spencer and associates (15) reported the abolition of a bilaterally synchronous ictal onset in all 5 patients who underwent a complete section of the corpus callosum, but in only 5 of 10 patients who underwent a two-thirds anterior section. In contrast, interictal bisynchronous discharges persisted even after a complete section, albeit with a significantly lower frequency. A significant reduction in bisynchronous discharges has been reported in several other patient series (14,16, 17, 18, 19). However, as with animal studies, there are a number of reports of an increase in partial seizures (2,20, 21, 22, 23, 24) and Spencer and coworkers described them as being more intense as well (25). Other researchers report a conversion of generalized to partial seizures following callosotomy.
Indications
In 1985, Williamson suggested the use of corpus callosotomy to treat infantile hemiplegia, Rasmussen syndrome, Lennox-Gastaut syndrome, and frontal lobe epilepsy. Hemispherectomy is the treatment of choice for such hemispheric syndromes as Rasmussen syndrome and perinatal infarction with hemiplegia, whereas cortical resection is performed in patients with frontal lobe epilepsy. The primary use of corpus callosotomy has been for the treatment of patients with Lennox-Gastaut syndrome. As new medications, the ketogenic diet, and vagus nerve stimulation have become available for these patients, corpus callosotomy has been reserved as a later therapy for patients with severe refractory epilepsy with frequent injurious drop attacks.
Efficacy
In general, the purpose of corpus callosotomy is to palliate a patient’s intractable seizure condition by decreasing or abolishing the most incapacitating of the generalized seizures and thus improving the patient’s quality of life (QOL). Overall, 50% to 77% of patients with Lennox-Gastaut syndrome have been reported to have a satisfactory outcome, defined as a seizure reduction of 50% to 80% or more in the different series. The best response has been observed in patients with drop attacks presenting as tonic and atonic seizures. However, there is evidence that patients with atonic seizures derived a greater benefit from the procedure than did those with tonic seizures (18,19,22,26, 27, 28). In 1996, Phillips and Sakas (29) reported the results of anterior callosotomy in 20 patients. They divided outcome into freedom from seizures and significant reduction (70%) of seizures. Using these criteria, 16 of 20 patients (80%) experienced significant improvement of a 70% or greater decrease in seizure frequency. Eleven of 13 patients with atonic seizures had the best outcome, and favorable results were found in 14 of 18 patients with generalized tonic-clonic seizures. Gates and colleagues (30) reported that tonic seizures in the presence of an ictal electroencephalographic pattern consisting of an electrodecremental response were associated with a very good outcome in 92% of patients 10 years of age or older. However, this association of seizure type and ictal electroencephalographic pattern was not predictive of outcome in younger patients (16,30).
Corpus callosotomy yields a significant reduction in generalized tonic-clonic seizures in 50% to 80% of several patient series (6). Oguni and coworkers (28) and Spencer and associates (7) suggest that patients with secondarily generalized tonic-clonic seizures in the presence of electroencephalographic evidence of secondary bilateral synchrony and clinical or neuroradiologic evidence of focality derive greater benefit than those with generalized tonic-clonic seizures without these characteristics. This view is not universally accepted; Phillips and Sakas do not consider neuroimaging or electroencephalographic findings to be predictive of outcome (29).
Patients with complex partial seizures are less likely to respond to this procedure; approximately 40% derive a significant reduction in seizures. Simple partial seizures are rarely affected by callosotomy. Corpus callosotomy had been used in patients with frontal lobe seizures in whom the seizure focus could not be lateralized because of very rapid spread of epileptiform activity. However, Purves and colleagues (31) reported on six such patients who underwent a two-thirds anterior callosotomy without favorable results.
Corpus callosotomy may be performed as a partial resection involving the anterior two thirds of the corpus callosum (the majority of cases) or as a complete section. The decision to use one technique over the other remains controversial. Studies by Cendes and coworkers (32), Harbaugh and associates (27), and Reutens and colleagues (33) showed no difference in seizure control between complete and partial sections. Spencer and associates (7), on the other hand, reported the elimination of generalized tonic-clonic seizures in 77% of patients who underwent a complete section of the corpus callosum, compared with 35% of patients who underwent a two-thirds anterior
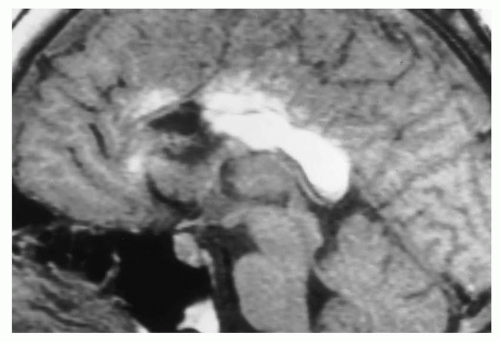
callosotomy. Following a reanalysis of 50 callosotomy patients, Spencer and coworkers (24) concluded that a two-thirds anterior section should be considered for patients with tonic, atonic, or myoclonic seizures, whereas a complete section should be reserved for those with an incomplete response to the two-thirds anterior section. Maehara and Shimizu (34) advocate a complete callosotomy, especially in children and adults with widespread epilepsy. In any event, when a complete section is considered, it should be carried out as a two-stage procedure in order to minimize neuropsychological complications (Fig. 84.1).
callosotomy. Following a reanalysis of 50 callosotomy patients, Spencer and coworkers (24) concluded that a two-thirds anterior section should be considered for patients with tonic, atonic, or myoclonic seizures, whereas a complete section should be reserved for those with an incomplete response to the two-thirds anterior section. Maehara and Shimizu (34) advocate a complete callosotomy, especially in children and adults with widespread epilepsy. In any event, when a complete section is considered, it should be carried out as a two-stage procedure in order to minimize neuropsychological complications (Fig. 84.1).
Impact of Seizure Reduction on Quality of Life
In 1997, Rougier and associates reviewed the literature on the efficacy of corpus callosotomy and its effect on QOL (35). They found a favorable outcome, defined as a 50% seizure reduction in 60% to 80% of all patients with atonic seizures and tonic seizures resulting in falls. Favorable outcomes in patients with tonic-clonic seizures varied from 40% to 80%. Patients with complex or simple partial seizures experienced significant improvement less often. Improvements in QOL indices and social adjustment did not always coincide with reduction in seizure frequency. The length of time that a patient had had intractable epilepsy and its deleterious effect on the patient’s cognitive and social function were important variables in predicting QOL improvements. In a study conducted at the Cleveland Clinic in Cleveland, Ohio, 9 of 17 patients experienced a greater than 80% reduction in their targeted seizures, and 15 of 17 reported satisfaction with the surgical outcome. However, improvement in alertness and responsiveness, not necessarily reduction in seizure frequency, was most closely associated with satisfaction with surgical outcome. Papo and colleagues (36) reviewed the records of 36 patients with intractable seizures of mixed types. Twenty-seven had had an anterior callosotomy, 8 had had a complete callosotomy in two stages, and 1 had had a posterior callosotomy. Of the 36 patients, 30 had adequate follow-up to report meaningful results. Fourteen had excellent results (defined as a greater than 90% reduction in targeted seizure type), five had good results (greater than 50% reduction), six had poor results (less than 50% reduction), and five showed no change. Global QOL measures did not always coincide with improvement in seizure frequency. In some patients with excellent seizure results, no clear change in QOL was reported. The authors suggest that this might be related to the long duration of uncontrolled seizures and their effect on cognitive function. Gilliam and coworkers (37) have also noted that overall clinical improvement did not always correlate with seizure reduction.
Surgical Technique
Under general anesthesia, the patient is placed in the supine position with pressure points padded. The head is placed in pin fixation in neutral position, with the neck slightly flexed. The hair is clipped and the skin prepped. A lumbar drain may be placed to aid in retraction of the midline. A variety of skin incisions may be used for anterior callosal sectioning, all of which provide access to the anterior midline. A coronally oriented skin incision 2 cm anterior to the coronal suture, exposing both sides of the midline, will afford the needed exposure. This incision will usually expose more of the right side than the left, because approach from the right allows retraction of the nondominant hemisphere. Hodaie and associates propose the use of image guidance, in part to analyze the parasagittal veins and thus determine the side of entry (38). A craniotomy is performed just anterior to the coronal suture, crossing midline to expose the sagittal sinus. The procedure can be performed without exposing the sinus, but retraction of the sinus is then not possible and sinus bleeding is more difficult to control if encountered. The dural flap is based on the sinus, and retraction of the dura allows retraction of the sinus. Although the exposure is anterior to the coronal suture, all but the most insignificant bridging veins should be spared. Planning the approach and exposure may thus be aided by examining preoperative magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) scans (Fig. 84.1). If a bridging vein complex does not allow retraction because of a far lateral entry of the vein into the sagittal sinus, a dural incision may be made in the form of a triangle around the laterally entering vein to allow retraction of the dural flap without disturbing the vein.
Once an unencumbered view of the intrahemispheric fissure is obtained, the medial aspect of the exposed frontal lobe is covered with moist cottonoids and selfretaining retractors are gently advanced. The falx is followed down the midline until the cingulated gyri are encountered. An error that is sometimes made is to mistake this view of the adherent cingulate gyri for the corpus
callosum. The cingulated gyri are separated under magnification in the midline, exposing the corpus callosum and the pericallosal arteries. Once this view is obtained and the retractors are set, a final check of the anterior exposure confirms the exposure of the anterior corpus callosum if the genu is visible.
callosum. The cingulated gyri are separated under magnification in the midline, exposing the corpus callosum and the pericallosal arteries. Once this view is obtained and the retractors are set, a final check of the anterior exposure confirms the exposure of the anterior corpus callosum if the genu is visible.
The actual division of the anterior corpus callosum is performed with a microdissection instrument and gentle suction. This should begin in the midline of the callosum just posterior to the genu. Great care is taken to separate, but not disturb, the pericallosal arteries. At this level, certain landmarks, such as the cavum septum pellucidum, are visible beneath the corpus callosum, even if the landmark is only a potential space in the individual patient. This midline landmark is valuable, if found, because it confirms the complete transection of the callosal fibers and allows one to stay out of the lateral ventricles. If the lateral ventricle is entered, intraoperative or postoperative bleeding may result in hydrocephalus. The transection is then carried forward into the genu and the rostrum of the corpus callosum. The disconnection is carried out downward following the A2 branches as they approach the anterior communicating artery complex.
The extent of posterior callosal sectioning is determined preoperatively. Some surgeons advise a simple one-half callosal sectioning, which can be measured by comparing the intraoperative transection to the length of the callosum on the preoperative sagittal MRI. This and other techniques, such as intraoperative plain films and stereotaxy, have been used to confirm the length of the callosotomy (39). Other authors advocate a three-quarter sectioning, as there is some indication that seizure control may be more complete. If a complete corpus callosotomy is to be performed, the sectioning may be done with a microdissector or suction aspiration to the splenium. A complete posterior sectioning is confirmed by viewing the arachnoidcovered vein of Galen in the posterior midline. If only an anterior transection is planned, an MRI-compatible marker should be placed at the posterior border of the anterior transection in order to view on imaging studies and to note on reoperation, if necessary, the extent of the first procedure. Hemostasis is obtained, and any entry into a lateral ventricle is covered with Gelfoam. A standard craniotomy closure is performed.
Complications
Complications unique to corpus callosotomy as a surgical procedure are neuropsychological in nature. Well-described acute and chronic neuropsychological sequelae are possible following callosotomy (40,41). Varying degrees of the acute disconnection syndrome, characterized by a lethargic, apathetic mutism during the first few days after surgery, are commonly seen. In our experience and that of other investigators, this syndrome is always transient in nature. The predictors of this transient state are related to the extent of callosal sectioning, baseline cognitive impairment, and the amount of traction necessary to gain access to the corpus callosum. Other observed early manifestations of the acute disconnection syndrome include incontinence, bilateral Babinski sign, and apraxia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree