Chapter 11 Cranial Nerves
Cranial nerves are the means by which the brain receives information from, and controls the activities of, the head and neck and, to a lesser extent, the thoracic and abdominal viscera. Briefly, there are 12 pairs of cranial nerves that are individually named and numbered (using roman numerals) in a rostrocaudal sequence (see Table 1.1). Unlike spinal nerves, only some are mixed in function and thus carry both sensory and motor fibres. Others are purely sensory or purely motor. The first cranial nerve (I; olfactory) has an ancient lineage and is derived from the forerunner of the cerebral hemisphere. It retains this unique position through the connections of the olfactory bulb and is the only sensory cranial nerve that projects directly to the cerebral cortex rather than via the thalamus, as do all other sensory modalities. The areas of cerebral cortex involved have a primitive cellular organization and are an integral part of the limbic system, which is concerned with the emotional aspects of behaviour. The second cranial nerve (II; optic) consists of the axons of second-order visual neurones and terminates in the thalamus. The other 10 pairs of cranial nerves attach to the brain stem. Most of the component fibres originate from, or terminate in, named cranial nerve nuclei (Ch. 10).
Olfactory Nerve (I)
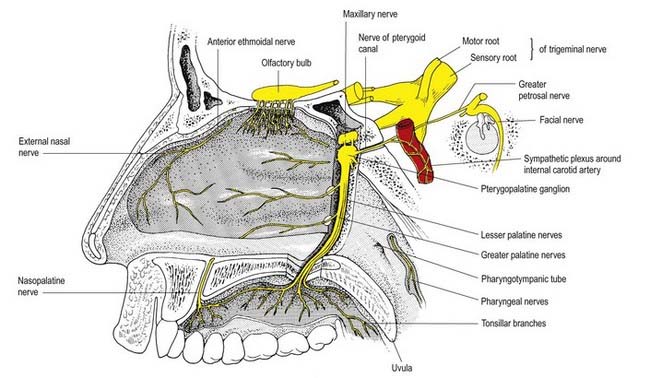
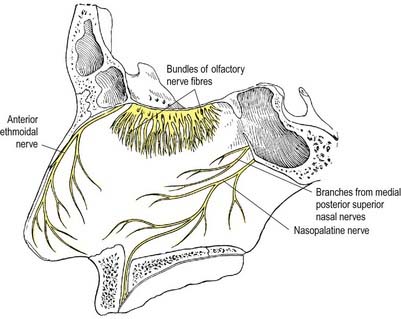
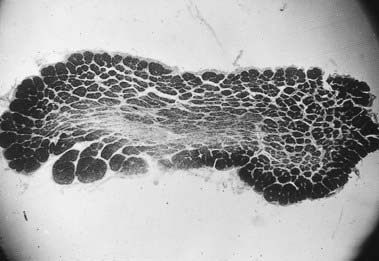
The cell of origin of the olfactory nerves serving the sense of smell is in the olfactory mucosa covering the superior nasal concha, the upper part of the vertical portion of the middle concha and the opposite part of the nasal septum. The axons, which are unmyelinated, originate as the central or deep processes of the olfactory neurones and collect in bundles that cross in various directions, forming a plexiform network in the mucosa. The bundles finally form approximately 20 branches that traverse the cribriform plate in lateral and medial groups and end in the glomeruli of the olfactory bulb. Each branch has a sheath consisting of dura mater and pia-arachnoid; the former continues into the nasal periosteum, and the latter into the connective tissue sheaths surrounding the nerve bundles (Figs 11.1, 11.2).
Olfactory pathways subserving the sense of smell are described in Chapter 12.
CASE 1 Anosmia
Discussion: This man has suffered a basal skull fracture involving the floor of the anterior fossa. The fracture line crosses the olfactory groove, resulting in laceration of the olfactory nerve and thus anosmia. Tumours and other mass lesions on the floor of the anterior fossa may similarly result in ipsilateral loss of the sense of smell; bilateral anosmia, with or without impairment of taste, may be due to the use of a variety of drugs, such as calcium channel blockers, some antibiotics, anticonvulsants and opiates, among others. (See also Ch. 9, Case 1.)
Optic Nerve (II)
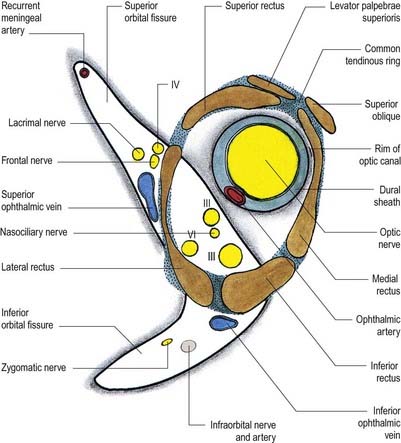
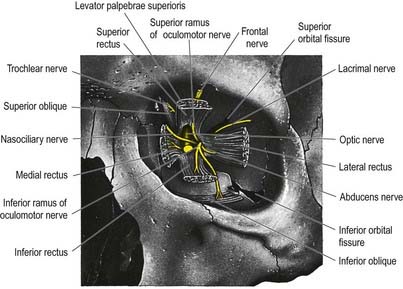
The optic nerve is the second cranial nerve (Figs 11.3, 11.4). It arises from the optic chiasma on the floor of the diencephalon and enters the orbit through the optic canal, accompanied by the ophthalmic artery. It changes shape, starting out flat at the chiasma and becoming rounded as it passes through the optic canal. In the orbit it passes forward, laterally and downward and pierces the sclera at the lamina cribrosa, slightly medial to the posterior pole. It has a somewhat tortuous course within the orbit to allow for movements of the eyeball. It is surrounded by extensions of the three layers of meninges.
Oculomotor Nerve (III)
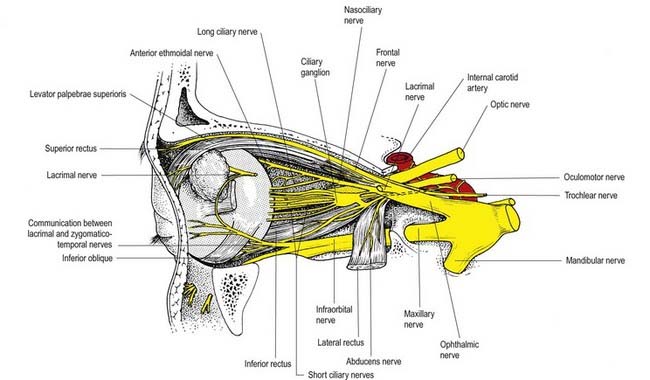
The oculomotor nerve is the third cranial nerve (Figs 11.3, 11.4, 11.8). It is the main source of innervation to the extraocular muscles and also contains parasympathetic fibres that relay in the ciliary ganglion.
CASE 3 Thyroid-Associated Ophthalmopathy (Graves’ Disease)
A 45-year-old woman is referred for evaluation of a mild action tremor. She has a history of a mixed seizure disorder in the first two decades of her life, completely controlled by sodium divalproate. She subsequently complains of double vision, and neuro-ophthalmological a examination shows impaired up-gaze of the right eye with resultant vertical diplopia. There is slight lid retraction. Thyroid function testing reveals an elevated thyroxine (T4) level and reduced thyroid-stimulating hormone (TSH). Orbital magnetic resonance imaging (MRI) documents thickening of the extraocular muscles, particularly involving the medial and inferior recti of the right eye (Fig. 11.9).
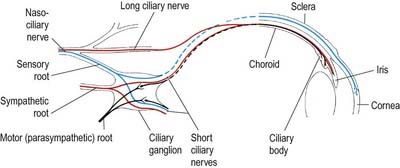
Ciliary Ganglion
The ciliary ganglion is a parasympathetic ganglion concerned functionally with the motor innervation of certain intraocular muscles (Figs 11.5, 11.6). It is a small, flat, reddish grey swelling, 1 to 2 mm in diameter, connected to the nasociliary nerve and located near the apex of the orbit in loose fat approximately 1 cm in front of the medial end of the superior orbital fissure. It lies between the optic nerve and lateral rectus, usually lateral to the ophthalmic artery. Its neurones, which are multipolar, are larger than in typical autonomic ganglia; a very small number of more typical neurones are also present.
The sympathetic root contains fibres from the plexus around the internal carotid artery within the cavernous sinus. These postganglionic fibres, derived from the superior cervical ganglion, form a fine branch that enters the orbit through the superior orbital fissure inside the common tendinous ring of recti muscles. The fibres either pass directly to the ganglion or join the nasociliary nerve and travel to the ganglion in its sensory root. Either way, they traverse the ganglion without synapsing to emerge into the short ciliary nerves. They are distributed to the blood vessels of the eyeball. Sympathetic fibres innervating dilator pupillae may sometimes travel via the short ciliary nerves (rather than the more usual route via the ophthalmic, nasociliary and long ciliary nerves).
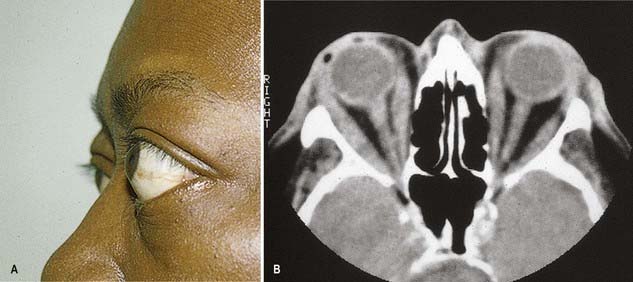
CASE 2 Nutritional Amblyopia
Discussion: This man has nutritional amblyopia, sometimes referred to as tobacco-alcohol amblyopia. The clinical manifestations are due to bilateral involvement of the neural fibres constituting the macular projection system, resulting in a macular syndrome. The lesions predominate in the central portion of the optic nerves bilaterally, where the macular fibres are found, thus making it a disorder of the anterior conducting system (Fig. 11.7). Although tobacco use is sometimes implicated as a cause, this is in all likelihood a nutritional disorder due to deficiency of one or more B vitamins. It responds quickly to vitamin supplementation.
Trochlear Nerve (IV)
The trochlear nerve is the fourth cranial nerve and is the only one that emerges from the dorsal surface of the brainstem (see Fig. 11.35). It passes from the midbrain onto the lateral surface of the crus of the cerebral peduncle and runs through the lateral dural wall of the cavernous sinus. It then crosses the oculomotor nerve and enters the orbit through the superior orbital fissure, above the common tendinous ring of the recti muscles and levator palpebrae superioris and medial to the frontal and lacrimal nerves. The trochlear nerve travels only a short distance to enter the superior (orbital) surface of superior oblique, which is its sole target (see Fig. 11.8).
CASE 4 Diabetic Third Nerve Palsy
Two months later the patient is entirely normal except for persistent mild left ptosis.
Discussion: Vasculopathic third nerve palsies are most commonly associated with diabetes mellitus and usually come under the rubric of diabetic ophthalmoplegia. Other conditions associated with microvascular disease, such as hypertension and dyslipidemia, may also be responsible. Most cases are thought to be the result of ischaemia affecting the central portion of the oculomotor nerve, sparing the peripherally located pupillary fibre bundle; nonetheless, a small proportion of patients exhibits minor pupillary involvement. In contrast, compressive third nerve palsies, such as those associated with an intracranial aneurysm, almost always have marked pupillary involvement and usually present with more pain. See Figure 11.10.
Trigeminal Nerve (V)
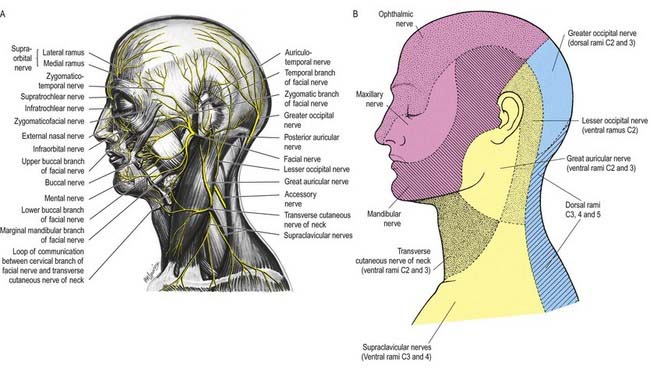
Innervation of the Face and Scalp
Three large areas of the face can be mapped to indicate the peripheral nerve fields associated with the three divisions of the trigeminal nerve. The fields are not horizontal but curve upward (Fig. 11.11A), apparently because the facial skin moves upward with growth of the brain and skull. Embryologically, each division of the trigeminal nerve is associated with a developing facial process that gives rise to a specific area of the face in the adult. Thus the ophthalmic nerve is associated with the frontonasal process, the maxillary nerve with the maxillary process and the mandibular nerve with the mandibular process.
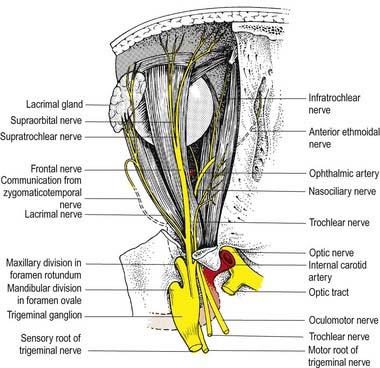
Ophthalmic Nerve
The ophthalmic nerve (Fig. 11.11B), a division of the trigeminal nerve, travels through the orbit to supply targets primarily in the upper part of the face. It arises from the trigeminal ganglion in the middle cranial fossa and passes forward along the lateral dural wall of the cavernous sinus. It gives off three main branches—the lacrimal, frontal and nasociliary nerves—just before it reaches the superior orbital fissure. The cutaneous branches of the ophthalmic nerve supply the conjunctiva, skin over the forehead, upper eyelids and much of the external surface of the nose.
CASE 5 Herpes Zoster Ophthalmicus
She is diagnosed with herpes zoster ophthalmicus. Within several days, vesicles appear in the territory of the ophthalmic division of the right trigeminal nerve, along with keratitis, conjunctivitis and iritis of the right eye (Fig. 11.12).
Lacrimal Nerve
The lacrimal nerve enters the orbit through the superior orbital fissure, above the common tendinous ring of the recti muscles and lateral to the frontal and trochlear nerves (see Figs 11.4, 11.5, 11.8). It passes forward along the lateral wall of the orbit on the superior border of the lateral rectus and travels through the lacrimal gland and the orbital septum to supply conjunctiva and skin covering the lateral part of the upper eyelid. The lacrimal nerve communicates with the zygomatic branch of the maxillary nerve, so parasympathetic fibres associated with the pterygopalatine ganglion might be conveyed to the lacrimal gland.
Frontal Nerve
The frontal nerve is the largest branch of the ophthalmic nerve (see Figs 11.4, 11.5, 11.8). It enters the orbit through the superior orbital fissure, above the common tendinous ring of the recti muscles, and lies between the lacrimal nerve laterally and the trochlear nerve medially. It passes forward on the levator palpebrae superioris, toward the rim of the orbit; about halfway along this course it divides into the supraorbital and supratrochlear nerves.
Nasociliary Nerve
The nasociliary nerve is intermediate in size between the frontal and lacrimal nerves and is more deeply placed in the orbit, which it enters through the common tendinous ring, lying between the two rami of the oculomotor nerve (see Figs 11.4, 11.5, 11.8). It crosses the optic nerve with the ophthalmic artery and runs obliquely below superior rectus and superior oblique to reach the medial orbital wall. Here, as the anterior ethmoidal nerve, it passes through the anterior ethmoidal foramen and canal and enters the cranial cavity. It runs forward in a groove on the upper surface of the cribriform plate beneath the dura mater and descends through a slit lateral to the crista galli into the nasal cavity, where it occupies a groove on the internal surface of the nasal bone and gives off two internal nasal branches. The medial internal nasal nerve supplies the anterior septal mucosa, and the lateral internal nasal nerve supplies the anterior part of the lateral nasal wall. The anterior ethmoidal nerve emerges, as the external nasal nerve, at the lower border of the nasal bone and descends under the transverse part of the nasalis to supply the skin of the nasal alae, apex and vestibule.
Two or three long ciliary nerves branch from the nasociliary nerve as it crosses the optic nerve (see Fig. 11.5). They accompany the short ciliary nerves and pierce the sclera near the attachment of the optic nerve. Running forward between the sclera and choroid, they supply the ciliary body, iris and cornea and are thought to contain postganglionic sympathetic fibres for the dilator pupillae from neurones in the superior cervical ganglion. An alternative pathway for the supply of the dilator pupillae is via the sympathetic root associated with the ciliary ganglion.
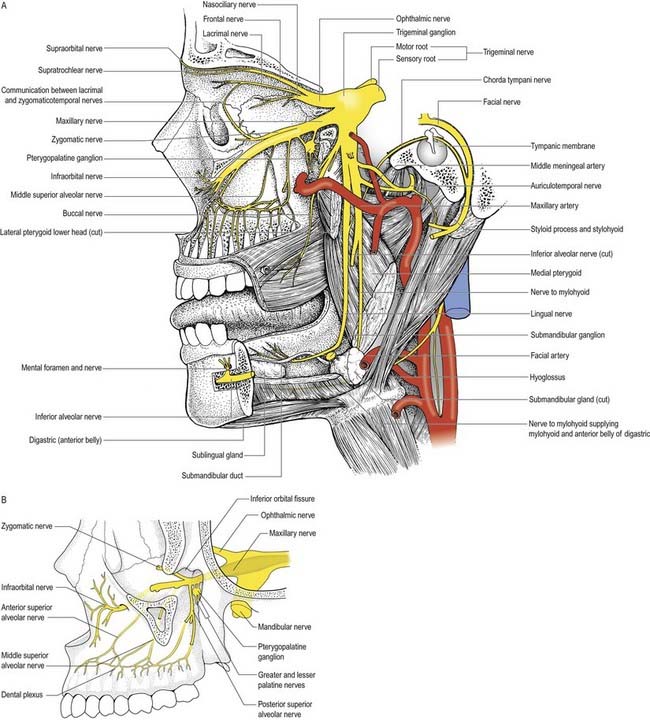
Maxillary Nerve
Zygomatic Nerve
The zygomatic nerve is located close to the base of the lateral wall of the orbit. It soon divides into two branches—the zygomaticotemporal and zygomaticofacial nerves—which run for only a short distance in the orbit before passing onto the face through the lateral wall of the orbit. Either these two branches enter separate canals within the zygomatic bone or the zygomatic nerve itself enters the bone before dividing.
The zygomaticotemporal nerve exits the zygomatic bone on its medial surface and pierces the temporal fascia to supply the skin over the temple. It also gives a branch to the lacrimal nerve, which may carry parasympathetic fibres to the lacrimal gland (Figs 11.5, 11.13).
Infraorbital Nerve
The infraorbital nerve emerges onto the face at the infraorbital foramen (see Fig. 11.5), where it lies between the levator labii superioris and levator anguli oris. It divides into three additional groups of branches. The palpebral branches ascend deep to orbicularis oculi and pierce the muscle to supply the skin of the lower eyelid and join with the facial and zygomaticofacial nerves near the lateral canthus. Nasal branches supply the skin of the side of the nose and movable part of the nasal septum and join the external nasal branch of the anterior ethmoidal nerve. Superior labial branches, large and numerous, descend behind levator labii superioris to supply the skin of the anterior part of the cheek and upper lip. They are joined by branches from the facial nerve to form the infraorbital plexus.
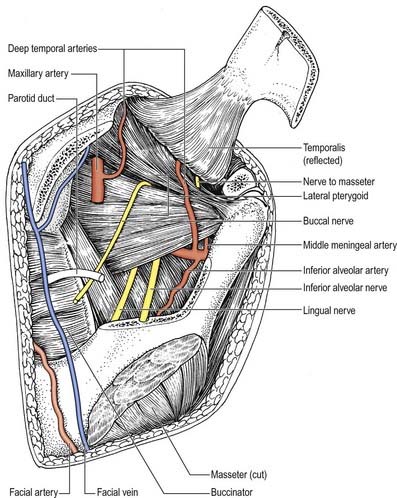
Mandibular Nerve
The mandibular nerve is the largest trigeminal division and is a mixed nerve (Figs 11.11, 11.13, 11.14). Its sensory branches supply the teeth and gums of the mandible; the skin in the temporal region; part of the auricle, including the external meatus and tympanic membrane, and the lower lip; the lower part of the face (see Fig. 11.11); and the mucosa of the anterior two-thirds (presulcal part) of the tongue and floor of the oral cavity. The motor branches innervate the muscles of mastication. The large sensory root emerges from the lateral part of the trigeminal ganglion and exits the cranial cavity through the foramen ovale. The small motor root passes under the ganglion and through the foramen ovale to unite with the sensory root just outside the skull. As it descends from the foramen ovale, the nerve is approximately 4 cm from the surface and a little anterior to the neck of the mandible. The mandibular nerve immediately passes between tensor veli palatini, which is medial, and lateral pterygoid, which is lateral, and gives off a meningeal branch and nerve to the medial pterygoid from its medial side. The nerve then divides into small anterior and large posterior trunks. The anterior division gives off branches to the four main muscles of mastication and a buccal branch that is sensory to the cheek. The posterior division gives off three main sensory branches—the auriculotemporal, lingual and inferior alveolar nerves—and motor fibres to supply the mylohyoid and anterior belly of the digastric (see Figs 11.13, 11.14).
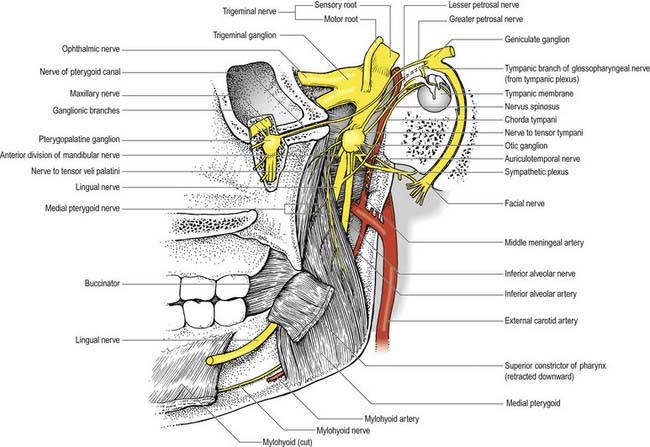
Fig. 11.14 Right otic and pterygopalatine ganglia and their branches displayed from the medial side.
Anterior Trunk
Buccal nerve
The buccal nerve (Fig. 11.15) passes between the two heads of the lateral pterygoid. It descends deep to the temporalis tendon, passes laterally in front of the masseter, and anastomoses with the buccal branches of the facial nerve. It carries the motor fibres to the lateral pterygoid, and these are given off as the buccal nerve passes through the muscle. It may also give off the anterior deep temporal nerve. The buccal nerve supplies sensation to the skin over the anterior part of the buccinator and buccal mucous membrane, together with the posterior part of the buccal gingivae adjacent to the second and third molar teeth.
Nerve to masseter
The nerve to the masseter (see Fig. 11.15) passes laterally above the lateral pterygoid and on to the skull base, anterior to the temporomandibular joint and posterior to the temporalis tendon. It crosses the posterior part of the mandibular notch with the masseteric artery and ramifies on and enters the deep surface of the masseter. It also provides articular branches that supply the temporomandibular joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree