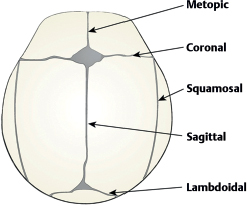
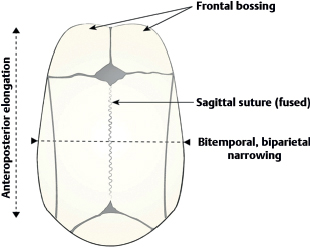
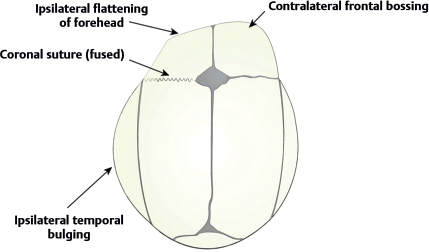
71 When does the embryonic skull begin to form? Between the 23rd and 26th day of gestation What is thought to initiate cranial suture formation? Osteogenic fronts, which consist of osteoprogenitor cells and osteoblasts at the leading edges of developing bone What factors determine normal suture formation? Bone deposition by osteoblasts, bone remodeling by osteoclasts, apoptosis in the frontal boundaries, local interactions between the dura mater and the sutures, genetic regulation, growth factors (fibro-blast growth factor receptor [FGFR]-1, -2, -3, -4; transforming growth factor [TGF]-1, -2, -3), and transcription factors True or false: The primary influence for cranial growth is the growing brain. True What are the sutures of the cranium? • Metopic (between both frontal bones) • Sagittal (between both parietal bones) • Two coronal (between parietal and frontal bones on each side) • Two lambdoid (between occipital and parietal bones on each side) • Squamosal (between parietal, temporal, and sphenoid bones) Fig. 71.1 Normal cranial sutures. Which of the sutures naturally closes earliest? The metopic suture—usually closed by 9 months of age and is unidentifiable in adults What does craniosynostosis refer to? Premature closure of cranial sutures resulting in skull deformities and problems in neurological development What is the incidence of craniosynostosis? 1 in 2100 children What categories of craniosynostosis are there? Nonsyndromic (primary): • Most common • Isolated sutures are affected Syndromic: • Multiple sutures are affected Part of a systemic disorder True or false: Craniosynostosis has a wide array of causes. True. Causes include: • Genetic mutations • Metabolic disorders • Rickets • Hyperthyroidism • Mucopolysaccharidoses • Hurler syndrome • Morquio syndrome • β-glucuronidase deficiency • Mucolipidoses • Hematological disorders • Thalassemias • Sickle cell anemia • Polycythemia vera • Teratogens • Valproic acid • Aminopterin • Diphenylhydantoin • Retinoic acid • Malformations • Microcephaly • Encephalocele • Shunted hydrocephalus • Holoprosencephaly True or false: The majority of simple, nonsyndromic craniosynostoses have a genetic pattern of inheritance. False; the majority are sporadic. Are there exceptions to the above? Yes; 2 to 6% of sagittal synostosis cases and 8 to 14% of coronal synostosis cases have been shown to have an autosomal dominant inheritance pattern. Can fetal head restraints cause craniosynostosis? Yes, although fetal head restraints usually result in cranial deformational asymmetries that are not true craniosynostoses. What are the four principles associated with suture closing? 1. Calvarial bones directly next to the fused suture act as a single bone plate with decreased growth potential. 2. Asymmetrical bone deposition occurs at the sutures along the perimeter of the bone plate with increased bone deposition at the outer margin. 3. Nonperimeter sutures in line with the fused suture deposit bone symmetrically at their suture edges. 4. Perimeter sutures adjacent to the fused suture compensate to a greater degree than the other distant sutures. How is craniosynostosis diagnosed? Prenatal ultrasound monitoring and clinical observation to see if the skull has a shape following the above four principles, along with absence of movement across the fused suture with or without palpable ridging over the fused suture What clinically similar condition must be differentiated from true craniosynostosis? Deformational plagiocephaly (DP), which is more common than craniosynostosis and results from external forces (e.g., sleeping position) causing skull deformation into a parallelogram shape when seen from above; resembles unilateral coronal and lambdoid craniosynostosis What imaging studies should be done if a prematurely closed suture is suspected? Plain x-ray or CT of the skull, with absence of the suture or bony ridging across part of the suture confirming the diagnosis What are the different types of nonsyndromic craniosynostosis? Simple • Scaphocephaly (dolichocephaly) → sagittal suture • Frontal plagiocephaly → unilateral coronal suture • Trigonocephaly → metopic suture • Posterior plagiocephaly → unilateral lambdoid suture Compound • Variable → two sutures • Brachycephaly → bilateral lambdoid sutures • Turribrachycephaly → bilateral coronal sutures True or false: Sagittal suture craniosynostosis is the most common form. True; it accounts for 40 to 60% of all craniosynostosis cases. How does the head look in sagittal synostosis? Scaphocephalic: anteroposterior elongation with frontal and/or occipital bossing and biparietal and bitemporal narrowing Fig. 71.2 Scaphocephaly. True or false: Bilateral coronal synostosis is twice as common as unilateral coronal involvement. False; unilateral coronal synostosis is twice as common as bilateral coronal involvement. How does the head look in unilateral coronal synostosis? Frontal plagiocephaly: flattened ipsilateral forehead and parietal area, compensatory contralateral frontal bossing and ipsilateral temporal bulging (from perpendicular growth of neighboring sutures) Craniofacial deformities: • Nasal root deviation to ipsilateral side • Anterior displacement of ipsilateral ear • Superiorly displaced sphenoid wing → heightened orbit (“harlequin” deformity) Fig. 71.3 Frontal plagiocephaly.
Craniosynostosis
71.1 Anatomy
71.2 Basic Concepts
71.3 Classification
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Craniosynostosis
Only gold members can continue reading. Log In or Register to continue




