CHAPTER 177 Dandy-Walker Syndrome
History
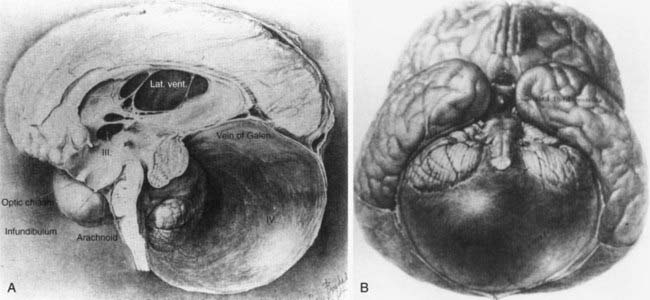
Dandy-Walker syndrome (DWS) represents a congenital malformation characterized by agenesis or hypoplasia of the cerebellar vermis, cystic dilation of the fourth ventricle, and enlargement of the posterior fossa with or without hydrocephalus. The first autopsy description of such a clinical picture appeared in 1887 by Sutton.1 It was not until 1914 that Dandy and Blackfan realized an association between hydrocephalus and cystic fourth ventricular dilation in a 13-month old girl.2 The malformation was further characterized by Dandy3 in 1921 and by Taggart and Walker4 in 1942 as being related to congenital atresia of the fourth ventricular exit foramina (Fig. 177-1). However, it was Benda in an autopsy series in 1954 who first used the term Dandy-Walker syndrome to describe this condition and offer a new theory on its etiology.5 He postulated that failure of normal regressive changes in the posterior medullary velum and absence of the cerebellar vermis formed a cyst from the distal end of the fourth ventricle that separated the cerebellar hemispheres. Since that time, no significant progress has been made in terms of etiology; however, DWS is a well-known malformation that has been associated with other central nervous system (CNS) and systemic anomalies, including genetic aberrations, environmental factors, teratogens, and congenital infections to name a few.6 Advances in diagnostic imaging and increased accessibility to them may have led to the overdiagnosis of DWS.7–9 This chapter aims to describe the basic clinicopathologic features of DWS; its diagnosis with other CNS, systemic, and genetic associations; and treatment controversies that still exist today.
Embryology, Pathophysiology, and Etiology
Cerebellar development begins in the ninth week of gestation when the genesis of the cerebellar hemispheres occurs from the rhombic lips. Subsequently, the hemispheres fuse to form the vermis. The choroid plexus of the fourth ventricle and the foramina of Magendie form around the 10th week of gestation from the rhombic vesicle. The fourth ventricle develops when cerebrospinal fluid (CSF) accumulates within its space. The cerebellar lobules develop from an anterior to posterior direction and are completely formed by week 18.10 The cerebellum develops slower than the cerebral hemispheres and therefore appears smaller at 20 weeks of gestation relative to the large posterior fossa CSF spaces, leading to a potential overdiagnosis of vermian hypoplasia by antenatal ultrasound.
Terminology and Differential Diagnosis
Dandy-Walker variant (DWV) is a term that was first introduced by Harwood-Nash and Fitz to describe a milder spectrum of DWS-like signs that were not congruent with the classic definition. It consists of an inferior cerebellar vermian defect and communication between normal-sized cisterna magna and the fourth ventricle.11 Dandy-Walker complex (DWC) is another term coined to describe a continuum of posterior fossa anomalies categorized from mild (mega-cisterna magna only) to moderate (mild hypoplasia of vermis, enlarged fourth ventricle) to severe (agenesis of vermis, dilation of posterior fossa cyst and fourth ventricle).12
This wide spectrum of posterior fossa cystic malformations provides the basis for a differential diagnosis in prenatal or postnatal presentations. These include DWV, mega-cisterna magna, posterior fossa arachnoid cyst, persistent Blake pouch cyst, fourth ventriculocele, and congenital vermian hypoplasia.12–14
Clinical Features
DWS has been reported to occur in 1 of 25,000 to 30,000 newborns15 with the highest incidence in infants younger than 1 year.16,17 However, diagnosis may be delayed until adolescence or even adulthood. Concurrent hydrocephalus may not be present on prenatal imaging or at birth but has been reported to occur in as few as 2% and as many as 90% of all patients.18–21 The higher end of this wide range is probably secondary to historical series of patients with hydrocephalus being the selected subgroup presenting to neurosurgical services. Those who develop hydrocephalus usually do so by 3 months of age.15 In one retrospective study of 72 children, 50% presented before 1 year of age, with a distribution up to 18 years of age, whereas the oldest reported newly diagnosed patient with DWS was 75 years old.22 The most common postnatal presentation is macrocrania. Other signs and symptoms may include sunset sign, large posterior fossa, seizures, spasticity, lethargy, delayed milestones, respiratory failure, apnea, increased intracranial pressure, and hydrocephalus. Older children may present similarly to patients with posterior fossa tumors, and symptoms may include nystagmus and ataxia.23 Numerous malformations are described in the literature in association with DWS and its variants. The incidence of associated anomalies in the CNS is variable but has been reported as high as 68%, with systemic abnormalities present in about one fourth of patients.24 The most commonly associated CNS abnormality is agenesis of corpus callosum, whereas systemically, capillary hemangiomas and cardiac defects represent the most frequent associations (Table 177-1).25
TABLE 177-1 Central Nervous System and Systemic Anomalies Associated with Dandy-Walker Syndrome
| CENTRAL NERVOUS SYSTEM |
| FACE |
| CARDIOVASCULAR |
| LUNG |
| ABDOMEN |
| MUSCULOSKELETAL |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|