Chapter 99 Deformity Surgery for Ankylosing Spondylitis
Ankylosing spondylitis (AS) is an inflammatory disease that can lead to painful disability and deformity.1 AS is characterized by a strong heretability factor, with most of the risk for susceptibility being connected to the presence of certain genes.2 The pathogenesis is thought to be immune-mediated joint erosion and bone proliferation that primarily affects the axial skeleton, including ligaments and articulations of the pelvis and spinal column. Inflammation of the vertebral joints and intervertebral disc spaces leads to ossification and fusion of the spine characterized by syndesmophyte formation, ankylosis, and the classic hallmark appearance of “bamboo spine.” Concomitant osteoporosis causes the spine to become brittle and susceptible to fracture and progressive spinal deformity. The etiopathogenesis of AS is under intense scrutiny at present, with current efforts under way to determine the exact roles of the mixture of genetic susceptibility, chronic inflammation, and bone-forming pathways.3
Clinical Presentation
AS is a chronic lifelong disease that affects men two to three times more frequently than women, and manifests clinically between the ages of 20 and 30.4 The prevalence of AS is between 0.5% and 1.3% and varies due to definition of the cases (pure AS vs. spondyloarthritis), screening criteria, ethnicity, and presence of the major histocompatability complex class I molecule HLA-B27.5 Although there is a strong correlation between the prevalence of HLA-B27 and AS, it is suspected but not proven that several non HLA-B27 genes are related to the disease progression.
The primary clinical axial spine symptom of AS from chronic inflammatory sacroiliitis is low back pain.6 The pain may be unilateral or bilateral and may include radicular symptoms extending into the buttocks or thigh that rarely extend below the knee. Symptoms are usually worse in the morning and improve with activity, distinguishing AS from mechanical low back pain. It is not uncommon for this back pain to awaken the patient at night, further distinguishing AS from other causes of chronic back pain. In children, of course, AS may present with peripheral arthritis.
Ankylosing spondylitic spinal deformity results from progressive flexion and kyphosis of the lumbar, thoracic, and cervical spine as patients attempt to unload stress from painful spondylitic facet joints.7 Autofusion in kyphosis results in a fixed flexion deformity and global sagittal imbalance with ventral displacement of the patient’s center of gravity. Compensatory flexion contractures of the hips and knees may develop as the patient attempts to maintain an erect posture and adequate field of vision. These strains lead to osseous remodeling, further kyphosis, and progressive deformity.
Inflammation and new bone formation drive vertebral column remodeling in AS.8 Indeed, the first two spinal lesions in AS described by Andersson9 and Romanus and Yden10 are inflammatory in nature. Andersson lesions appear as a spondylodiscitis that destroys the central portion of the intervertebral disc and adjacent vertebral body. Romanus lesions are erosive changes at the ventral and dorsal vertebral end plates that appear on radiographs as “shiny corners.” In late disease, these Romanus lesions lead to destruction and rebuilding of the cortex, resulting in squaring of the vertebral bodies.
Other inflammatory lesions are also characteristic of AS.6 Enthesopathy, or inflammation of the ligamentous insertion points, characterizes AS throughout the axial spine. Indeed, enthesitis is the cause of both Andersson and Romanus lesions. Synovitis occurs at zygapophyseal, costovertebral, and costotransverse joints. Inflammation then promotes ectopic bone formation within affected ligaments, resulting in ossification of spinal ligaments and within intervertebral discs, end plates, and apophyseal structures. Formation of new ectopic bone leads to formation of syndesmophytes (bridging the ossified nucleus pulposus at each disc level) or enthesophytes (osseous outgrowths that do not bridge structures). Therefore, advanced AS is characterized by universal syndesmophytosis and squared vertebral bodies with kyphotic deformity that is aptly termed “bamboo spine.” It is this propensity of AS patients to make new bone that may not be affected by newer biologic agents that provide remarkable symptom relief. This is the challenge to our understanding of the fundamental nature of this disease.3
Osteoporosis in AS is particularly challenging. Early papers hinted of osteoporosis as a late finding, but more recent studies have demonstrated that spinal osteoporosis is found even in early AS without peripheral osteoporosis.11 This axial osteoporosis is linked to early inflammatory remodeling of the spine. Syndesmophyte formation may also correlate with lower bone mineral density of the spine.12 Paradoxically, dual-energy x-ray absorptiometry (DEXA) scans in advanced AS may overestimate bone mineral density due to the increased mineral concentration in syndesmophytes, which provide no real functional support. CT can help correlate osteoporosis and disease duration. The clinical consequences of this osteoporosis are profound. Patients with early AS and mild osteoporosis have a fracture prevalence five times greater than in the normal population.13
The combination of inflammation and osteoporosis promotes AS fractures and is paradoxically related to ossification. Ossification of the disc space occurs centripetally through the anulus fibrosus, and only rarely is the center of the disc involved. This incomplete ossification leads to formation of polysegments in the spine, with resulting long lever arms of force. The combined stress concentration from loss of polysegmental spinal motion and secondary osteopenia predisposes patients to spinal fracture and nonunion. Aseptic spondylodiscitis, presenting as focal pain with coexisting erosive sclerotic changes in adjacent vertebral bodies, is noted at these sites.14 It is uncertain whether aseptic spondylodiscitis is a primary inflammatory process or the result of trauma. Radiographically, the appearances of spondylodiscitis, pseudarthrosis, and discitis are similar.
Acute traumatic fractures, particularly in the cervical spine, are also widely reported.6 Again, osteoporosis and stress forces due to long, stiff lever arms enhance the susceptibility of the AS patients to acute spinal fracture. The lifetime incidence of acute traumatic fractures is believed to be approximately 14%.15,16 It is reported that 75% of fractures occur in the cervical or cervicothoracic junction, 14% in the thoracic spine, and 5% in the lumbar spine.17,18 Cervical fractures commonly involve both anterior and posterior columns, leading to higher rates of mortality and neurologic complications in AS than in non-AS patients.19,20 Even minor trauma such as a simple slip and fall can cause a major spinal fracture and neurologic injury, with the rate of neurologic deficit ranging from 53% to 83%.21 There should be a high index of suspicion in any AS patient with acute onset of new focal pain or deformity, including any newly observed loss of height. Occult fractures must be suspected any time an abrupt change occurs in the patient’s condition, and CT is often required to fully evaluate the symptomatic areas. Undiagnosed or poorly managed spinal fractures can contribute to worsening kyphosis and deformity, particularly if the fractures heal in flexion.
Spinal deformity leads to disability and subsequent mortality.6 Chin-on-chest deformity seen with fixed cervical flexion significantly hinders forward vision, swallowing, hygiene, and self-esteem. The combination of debilitating disease, deformity, and limited treatment options makes managing these deformities difficult. Although the surgical management of AS deformity is technically challenging and not without risks, the psychological and functional impairment of progressive deformity warrants surgical correction and stabilization when conservative options have been exhausted.
Surgical Management
General Principles
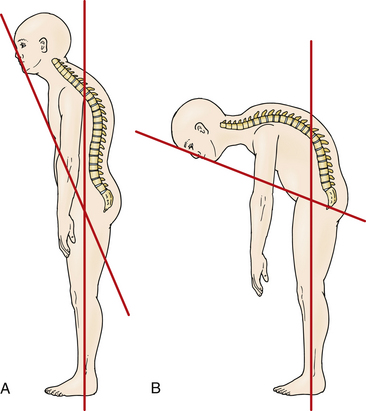
Accurate measurement of the deformity is required for surgical planning. Simmons advocates the chin-brow to vertical (CBV) angle as the most effective and reproducible measurement of deformity.22 The CBV can be evaluated on photographs and is the angle created by (1) the vertical axis of the patient standing with hips and knees extended and (2) the line drawn from the chin to the brow. A greater CBV angle correlates with greater compromise of horizontal gaze and is a critical marker for the degree of deformity (Figs. 99-1A and B).
Normal CBV is 0 degrees but can exceed 90 degrees in severe chin-on-chest deformity. A final corrected angle of approximately 10 degrees of flexion is generally recommended.23 Radiographic evaluation with 36-inch plain radiography is highly recommended.24 Osseous anatomy for instrumentation, existing stenosis requiring decompression, and evaluation of soft tissue or vascular structures like the vertebral arteries can be better delineated on the CT and MRI studies necessary for preoperative planning.25–27 Flexion and extension radiographs can evaluate for instability (particularly atlantoaxial instability) sometimes present in AS.
The technique and location of the osteotomy depends on the region of the spinal deformity that maximally influences sagittal alignment. Overall spinal balance as well as the hips must be evaluated to delineate the primary site of deformity. In some patients, more than one site may contribute to the deformity. The common sites of deformity include the cevicothoracic junction, midthoracic spine, thoracolumbar spine, and hip joints.6 Assuming equal deformity at these levels, lumbar correction surgery should be considered prior to cervical correction surgery because of the lower rate of complications.28
The site of correction depends on the site of deformity. Deformities isolated to the lumbar spine are corrected by a lumbar osteotomy procedure. The osteotomy is preferred below the level of the conus medullaris and is usually performed at L3 to avoid acute angular correction at the cord level.22 Most thoracolumbar kyphotic deformities can be addressed through a single lumbar osteotomy. The correction should be planned so that the plumb line from C7 falls within the body of S1. Even in cases in which the thoracic kyphosis is greater than normal, a compensatory lumbar osteotomy may correct sagittal plane malalignment and allow the patient to have forward gaze with the hips and knees fully extended. In cases of severe thoracic kyphosis, where the lumbar and cervical lordosis have been at least partially maintained, thoracic osteotomy by a combined ventral and dorsal approach may be indicated. It is important to note that due to fixed cervical deformity, overcorrection of the gaze angle can cause significant gait difficulty. When the primary deformity is at the cervicothoracic junction with a chin-on-chest deformity, an osteotomy of the cervical spine is indicated. The C7-T1 junction is the preferred location because it places the osteotomy below the entrance of the vertebral arteries into the transverse processes at C6 and uses the relatively large spinal canal–to–cord area ratio to safely obtain correction.
The influence of severe hip flexion contractures, with or without associated hip joint disease, is critical in the preoperative assessment. Soft tissue release about the hips, or more commonly, total hip joint arthroplasty, may be sufficient in itself to allow the patient to stand reasonably upright and see straight ahead, irrespective of the spinal deformity.29 These procedures should be performed prior to any larger surgical correction of spinal deformity.
Diligent presurgical screening is paramount since AS patients frequently have multiple comorbidities.24 Preoperatively, patients with a fixed thoracic deformity should be screened for cardiac and pulmonary abnormalities that can be associated with extra-articular manifestations of AS. Although pulmonary function abnormalities secondary to decreased thoracic expansion have not carried anesthetic risk for most patients, 10% will have cardiac pathology, generally either aortic stenosis or conduction abnormalities.30 Nonsteroidal anti-inflammatory agents may need to be halted prior to surgery to reduce the risk of pseudarthrosis and nonunion. Nutrition should be optimized, sometimes with tube feeding or parenteral nutrition in extreme cases, especially with postoperative risks of swallowing difficulty.
Surgical Correction
Smith-Petersen Osteotomy
Smith-Petersen and Larson first proposed their osteotomy for the correction of flexion deformity for rheumatoid arthritis in the lumbar spine on six patients in 1945.31 Since that time, the Smith-Petersen osteotomy (SPO), also known as the opening wedge osteotomy and extension osteotomy, has been used extensively and optimized for AS. It has been reported primarily in the lumbar and cervical spine.
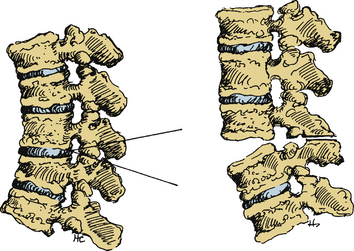
Smith-Petersen originally performed a V-shaped wedge resection osteotomy at the L1, L2, and L3 levels (Fig. 99-2).31 In the original operation, the L2 spinous process was removed completely along with the articular processes of L1, L2, and L3. This dorsal osteotomy wedge was then closed and the deformity corrected via forceful manual manipulation through hyperextension. This maneuver used the middle column (e.g., the posterior longitudinal ligament) as a fulcrum and caused disruption of the anterior longitudinal ligament with a monosegmental opening wedge and extension of the anterior column. Local bone grafts were placed across the osteotomy sites, and the patient was immobilized in a postoperative cast for 2 months followed by a back brace for 1 year. Detailed results were not described.
In 1973, McMaster and Coventry reported on 17 patients with an SPO of the lumbar spine using a plaster case with a turnbuckle and hip spica immobilization for postoperative correction (no instrumentation was used).28 They reported an impressive 39-degree correction average, which has been replicated by other authors.32 Twelve of the 17 patients had complications, including 2 deaths and 5 neurologic deficits.
The SPO has also been commonly employed in the cervical spine. In 1953, Mason et al. reported successful correction of flexion deformity of the cervicothoracic spine in a patient with AS.33 They performed the osteotomy distal to C7 to avoid damage to the vertebral arteries. In 1958, Urist reported a successful osteotomy at the cervicothoracic junction in a patient awake under local anesthesia.34 However, it was Simmons that elaborated on the SPO in the first large case series of 42 patients in 1977.22
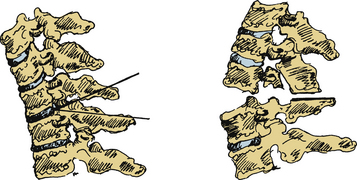
The Simmons SPO modification involved a wide laminectomy from C6 to T1, with osteotomy at the C7-T1 space (Fig. 99-3).22 Simmons resected the entire dorsal arch of C7, the inferior half of C6, and the upper half of T1. The laminae were undercut and foraminotomies performed to prevent impingement of the C8 nerve root. Following bony decompression, Simmons extended the neck and “cracked” the anterior column. Simmons performed the procedure under local anesthesia with halo control and then fixed the halo to a body cast that was worn for 4 months. There were no mortalities, and C8 weakness was the primary morbidity, occurring in 18 patients, with five permanent deficits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree