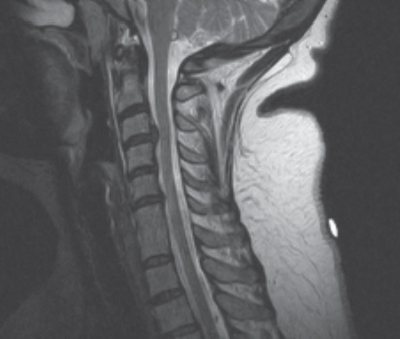
48 What are common findings in cervical disk herniation?1 1. Signs of radiculopathy 2. Neck pain 3. Cervical myelopathy, especially central cord syndrome 4. May be asymptomatic Describe the cervical disk syndrome from a C4–5 disk herniation.2 1. Compression of C5 nerve root 2. Reduction of the deltoid jerk 3. Weakness of the shoulder abduction 4. Paresthesia in the shoulder Describe the cervical disk syndrome from a C5–6 disk herniation. 1. Compression of C6 nerve root 2. Reduction of the biceps jerk 3. Weakness of the elbow flexion 4. Paresthesia of the lateral aspect of the forearm and thumb Describe the cervical disk syndrome from a C6–7 disk herniation. 1. Compression of C7 nerve root 2. Reduction of the triceps jerk 3. Weakness in the elbow extension 4. Paresthesia in the index and middle finger Describe the cervical disk syndrome from a C7-T1 disk herniation.2 1. Compression of C8 nerve root 2. Weakness of intrinsic muscles of the palm 3. Paresthesia in fourth and fifth fingers What are the surgical options to treat a cervical disk herniation?3–5 They are essentially divided into anterior and posterior approaches: 1. Anterior cervical diskectomy with fusion (ACDF) or without fusion 2. Anterior diskectomy and arthroplasty 3. Cervical laminoforaminotomy (and where possible removal of soft herniated fragment) What is the most common complication from anterior cervical approach and what is the cause?6 • Hoarseness of voice is the most common complication of anterior approaches, and it is caused by injuries to the recurrent laryngeal nerve. • It is usually considered safer to approach the cervical spine from the left side, as in the majority of cases the recurrent laryngeal on this side loops posteriorly around the arch of the aorta, and ascends in the tracheoesophageal groove posterior to the left lobe of the thyroid, and therefore is less likely to be encountered during dissection. Fig. 48.1 Midsagittal T2-weighted MRI of the cervical spine demonstrating a C3–4 herniated disk. When is anterior cervical plating considered a viable adjunct to simple ACDF? For multilevel constructs and where there is concern about fusion, cervical plating seems to improve the fusion rate and reduces the risks of postoperative kyphosis. What is the most important radiological exam for thoracic herniated disk?7 CT scan, as it can show the presence of calcifications, which would affect the choice of surgical approach What are the indications for posterior approach in thoracic disk herniation? A posterolateral approach with medial facetectomy is usually sufficient for a lateral disk herniation without myelopathy or calcifications. What approach is indicated for a central thoracic disk herniation in the presence of myelopathy or calcifications? Anterior transthoracic approach Approaching a thoracic herniated disk, what maneuver helps to increase safety?8 Opening of the posterior longitudinal ligament In choosing the rib to be removed, what should be considered? The ribs from T2 to T9 articulate with the superior facet and transverse process of the vertebra with the same number and the inferior facet of the vertebra above. Name a few maneuvers to increase the risks of spinal cord ischemia. • Administer steroids. • Avoid manipulation of the cord. • Maintain mean arterial blood pressure above 80 mm Hg. Which rib is then removed to access the disk space of the diseased level? The rib two levels above Following the lateral extracavitary approach, is fusion always necessary? Only if more than 25% of the vertebra had to be removed to safely remove the disk What are the major risks during a lateral approach to the thoracic spine? • Injuries to the spinal cord • Injuries to the pleura and/or lung Describe some advantages of the lateral extracavitary approach to the thoracic spine. Possibility of circumferential fixation of the spine through a single incision while avoiding the morbidity of a thoracotomy What is a disk herniation?9 A displacement of disk material beyond the boundaries of the disk space How can you classify a disk herniation? 1. Focal (less than 25% of the disk) 2. Broad based (less than 50%) 3. Protrusion (the fragment does not have a narrower part that attaches it to the disk) 4. Extrusion (there is a narrow part attaching the extruded fragment to the disk, a collar, or neck. Extrusions comprise: a. Free fragment: when there is no continuity with the disk b. Migrated fragment: fragment is migrated from the disk site along the axis Fig. 48.2 Midsagittal T2-weighted MRI of the lumbar spine demonstrating an L5-S1 herniated disk. How do disk herniations typically present? • Presentation may be incidental (on an MRI or CT obtained for other reasons) • Patients may present with back or neck pain and radiculopathy following the nerve root level at which the disk is herniated. • If the herniation is above L1 (above the conus), then patients may also present with symptoms and signs of myelopathy. • If the disk pathology is primarily degeneration with only a mild protrusion or bulge, then the presentation may be only axial neck or back pain. How does degenerative disk disease appear on MRI?10 Disk degeneration is associated with changes in signal intensity in vertebral body marrow adjacent to the endplates (Modic changes). Describe the Modic classification of degenerative changes. Type 1: decreased signal on T1 and increased signal on T2, representing bone marrow edema and manifestation of an acute process Type 2: increased signal on T1 and isointense or slightly hyperintense signal on T2, representing marrow fatty degeneration and associated with a chronic process Type 3: decreased signal on both T1 and T2, representing bony sclerosis and yet associated with a chronic process What are the initial conservative treatment options for a disk herniation?11 • Lifestyle and activity modifications, such as losing weight and avoiding heavy lifting or strenuous work • Patient education and reassurance that the symptoms will likely subside if treatment is followed • Temporary bed rest (for about 1 week) • Medications such as NSAIDs What are some second-tier conservative therapies? Second-tier therapies involve a combination of the following: • Physical therapy (such as the McKenzie techniques, traction, massage, ultrasound) • TENS or interferential units • Bracing (lumbosacral orthosis) • Pain management (NSAIDs, short-term weak opioids, muscle relaxers, antiepileptics [e.g., gabapentin] or antidepressants [e.g., amitriptyline]) • Epidural steroid injections/trigger point injections/facet blocks What are some alternative treatment options for low back pain or symptoms of disk herniation? • Chiropractic manipulations (options such as the activator techniques involve minimal manipulation and are safer) • Acupuncture • Prolo therapy • The Alexander technique What is the AHCPR classification?12 • Agency for Health Care Policy and Research • It is a division of the U.S. Department of Health and Human Services that classifies back problems in three categories according to the potential danger. How are back problems classified in the AHCPR classification? 1. Potentially serious, including tumors, infections, cauda equina syndrome, and spinal fractures 2. Sciatica pain 3. Nonspecific back pain What are the worrisome signs (“red flags”) that could lead to diagnose different conditions? • Cancer: • Age >50 or <20 • Suspicion for mass • Unexplained weight loss • Immunosuppression • Fever • Use of recreational drugs • Fracture: • History of trauma • Steroid use • Age >70 • Cauda compression: • Urinary retention or incontinence • Fecal incontinence • Saddle anesthesia • Lower extremity significant weakness What electrodiagnostic tests could be used to investigate a patient with LBP who did not improve after 1 month of conservative treatment?3,4 1. EMG 2. H reflex 3. SSEP 4. NCS How is scoliosis measured?13 Cobb angle: • Draw a line through the superior endplate of the highest vertebra involved and the inferior endplate of the lowest one. • Then draw two perpendicular lines to these. • The angle between them is the Cobb angle. What is the Oswestry Disability Index and what does it measure?14 It is a 10-item questionnaire about activities of daily living. It is used to evaluate back pain. What patients should undergo radiographic evaluation of back pain? Patients with clinical findings consistent with herniated disk or spinal stenosis and who did not respond to conservative measures for an appropriate period of time When is a bone scan with SPECT indicated, and what information can be obtained through this scan?15 • It evaluates facet joint arthropathy and spinal tumors and infections, enhancing the metabolically active bone. • SPECT increases the resolution of the bone scan, which is very useful in the detection of an isolated pars interarticularis fracture in spondylolysis, especially a hairline fracture, which is difficult to demonstrate with other modalities. • Patients with a positive bone scan have an excellent response to facet joint injections when they are administered at the levels where the abnormalities are seen on the bone scan. Treatment of what subset of patients could benefit from the additional information provided by provocative diskography?16,17 • Diskography is especially useful in patients undergoing lumbar fusion to confirm the diskogenic component of the pain. • This technique should always be accompanied by other investigations such as MR and CT. To confirm the level to treat, the pain response to diskography and the MRI findings should be concordant. What are the indications for spine x-ray? • Spinal x-rays are not indicated for evaluation of back pain during the first month after the onset of symptoms. • If signs of serious underlying pathology are present, it is reasonable to take the x-rays before the 4-week mark. In which cases are oblique x-rays indicated? In cases where spondylolisthesis is present on lateral views What are the indications for MRI? MRI is the gold standard to diagnose herniated lumbar disk (HLD) and spinal stenosis. What are pros and cons of MRI? • Advantages include absence of ionizing radiation and better resolution for pathology outside the spinal canal • Disadvantages include difficulties in examination of bone and early bleedings When is CT scan indicated? • Very useful in the setting of trauma to detect fractures and evaluating hemorrhages • Particularly useful in claustrophobic patients • Also useful in patients who have previously undergone surgery to evaluate the extent of bony resection When is myelography indicated and what information can it add?18 • It is of limited use; it is especially useful in gathering information about the CSF flow. • It cannot detect causes of LBP that are external to the dural space such as far lateral disk herniation, and it has limited use in detecting L5/S1 disk herniation because of the so-called insensitive space. • It is especially useful in the setting of prior surgery with instrumentation in place such as pedicle screws (as MRI will provide a poorer image with significant artifact). What are the indications for herniated lumbar disk (HLD) surgery in patients in whom clinical and radiological findings correlate?19 1. Symptoms persistent after 6 weeks of conservative treatment 2. Cauda equina syndrome 3. Progressive neurological deterioration 4. Intolerable pain despite optimal medical management 5. Patient’s preference When is spinal fusion recommended for HLD? 1. In cases with associated spinal deformity or instability 2. In cases with primarily lower back pain axial symptoms and significant degeneration with Modic changes seen on MRI How is sagittal balance assessed?20 On a lateral x-ray a line (“plumb”) is vertically traced from the center of the C7 vertebral body. This line should pass within 2 cm of the sacral promontory within the limits of the L5/S1 disk space. What is the flat back syndrome?21 A loss of lumbar lordosis or kyphosis of the lumbar curve that produces symptoms Why is HLD often off to one side? The posterior longitudinal ligament (PLL) is thicker in the midline. What are the typical symptoms of HLD?22 1. Initial back pain gradually easing off and becoming radicular pain 2. Flexion of the spine with knee flexion can reduce the pain. 3. Increasing the pressure in the thecal sac sneezing or coughing increases the pain. 4. Mild bladder dysfunction, usually starting as reduced bladder sensation and then as a voiding difficulty What are the most common findings in HLD? 1. Normal exam 2. Pain in a radicular distribution 3. Motor weakness 4. Sensory disturbances in a radicular distribution 5. Hyporeflexia What are the most useful nerve root tension tests in HLD?23 1. Straight leg raising (SLR) 2. Bowstring test 3. Crossed SLR 4. Reversed SLR 5. Flexion, abduction, and external rotation (FABER) 6. Trendelenburg What is a nerve root syndrome and what causes it? It represents the symptoms and signs related to a herniated disk at a specific level (reflexes, motor weaknesses, hypo/dysesthesias, pain distribution) Which nerve root is most likely to be affected in a case of posterolateral disk herniation at L4–5?24 It is usually the nerve exiting the foramen below the herniation, in this case the L5 nerve root. What is the Jendrassik maneuver?25 It is a reinforcement maneuver to help relax the patient while eliciting tendon reflexes (e.g., clench the teeth for upper limbs). Name the typical components of L3–4 lumbar disk syndrome.26 1. Diminished knee jerk 2. Weakness of the quadriceps; deficit of knee extension 3. Hypoesthesia of the medial side of the malleolus and foot 4. Pain in the anterior thigh Name the typical components of L4–5 lumbar disk syndrome. 1. Weakness of the tibialis anterior and in 30% of cases also the EHL 2. Hypoesthesia of the dorsum of the foot and big toe 3. Pain in the posterior thigh and leg Name the typical components of L5-S1 lumbar disk syndrome. 1. Diminished ankle jerk 2. Weakness of the gastrocnemius resulting in deficit of plantar flexion and in vast majority of cases also the EHL 3. Hypoesthesia in the lateral aspect of malleolus and foot 4. Pain in the posterior thigh and leg What is the “failed back syndrome”?27 It is a generic term applied to a patient who is unable to return to work after spinal surgery because the symptoms did not resolve or were aggravated, and the patient requires analgesia. What are the surgical and interventional options to treat lumbar radiculopathy?28 1. Laminectomy/laminotomy and diskectomy 2. Microdiskectomy (open or minimally invasive surgery [MIS]) 3. Sequestrectomy 4. Intradiskal procedures (chemonucleolysis, vIdET [intradiskal electrothermal therapy], laser decompression) What is the outcome of lumbar diskectomy for HLD?29,30 65 to 85% of patients are pain free at long-term follow-up, with 10% requiring further surgery. What is an extreme lateral HLD?31,32 A disk herniation distal to the facet (extraforaminal) What nerve root is affected in an extraforaminal disk herniation? The one exiting at that level (i.e., for an L4/5 extra-foraminal HLD, it is L4) How can a lateral disk be approached?8 There are essentially two approaches: 1. Paramedian approach 3 to 4 cm lateral to the midline that allows access to the lateral aspect of the facet joint and transverse process 2. Midline approach with hemilaminectomy and removal of most of the facet joint What is a Schmorl’s nodule? It represents a disk herniation through the cartilage of the endplate into the cancellous bone of the vertebral body. What is meant by the term juxtafacet cyst?5 Juxtafacet cysts arise from the ligamentum flavum or in close contact to a facet joint. They include two types: synovial (if they have synovial lining) or ganglion (if they do not). What is the best treatment for recurrent herniated lumbar disk?33 There is evidence that for a recurrent HLD a redo diskectomy is superior to diskectomy and fusion in cases where spinal instability cannot be demonstrated. What is the most common symptom associated with CSF leak?34 Low-pressure headache If an incidental durotomy is noted intraoperatively, how can it be repaired? 1. If the durotomy can be accessed, primary closure is attempted with nonabsorbable suture. 2. If the durotomy is in the anterior aspect of the thecal sac, one option in the lumbar spine is to perform a posterior dural opening to provide exposure of the involved segment, and primary watertight closure of both durotomies is performed. 3. If the durotomy is on a nerve sleeve, a muscle or fascial patch is applied, reinforced by fibrin glue or blood patch. 4. A spinal drain is inserted. It can help taking pressure off the opening and speed the healing process, especially if it can be placed above the actual durotomy site. What is the lateral recess stenosis, and what are the most common causes of it? The lateral recess is the space between the pedicle laterally, the articular facet of the vertebra above (it is the deeper one in the articulation), and the posterior surface of the vertebral body anteriorly. Any disturbances of one or more of these elements can present a cause of compression at this level (i.e., hypertrophy of the facet joint and/or ligamentum flavum with subsequent spinal stenosis, degenerative spondylolisthesis with movement of the facet joint or presence of reactive juxtafacet cyst, HLD). What are the clinical features distinguishing lateral recess stenosis from disk-related pain?11 In lateral recess stenosis the symptoms are usually elicited by walking, whereas sitting or bending forward (postures that increase kyphosis) help relieve the pain. Disk-related pain is aggravated most of the time by sitting, as there is inevitably more pressure on the anterior elements of the spine and the disk. What is CES?35 It is a clinical syndrome that can result from both compressive and noncompressive causes involving multiple lumbar and sacral nerve roots. What are the most common clinical findings in CES?26 1. Bladder dysfunction (urinary retention) and/or incontinence (also fecal) 2. Sensory deficits (saddle anesthesia) 3. Motor weakness of one or more nerve roots 4. Pain What are the most common causes of CES? 1. Nonneoplastic compressive: HDL, canal stenosis, epidural abscess, subdural hematoma, AVM 2. Neoplastic compressive: schwannoma, ependymoma, lipoma, metastatic tumor 3. Noncompressive: ischemic, inflammatory, arachnoiditis, iatrogenic What is the best timing to intervene in the causes of CES? Surgery should be performed within 48 hours of the onset of symptoms. What is intended by the term pars interarticularis defect?36 A congenital or acquired fracture of the bony bridge joining the superior and inferior facet joints of the vertebra What is intended by the word spondylolisthesis? A subluxation of a vertebral body on another, causing nerve root compression from forward movement of the anterior vertebra while the posterior elements are fixed How can spondylolisthesis be graded? The most used grading system is the Meyerding; it is based on measurement of the percentage of vertebral body slipping in the anteroposterior plane: 1. Grade I: <25% 2. Grade II: 25–<50% 3. Grade III: 50–<75% 4. Grade IV: 75–100% Fig. 48.3 Midsagittal T2-weighted MRI of the lumbar spine demonstrating a grade I spondylolisthesis with severe spinal stenosis at L3–4 in a patient who had undergone prior laminectomies from L4 to S1.
Degenerative Spine Disease
48.1 Cervical Disk Herniation
48.2 Thoracic Herniated Disk
48.3 Degenerative Disk Disease and Lower Back Pain

48.4 Cauda Equina Syndrome (CES)
48.5 Spondylolisthesis and Spinal Instability

Degenerative Spine Disease
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






