DEMENTIA IN CHINA
Prevalence of Dementia
The number of people suffering from dementia in China was estimated to be 5 million in 2001, and it has been projected that there will be a more than 300% increase in this number by 20401.
Since 1980, a number of epidemiological surveys of dementia using standardized instruments and diagnostic criteria have been carried out. However, only a few of these studies have been published in international journals. Dementia prevalence estimates vary widely within China. This variation may be related to differences in population structure, genetics and lifestyle in the country’s various regions, but it may also be due to different mortality rates of dementia and to methodological differences between studies. Chiu and Zhang reviewed 16 studies carried out between 1980 and 1999 and found the prevalence rates of dementia to range from 0.46% to 7.0%2. Dong et al. performed a meta-analysis of 25 Chinese studies that were conducted between 1980 and 2004 and comprised a total population of more than 76 000. They estimated that the overall prevalence of dementia in China was 2.8% in people aged 60 or above3. Alzheimer’s disease and vascular dementia were found to be the most common types of dementia, with the prevalence rate of the former reported to be 1.6% and that of the latter to be 0.8%. Both reviews2,3 found the rates of dementia, particularly that of Alzheimer’s disease, to be lower than those reported in Western developed countries. In addition, Dong et al.3 found that the prevalence of Alzheimer’s disease increased significantly from 1980 to 2004, and reported that the gap in the prevalence of dementia between China and Western countries has been decreasing.
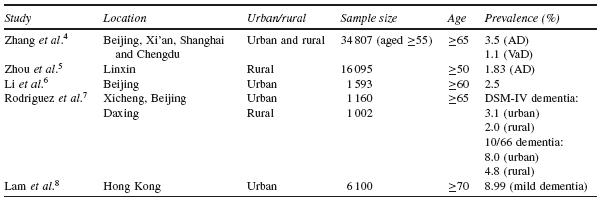
Several epidemiological surveys that examined the prevalence of dementia in different regions of China using larger samples were published in international journals between 2004 and 20084– 8. The initial screening for these surveys was usually performed using the Chinese version of the Mini-Mental State Examination, with diagnoses confirmed through neuropsychological assessment and clinical interviews. The results of some of these studies are presented in Table 117.1. A recent large-scale survey reported that the prevalence rates of Alzheimer’s disease and vascular dementia were 3.5% and 1.1%, respectively. Greater prevalence of dementia was apparent in the northern regions compared with the south, but no difference was found between urban and rural Chinese residents4,9. The burden of Alzheimer’s disease and vascular dementia was not distributed equally among all regions and sociodemographic groups. Significant north– south variation was observed for both Alzheimer’s disease and vascular dementia, but was more pronounced for the latter than the former. In both crude and age-adjusted associations, the prevalence odds of vascular dementia were approximately double in northern areas relative to southern areas. He et al. reported that the northern cities of China have a threefold higher incidence of stroke compared to southern cities, a fact that may be associated with different exposures to such risk factors as hypertension, a diet high in salt, and heavy alcohol and cigarette consumption10. In addition to this north– south variation, Zhang et al. also observed an east– west difference in the prevalence of dementia. Western China is less developed than the east, and life expectancy is also lower in the former. Thus, the lower prevalence rate of dementia in the western part of China may reflect a higher case fatality rate following Alzheimer’s disease onset in the younger age groups or fewer persons at risk of Alzheimer’s disease surviving until the period of onset9.
Incidence of Dementia
Studies on the incidence of dementia in China are scarce. Li et al. examined 1 090 elderly aged 60 or above in Beijing using the DSM-III criteria in a study that lasted from 1986 to 198911. The annual incidence rate of dementia was 0.6%. A similar cohort study was conducted in the same urban district of Beijing from 1997 to 19996. In this study, 1 593 elderly aged 60 or above were examined using the DSM-IV criteria. The annual incidence rate was 0.9%, which was
significantly higher than that reported 10 years earlier. Zhang et al. examined 1 970 elderly aged 65 or above in Shanghai in 1987 and followed them up for five years12. They reported an annual dementia incidence rate of 1.15%. Qu et al. surveyed 2 197 elderly in Xi’ an in 1998 and 200113. The annual incidence rate of dementia was found to be 0.89% among the elderly aged 65 or above. Of particular interest is the common finding that the incidence rate of dementia was higher in the illiterate groups in these studies.
Treatment
Guidelines for the treatment of dementia have been published recently. These guidelines cover the pharmacological and non-pharmacological treatment of cognitive and neuropsychiatric symptoms in dementia. In a section on potential drug treatments, acetylcholinesterase inhibitors (AChEIs) and memantine are listed along with other drugs, such as antioxidants and vasodilators. In clinical practice, huperzine A is used much more often in the treatment of dementia in China than other AchEIs, such as donepezil or rivastigmine, as it is covered by the National Drug Catalogue (China) and is inexpensive. It is an alkaloid isolated from the Chinese herb Huperzia serrata, and it is a reversible inhibitor of acetylcholinesterase. Randomized controlled trials in China have reported huperzine A to have some success in improving general cognitive functioning for patients with Alzheimer’s disease14. The other cholinesterase inhibitors and memantine are not consistently covered by the National Drug Catalogue.
The drugs used in the treatment of neuropsychiatric symptoms include AChEIs, antipsychotics, antidepressants, anxiolytics and mood stabilizing agents. The US Food and Drug Administration (FDA) warning of increased adverse cardiovascular events with the use of atypical antipsychotics in dementia is mentioned in the Chinese guidelines. Such non-pharmacological treatments as reminiscence therapy, validation therapy, reality orientation and behavioural modification are also recommended. These guidelines emphasize the comprehensive assessment of the needs of both patients and their caregivers, as well as a multidisciplinary management approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree