9 Disorders of attention and memory
At the end of this chapter, you should be able to:
• describe the potential effects of cortical, as well as subcortical lesions on attention and memory
• describe the main clinical manifestations of some common disorders of attention and memory
• demonstrate an understanding of the role of attention and memory in learning
• explore the implications that disorders of attention and memory may have for patients with a neurological condition
• define unilateral neglect, describe and explain the common clinical manifestations of this syndrome
• provide different explanations for unilateral neglect
• demonstrate an understanding of the possible implications of neglect for neurological rehabilitation
• demonstrate an understanding of the role of the multi-disciplinary team in the management of patients with neglect
• explore how you would adapt the general theory of motor learning for patients with impaired attention/memory as a result of a neurological condition.
Introduction
Given the prerequisite of attention for learning, and the finding that attentional deficits are common in a number of clinical populations, it is important that health-care professionals have a sufficient understanding of the normal function of attention, the impact of specific health conditions on this function, and the impact that attentional deficits may have on the rehabilitation process. Consider Case study 9.1.
Attention
Attention described
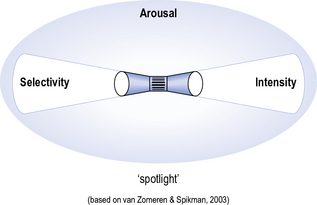
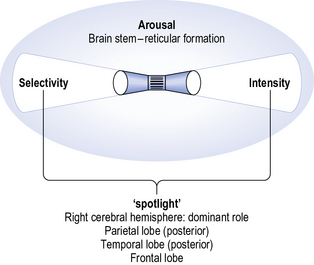
James’ interpretation of attention resembles that of a torch that illuminates certain objects and discerns them from a background of competing stimuli. In a similar vein, van Zomeren and Spikman (2003) more recently compared attention to a ‘spotlight’, which provides both intensity and selectivity.
Additionally, for this ‘spotlight’ to work, one needs to have a sufficient level of arousal, defined by Stuss and Benson (1986) as:
Taken together, attention could be interpreted as illustrated in Figure 9.1, which may help to understand the range of difficulties that patients with impaired attention may experience.
Clinical manifestations of attentional deficits
Disorders of attention are common in neurological populations (Geschwind 1982), especially in patients with head injuries and frontal lobe lesions (Hécaen and Albert 1978). Common signs and symptoms of attentional difficulties include those associated with impaired arousal, ranging from coma, drowsiness, a lack of concentration, through to hypervigilance and panic. Patients may lack a general awareness of what goes on around them, e.g. they may be oblivious to a dispute between fellow patients. Fatigue (see Chapter 14) is a common problem in patients with conditions affecting the CNS, which therapists need to take into account; sessions that may not place a notable cardiovascular or biomechanical load on patients may still induce fatigue due to attentional demands. Overall processing speed may be reduced, which may manifest itself as a learning difficulty. Patients may complain that the usual conversations with their family are too fast, and that they are unable to follow the news on TV. Attentional capacity may be more limited, restricting the amount of information they can take in. In terms of selectivity, patients may have difficulty focusing and sustaining their attention, and as a result they may be easily distracted. This can pose a particular challenge in a busy therapy department (see Clinical box 9.1), where there is a constant source of diversion in the form of other people, moving objects and – in some situations ? music. Multi-tasking, which requires attention to either be divided or switched between one task and the next, may be impossible. Some patients will stop talking when concentrating on a task, or stop practising while talking to their therapist. In terms of intensity, some patients may find it difficult to generate sufficient attention and this apparent apathy may be misinterpreted as a lack of motivation. Other patients may show perseveration, which means that they continue a task even if it has been completed, signalling difficulty with disengaging attention.
Attention and the brain
We will now look at each of these areas in turn.
Reticular formation
The reticular formation (from the Latin reticulum: network, see Chapter 2) is an extensive neural network that connects the thalamus with the cerebrum. Its main functions include regulating the level of arousal, the sleep–wake cycle, and motor activities that involve motivation and reward. It follows that damage to this network (e.g. through a traumatic brain injury, which may cause diffuse axonal tearing) may result in abnormal levels of arousal (e.g. coma, drowsiness), disturbances in sleep–wake rhythm (e.g. the patient may be sleepy during the day, but active at night), or lack of response to incentives.
Right cerebral hemisphere
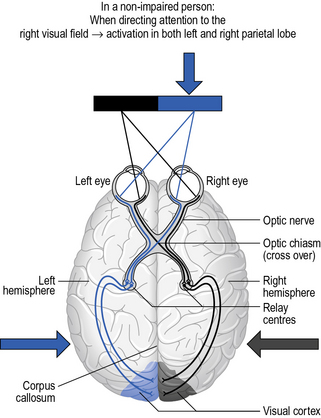
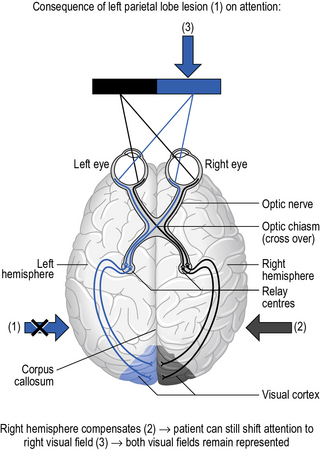
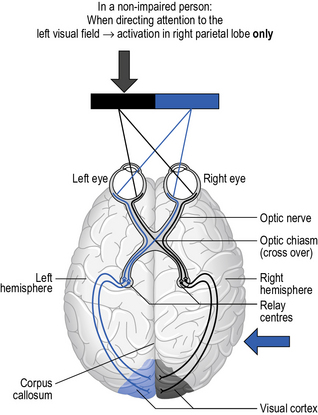
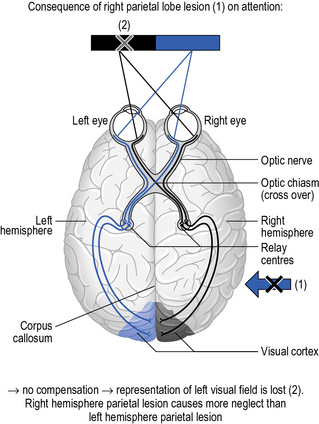
For a reason not readily understood, the right cerebral hemisphere plays a dominant role in attention. Neuroimaging studies have shown that if a person directs their attention to the left visual field, only the right cerebral hemisphere is activated. In contrast, if a person focuses on stimuli in their right visual field, both left and right hemispheres are activated. It follows that if a person sustains a lesion to the left hemisphere, their right hemisphere can continue to focus their attention on the left visual field, and compensate for the damaged left hemisphere when focusing attention on the right visual field. Thus, despite the left hemisphere lesion, there may not be a noticeable attentional deficit. But what happens when the right hemisphere is affected? The patient will still be able to direct their attention to their right visual field, but they will now have difficulty focusing on their left visual field (Fig. 9.2). This scenario is known as hemi-inattention, other terms being hemispatial neglect or unilateral neglect (see later).
Posterior parietal lobe
The posterior parietal lobe is especially involved in focusing attention on a particular location. Refer back to Chapter 5 on the relationship between the brain and behaviour: we saw there that the posterior parietal lobe was responsible for integrating information for planning action in user-centred space. More specifically, this part of the brain is involved in disengaging, moving and re-engaging attention to a particular location. Lesions of this part of the brain (e.g. due to a tumour or stroke) may result in unilateral neglect (i.e. having difficulty shifting attention towards the affected side). More about this syndrome will be discussed later in this chapter.
Posterior temporal lobe
Chapter 5 explained the role of the temporal lobe in object recognition. More specifically, this part of the brain is involved in focusing attention on particular features of an object. Damage to this part of the brain, therefore, often leads to difficulties recognising objects, a condition known as visual agnosia.
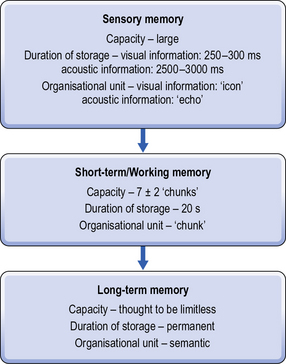
Frontal lobe
The frontal lobe is involved in short-term memory, in the sense that it keeps track of what has just been done. It is also involved in prospective memory (i.e. keeping track of what needs to be done next) and in selecting appropriate actions. Lesions to the frontal lobe (e.g. due to head injuries) impair this process, causing a person to ‘lose track’ of what they are doing and rendering their behaviour disorganised. This type of disorder, which is part of ‘executive dysfunction’ or ‘dysexecutive function’, will be discussed in more detail in Chapter 12.
Taken together, building on Figure 9.1, a simple way to remember the various main brain areas involved in attention is illustrated in Figure 9.3.
Clinical implications of attentional deficits
In Chapter 8, we have seen how attention is a prerequisite for learning; attention is a major control process in the passing of information through to memory – a function that will be discussed in the next section. It is not surprising, therefore, that attentional deficits can present a real bottleneck for rehabilitation. Given the complexity of attention, which comprises a number of different functions, it is not possible to provide a standard protocol for managing attentional deficits. van Zomeren and Spikman (in Halligan et al. 2003) suggest the following pointers:
Think about whether any of these pointers may help you to answer the questions in the clinical application in Box 9.1–and why they might be effective.