INTRODUCTION
Gait, the art and manner of walking, is defined as a learned complex motor skill that facilitates locomotion. Humans have used the bipedal form of locomotion for more than 1 million years. Although it can be performed automatically and without conscious effort, gait requires the integration of mechanisms of locomotion with those of balance, motor control, cognition, and musculoskeletal function (1). The ability to walk is a basic component of quality of life, and is influenced by many disorders, as well as by normal aging (2).
Gait disorders are caused by many neurologic and nonneurologic diseases and often reflect a range of dysfunctions of the central and peripheral nervous systems, the musculoskeletal system, or all. In elderly patients, severity of gait disorders, postural reflex impairment, and the rate of their progression are associated with significant morbidity and mortality (3). The most severe consequence of gait disturbances is falls with risk for head trauma, bone fracture, or the development of fear of falling with loss of mobility and independence. According to Tinetti (4), 30% of elderly persons suffer at least one fall annually, with the figure being 40% among those older than 80 years.
The increased awareness of the importance of gait and postural control to quality of life and functional independence has led many research groups to study the pathophysiology, epidemiology, clinical, and therapeutic aspects of these motor functions. This chapter aims to provide a review of gait disorders that would be applicable to the practice of a clinical neurologist.
THE GAIT CYCLE
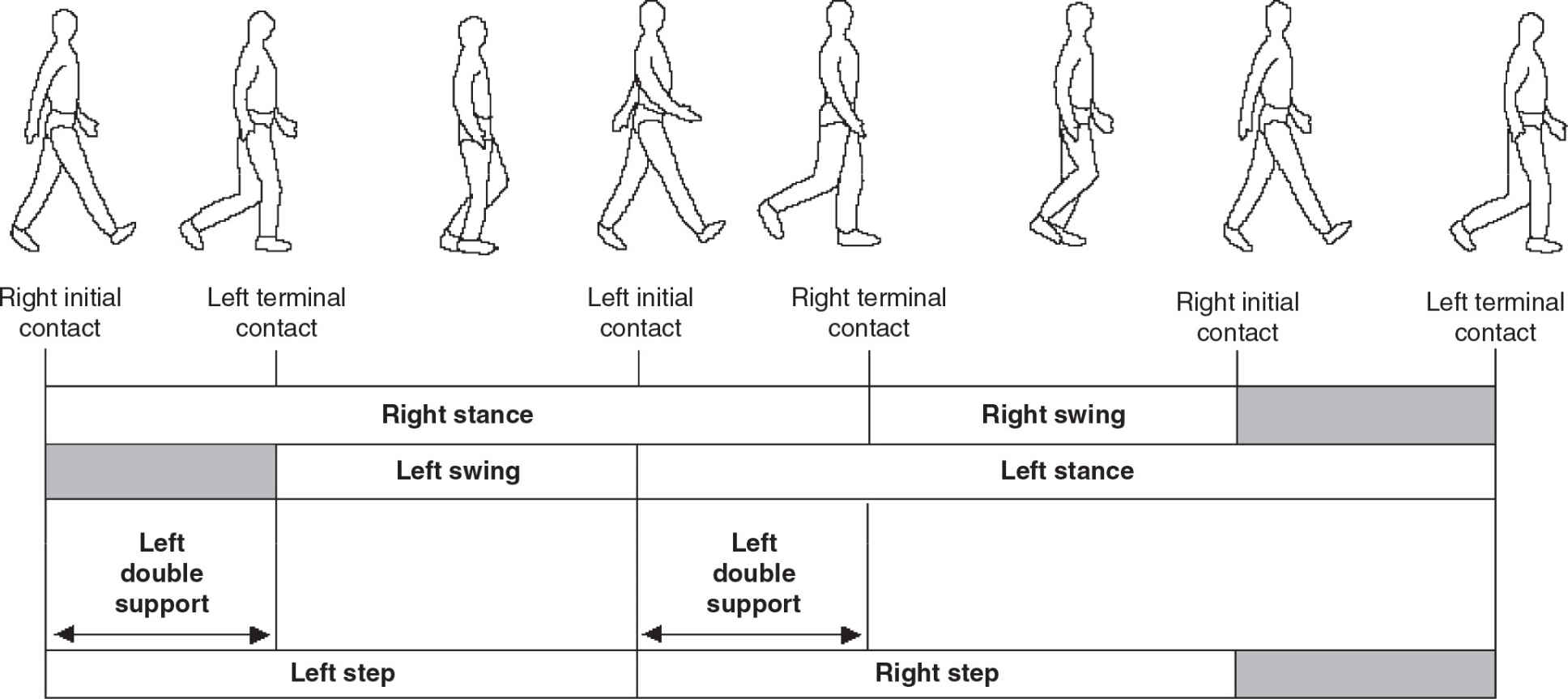
Walking can be regarded as a composite of similar gait cycles. Classically, the gait cycle starts when one heel touches the ground while the ipsilateral knee is extended and the right is dorsiflexed (extended). The foot rolls on the ground and carries most of the body mass as part of the stance phase. As the body mass moves forward, the heel leaves the ground. After a forced plantar flexion that pushes the center of body mass forward, the toes also leave the ground. When the foot toes leave the ground, the swing phase of the leg starts. In the swing phase, the leg swings forward after the hip is flexed while the knee initially will be flexed and later extended to reach the ground in a locked position. During the swing phase, the foot is dorsiflexed to avoid any contact of the toes with the ground. The cycle ends when the heel comes in contact with the ground again (Fig. 36.1).
The gait cycle can also be characterized temporally. Each foot normally touches the ground for about 60% to 65% of the gait cycle. During 30% to 40% of the cycle, only one leg is in contact with the ground (single-support time), and during 20% to 25%, both legs touch the ground (double-support phase). Based on the stated time frame, the swing phase of one leg and the stance phase of the other leg (single-support time of the leg), which are equal in time, take place during 35% to 40% of the gait cycle. The proportion of each phase of the gait cycle is changed in relation to the speed of walking, as well as in relation to the physical state, security, and equilibrium. Accelerated walk is associated with shortening of all phases, but mainly the double-limb support time. Aging, physical weakness, and disequilibrium increase double-limb support time.
Three additional spatiotemporal features of locomotion are stride length, cadence, and step width. Stride length is the distance between the places where the heel first touches the ground at the initiation of one gait cycle to the place where it touches the ground again. Stride length is also the summation of the distances of two steps (left one right). Cadence is the step rate or the number of steps in a given time (e.g., steps per minute), and step width describes the distance between the two feet at the perpendicular axis to the walking direction at a given step.
GAIT AND BALANCE EXAMINATION
Posture, balance, and gait assessment are fundamental parts of the neurological examination (5). Locomotion should be evaluated in an open space, with the patient walking at his or her most comfortable pace for 7 to 10 m, preferably with a turn at mid-distance. Clinical observation in the assessment of gait disturbances is very informative for diagnosis and treatment of gait disturbances. Objective measures used by gait laboratories have an important role in the detection of subclinical disturbances or prior to surgical interventions (6).
GAIT ASSESSMENT
Gait and posture should be assessed as part of the routine clinical examination. Several aspects of gait should be checked:
• Ability to rise from a chair with his/her arms crossed, enables testing the strength of the hip and knee extensor muscles, as well as general postural control.
• Standing capacity, looking at the base of support, the ability to stand with the feet together, in a tandem stand (up to 30 seconds), on one leg (up to 5 seconds), and standing with both feet together and eyes closed (Romberg test). These tests provide valuable information about postural control, balance, vestibular function, and proprioception.
• Challenge test, pulling backward (pull test) while protecting the patient from falling can provide functional information.
• Normal walking in an open space is informative with regard to locomotion, equilibrium, and interaction with the environment.
• Turning in place is informative in terms of general coordination and equilibrium. Turning is best for provoking “freezing episode.”
• Ability to perform another cognitive or motor task while walking (dual tasking) can provide important information about cognitive and motor reserve which is of importance to assess fall risk.
• If the patient reports fear and insecurity or if it is suspected that these features might contribute to the clinical syndrome, the effect of support by a hand, cane, or a walker should be assessed.
• When testing gait, other components of motor function should be assessed (muscle strength, tone, coordination, and range of motion), as should cognition and affect. For cognition, it is important to assess specifically attention, working memory, cognitive slowing, reaction time, executive functions, and visuospatial orientation. Depression and anxiety can be assessed as part of the interview and the examination, but it will more frequently be picked up by validated assessment tools (7).
BEDSIDE (LOW TECHNOLOGY) PHYSICAL EXAMINATION TOOLS
The Timed Up and Go (TUaG) test is a gross measure of locomotion that has been associated with fall risk in the elderly population (8). The person is asked to get up from a chair, walk 3 m, turn 180 degrees, and return to a sitting position in the same chair. Healthy volunteers are able to complete the test in less than 10 seconds. Needing more than 14 seconds to perform the test is a marker for increased fall risk. Performing the test in more than 30 seconds means that there is a severe gait disorder and poor performance on the Barthel Activities of Daily Living Index (9). Recent studies have reported that the TUaG test can reflect about cognitive function and even predicts as a marker, the future development of cognitive decline (10). Furthermore, measuring performance on the TUaG with objective body-fixed sensors (called Instrumental TUaG = ITUG) can be even more sensitive detector of behavioral and cognitive functions (11).
The Tinetti scale was developed to screen for balance and mobility skills in the aged population and to determine the risk for falls (12). It consists of two parts for evaluating balance (16 points) and gait (12 points).
Morse (1998) (13) developed the simpler validated Morse Falls Scale (MFS), which evaluates falls history, the presence of other disorders, the use of walking aids, mental status, and more. This scale has good interrater reliability (r = 0.97) and sensitivity to various medical disorders. A specific risk level carries with it recommended actions for fall prevention: for example, a score of 0 to 24 = no interventions needed, 25 to 50 = standard fall prevention interventions, ≥51 = high-risk prevention interventions.
Many of the above tests and scales have been incorporated in a comprehensive scale, referred to as Clinical Gait and Balance Scale (GABS), which includes 14 different gait and balance parameters designed to assess the severity of this various functional domains (14). The GABS, which has been validated against computerized gait analysis instruments, has been found to have high intrarater and internal item reliability.
LABORATORY-BASED GAIT-ASSESSMENT METHODS
Many different systems are available to capture human movement, but most laboratories generally use three basic ones: (a) a motion-capture system, (b) force plates, and (c) electromyography (EMG) equipment.
Motion-capture systems use camera-based equipment and track and record the trajectories of lightweight reflective markers located on the patient’s skin, plus movements of the patient’s body segments during walking. Using the three-dimensional position data obtained, it is possible to compute joint angle, temporal–spatial, and kinematic data. Temporal data, such as the percentage of time in the swing phase, can provide information about the patient’s developmental stage and movement stability. Joint angle data provide information on the relative orientation of the body segments during the gait cycle.
A force plates system can simultaneously measure the interaction of the foot with the ground. The resultant force generated by this interaction is referred to as the ground reaction force (GRF). The GRF reflects the dynamic effects of the body and the foot’s support of body weight. The examination of the characteristics of the force curves generated can provide information about gait rhythmicity, stride-to-stride variability, gait asymmetry, and freezing of gait (FOG).
EMG is used to determine the intensity of contraction and phasic activity of the lower extremities and axial muscles during locomotion providing insight into the underlying neuromuscular activity during the gait cycle.
GAIT AND MENTAL FUNCTION
Dementia and depression have been shown to be associated with abnormal gait and stride-to-stride disrhythmicity, as well as with increased risk of falls (15). Patients with Alzheimer’s disease are at higher risk to fall and, even if they might be classified by observation as walking normally, gait laboratory assessment can detect significant disturbances (15). Moreover, prospective studies have demonstrated that abnormal walking is a sensitive risk marker for the future development of non-Alzheimer’s and Alzheimer’s dementia (16,17).
Interestingly, walking regularly four to five times a week can delay the development of dementia, further supporting the relationship between cognition and locomotion (18). Aerobic walking also has been found to improve fitness, motor function, fatigue, mood, executive control, and quality of life in patients with mild to moderate Parkinson’s disease (PD) (19).
Another aspect of cognition and gait is the ability to perform street walking while simultaneously paying attention to the traffic, talking on a mobile phone, or simply thinking of something else. Many studies were able to demonstrate that overloading the cognitive function, and especially the executive domain, is associated with decreased gait speed, increased stride-to-stride dysrhythmicity, and deterioration of postural control (20). It has been shown that the degree of dysrhythmicity is associated with the level of executive function, demonstrating that locomotion is heavily dependent on frontal lobe’s function (21).
GAIT DISTURBANCES
The most common causes for abnormal gait in neurological clinics are stroke (21%), PD (17%), polyneuropathies (7%), multiple sclerosis (7%), spinal disorders (4%), and pain syndromes (4%) (22).
CLASSIFICATIONS OF GAIT DISTURBANCES
Gait disturbances can be classified according to the system affected, the phenomenology or objective signs, and the temporal aspects of the disturbance. The system-oriented classification (Table 36.1) helps in deciding at what level the disturbance originates. After a neurologic examination, it is usually not difficult to decide if the gait disturbance originates at the peripheral neuromuscular system, the spinal cord, or the pyramidal, cerebellar, or extrapyramidal systems. It is more difficult to classify gait disturbances when multiple systems are involved, as is frequently the case especially among the elderly population. The term “frontal gait disturbances” reflects the observations that subcortical disequilibrium, “gait apraxia,” and other more poorly characterized gait disorders are the result of dysfunction of the frontal lobe and its multiple connections. Some gait disturbances, however, cannot be classified based on the system-oriented classification. The most common among them is the “cautious gait” syndrome that was part of the high-level gait disturbances subtypes, but its true origin is difficult to diagnose. Cautious gait can be the earliest stage of the frontal disequilibrium gait disorder, as well as the result of a general anxiety state, visual or vestibular disturbances, recent fall with (even trivial) leg or foot injury, or secondary to peripheral problems such as pain, neuropathy, abnormal proprioception, or discomfort walking with high heels.
| System-Oriented Classification of Gait Syndromes |
Peripherally Originating Gait Syndromes
Musculoskeletal
Joints, bones, ligaments, tendons, muscles, peripheral nerves
Sensory
Proprioceptive, vestibular, visual
Centrally Originating Gait Syndromes
Spinal
Spastic paraparesis
Sensory ataxia
Pyramidal
Spastic
Paretic
Cerebellar
Ataxic
Extrapyramidal
Bradykinetic/hypokinetic
Rigid
Dyskinetic
Episodic
High Level
Disequilibrium
“Apraxic”
Unclassified
Cautious/fear of falling*
*The etiology of many gait syndromes is not always readily attributable to a single cause. For example, fear of falling may be due to changes in frontal, vestibular, visual, and/or extrapyramidal function.
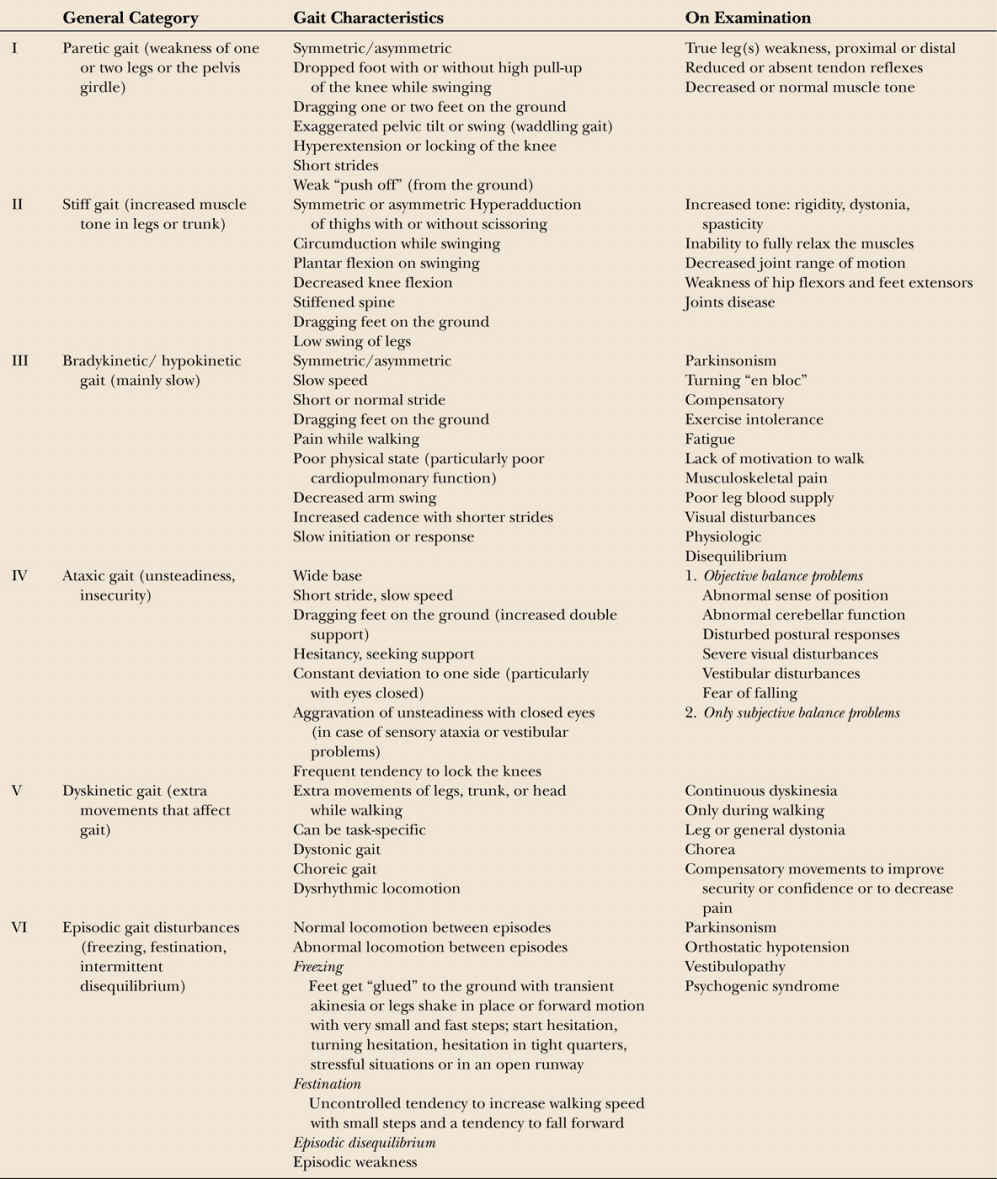
Table 36.2 summarizes the main gait disorders focusing on the clinical phenomenon. We believe that such clinical descriptions of locomotion help characterizing the pathophysiology and also improve the communication between clinicians and researchers. It is a very detailed description that rarely used in everyday clinical assessment, but it can be a very useful teaching tool to improve the way one looks at gait and describe it. In the table, we divided gait into six major clinical categories: paretic, stiffed, bradykinetic\hypokinetic, ataxic, dyskinetic, and episodic gait disturbances (EGDs). Most gait disturbances are continuous in nature, affecting locomotion throughout the day with minimal fluctuations during the day. We subcategorized EGDs, even though it is not a clinical characteristic of locomotion as all others but a time-oriented category, because of its importance to daily function and especially to falls risk (23).
We now describe the six different clinical categories and the main subclinical characteristics based on Table 36.2.
PARETIC GAIT
Paretic gait is associated with weakness as the main clinical feature. Paretic gait is frequently characterized by the compensatory behavioral gait modifications. For example, paretic gait is frequently associated with locking of the knees during stance to avoid collapse at the level of the knee because of weakness at the quadriceps.
Proximal Weakness: Waddling Gait, Duck-like Gait
Weakness affects pelvic girdle muscles and proximal muscles of the leg normally responsible for supporting hip abduction and for keeping the pelvis in a horizontal position while walking. Due to gluteal muscle weakness, the hip tends to tip toward the swing leg and lumbar hyperlordosis develops with the trunk flexing toward the support leg to compensate for this abnormality. The hip and trunk swing from side to side to compensate for the difficulties in lifting the leg. The alternate collapsing of the hip gives the impression of waddling, hence the term “duck-like gait.” Again, because of muscle weakness, rising from a chair can often be accomplished only with the support of the upper extremities. Duck-like, however, may not be always do to proximal weakness and has been, for example, described in “tardive gait” (24).
Distal Weakness: Cock Gait, Steppage, Foot Drop, Flail Foot, Slapping Gait
The most common pattern of gait disorder due to weakness of the anterolateral (peroneal) muscle group takes the form of foot drop as the patient lifts the foot to clear the ground. While walking, to keep the tip of the foot clear of the floor, the walker must flex the extremity excessively at the hip and lift the knee (cock gait). The cock gait or cockwalk is typically seen in patients with manganese toxicity (25), but has been also described in association with polycythemia and chronic liver disease (26).
In the touchdown phase, the foot first rubs against the floor with the great toe or with the anterolateral edge of the foot before putting down the entire sole of the foot (steppage gait). Weakened dorsal flexion of the foot renders patients unable to walk on their heels because they cannot lift the tip of the foot on the affected side.
The involvement of the posterior group of crural muscles is characterized by weakened plantar flexion and leg adduction. While walking, the patient has problems rolling the sole of the foot off the floor and pushing off with the tip of the foot. Instead, the foot comes down flat like a flail (slapping gait, flail foot). In an effort to walk on tiptoe, the foot collapses on the affected side.
Hemiparetic (Hemiplegic) Gait
Hemiparetic gait is seen most frequently following a lesion in the upper motor neuron above the foramen magnum. The weakness is classically at the extensors of the upper limb, which is held in flexion while the arm is abducted at the shoulder due to overactivity of the flexor muscles (spasticity). The lower extremity shows paresis of flexion and is held in extension of the hip and knee, with plantar flexion of the ankle and toes.
Patients with hemiparesis stand and walk with the paralyzed arm flexed and prone and the leg extended. If weakness is the main problem at the initial phase of upper motor neuron lesion, spasticity develops with time, and from a paretic gait, the affected individual will develop the stiffed gait.
STIFF-LEGGED GAIT
Stiff-legged gait is caused by an upper motor neuron lesion (pyramidal or extrapyramidal), but it also can be the end result of joint or muscle disease with secondary decreased range of limb motion. Circumduction is one compensatory response at the swing phase that improves ground clearance of the swinging foot. Stiff gait is a characteristic feature of the stiff-person syndrome (27).
Spastic Gait
Spastic hemiparesis typically produces the characteristic arm flexion at the elbow and ipsilateral leg extension with plantar flexion of the foot. On walking, the spastic leg circumducts in association with contralateral trunk flexion. Spastic paraparesis usually results from lesions of the thoracic portion of the spinal cord and shows spasticity of hip adductors, as a result of which gait is stiff and associated with thigh scissoring, where each leg crosses in front of the other during the swing phase of walking.
Spasticity-based foot deformities later become fixed due to the development of contractures. A detailed classification includes the following seven patterns that are likely to occur separately or in diverse combinations (28).
1. Equinovarus deformity is the most common pathologic position of the lower limb, with the foot and ankle turned downward and inward, mainly as a result of gastrocnemius and soleus hyperactivity. The foot touches down on the lateral edge where a tender bruise often develops. In the swing phase, the foot may rub against the floor and fail to provide support in the stance phase.
2. Valgus foot is bent outward as a result of peroneal muscle group hyperactivity. The foot touches the floor with the medial edge.
3. Hyperextended great toe tends to be a compensatory manifestation in paretically restricted dorsiflexion of the foot.
4. Flexed knee persists in all phases of the walking cycle, forcing the patient to assume a compensatory position in the support phase, and curtailing the stride length due to insufficient extension in the swing phase.
5. Stiff (extended) knee limits movement in the swing phase and leads to foot dragging, which is compensated by circumduction (see the following).
6. Adducted thigh interferes with the swing phase of gait, so that thigh scissoring curtails proper limb advancement (see Spastic Paraparetic Gait). The base is narrow in the support phase and balance may be impaired.
7. Flexed hip interferes with the support function of the extremity, resulting in a permanently flexed trunk and shortened stride.
Circumduction
The leg maintains a stiff posture in extension and rotates in a semicircle, first away from and then toward the trunk, in such a way that the proximal end of the leg is fixed while the distal end moves in a circle. The patient may be able to turn to the paralyzed side more easily than to the normal side. The hemiplegic/spastic gait tends to be slow, with decreased step length and increased stance phase. Compensatory changes include hip hiking from lack of knee flexion of the stance leg, decreased lateral shift over the affected side, lack of heel strike secondary to the plantar flexion of the ankle, and recurvatum of the affected knee. The swing phase is characterized by absent or reduced knee flexion due to quadriceps spasticity. The flexor synergy gait occurs less commonly and consists of hip flexion, abduction and external rotation, knee flexion, and ankle dorsiflexion. This synergy pattern does not allow the person to stand.
Spastic Gait in Cerebral Palsy
The term “cerebral palsy” is comprised of several different motor abnormalities that usually result from perinatal injury. Severe lesions often result in bilateral hemiparesis: Patients stand with legs adducted and internally rotated at the hips, extended or slightly flexed at the knees, with plantar flexion at the ankles. The arms are held adducted at the shoulders and flexed at the elbows and wrists. Patients walk slowly and stiffly with plantar flexion of the feet, causing them to walk on their toes.
BRADYKINETIC\HYPOKINETIC GAIT
Bradykinetic gait is the classic and early feature of parkinsonism. Walking slowly with a short stride and a stooped posture can, however, be the result of general physical weakness, depression, fear, or insecurity.
Parkinsonian Gait
Parkinsonian gait is characterized by a paucity of movement of the facial, trunk, and upper and lower limb muscles, which results in a gait that’s narrow-based, slow, and shuffling with short rapid steps; this tendency to shift from walking to a running pace with small steps as a result of an uncontrolled shift of the center of gravity forward, with an inability to bring it back is called “festination.” The steps are short so that the feet barely clear the ground, and the soles of the feet shuffle and scrape the floor. Such a gait, with characteristically small steps, is termed “marche à petits pas.” The person may also have difficulties with stops and turns. Joint motion is reduced due to rigidity, and there is usually little or no arm swing. The gait in PD reflects a combination of akinesia, impairment of postural reflexes, dystonia, rigidity, and tremor. These patients stand in a posture of general flexion, with the spine bent forward, the head bent downward, the arms moderately flexed at the elbows, and the legs slightly flexed. Although the arms are held immobile, a rest tremor often involves the fingers and wrists. As the patient walk forward, the legs remain bent at the knees, hips, and ankles. Parkinsonian patients often have difficulty when they start to walk after standing still or sitting for a long time. The walking movements may stop involuntarily, and the patient may freeze on attempts to pass through a doorway or into an elevator. EGDs (freezing or festination) are typical in parkinsonian gait and will be discussed elsewhere in this chapter.
ATAXIC GAIT
Ataxic gait is characterized by unsteadiness causing a compensatory widening of the stride base. Unsteadiness can be the result of peripheral neuropathy or disturbance at the posterior column of the spinal cord with abnormal sense of position (sensory ataxia), vestibular disturbance (vestibular ataxia), cerebellar disorder, or frontal disturbance, which is the result of abnormal postural responses (reflexes). Ataxia can also be secondary to a psychological state of fear of falling with no objective balance problem (“psychogenic ataxia”).
Widened Base with Directional Deviations: Veering Gait
Balance disorders and other conditions that aggravate lateral stability force the patient to compensate by widening the base. Typically, the etiologies include disorders of the balance and equilibrium system that is made up of the vestibular labyrinth in the inner ear and the eighth cranial nerve and its brain stem nuclei and connections. Deviations to one side also may be present in lesions of the nondominant parietal lobe associated with sensory neglect of the respective half of the space.
The peripheral vestibular syndrome is a typical cause of veering gait, with patients feeling propelled in some direction and having the illusion that their body or the environment is in motion (vertigo). In extreme cases, attempts to stand up are followed immediately by a fall. Sometimes, the head is held stiff in an effort to control vestibular input. According to observations by Brandt et al. (29), lateral deviations affecting gait in the acute peripheral vestibular syndrome paradoxically abate while the person is running (29). One possible explanation is that running requires the activation of spinal locomotor mechanisms, inhibiting vestibular information. In less-severe cases, the lateral sway will be revealed only upon closing the eyes and in tandem gait. The sway to one side can likewise be elicited by stepping in place with the knees lifted high and with the eyes closed (Unterberger’s stepping test). In the central vestibular syndrome, there is usually no vertigo; there is, however, a tendency for the instability and unsteadiness of posture and gait to deteriorate in proportion to increased motor demands or in the setting of visual input restriction.
Disorders of Proprioception: Posterofunicular Spinal Ataxia and Tabes Gait
Sensory ataxia accompanies disorders of deep sensation from the lower extremities. The patient complains of feeling unsteady when placing the foot down, which can be compared to walking over moss-covered ground or on cushions. This unsteadiness is more pronounced in situations characterized by decreased visual control. Posterofunicular spinal ataxia is identified by a wide-based gait, strides of irregular length, and duration with the feet stepping down hard on the floor and arms held in abduction. Patients must keep looking at their feet and at the floor to avoid falling down. Apart from disordered vibration sensation and sense of position, there is usually areflexia of the lower extremities. Romberg’s sign is markedly positive, although without lateral fall predilection.
Cerebellar Ataxia: Drunken Gait
Ataxia is a major symptom of the neocerebellar syndrome in lesions of cerebellar hemispheres and their connections (30). Cerebellar ataxia gait is marked by a wide base and irregular cadence of steps of unpredictable timing and unpredictable site of foot contact with the floor. Patients are incapable of walking straight ahead: Their deviations follow an irregular pattern. In less-serious cases, difficulties become recognized only in situations that place increased demands on motor coordination (turning around, walking downstairs, or walking in tandem). On examination, signs of a cerebellar syndrome predominate: dysmetria with overshoot of extremity movements, poor coordination, dysynergy of muscles of the extremities and trunk, and rapid alternate movement irregularity (dysdiadochokinesia) (31). Equilibrium is unimpaired, and pull-test responses are hypermetric but otherwise normal (32). Although gait is markedly disordered, falls are relatively rare.
Persons with paleocerebellar syndrome in lesions of the anterior vermis or flocculonodular lobe have different symptoms, with severe postural and gait instability as a prominent sign, as well as a pronounced tendency toward toppling falls (see the following). There are no extremity signs (30).
DYSKINETIC GAIT
Dyskinetic gait, typically seen in patients with PD who experience levodopa-induced dyskinesias, is unique because extra involuntary movements appear while the person walks, making ordinary locomotion look bizarre or dance-like. Because of the involuntary nature, patients sometimes are not aware of the disturbance even if it might lead to tripping and falls. The response of a patient who is aware of such movements is to suppress them voluntarily or incorporate them into the repertoire of normal gait. Ironically, gait might seem even more bizarre by the efforts made to suppress those extra movements.
Choreic Dancing Gait
In choreic gait, lower limb chorea is superimposed on walking movements, thus giving rise to a peculiar ataxic gait pattern reminiscent of ballet dancing. Cadence is entirely irregular: The feet make accidental flat contact with the ground or, if they are turned, any part may touchdown, and they purposelessly jump away from intended directions and the strides or jumps are of irregular length. When these involuntary movements simultaneously affect the trunk and upper extremities, there is a general impression of lack of control and direction. Although patients may sometimes assume highly unusual and unstable positions, falls are rare. When walking, choreic patients speed up and slow down at unpredictable times, with occasional extra steps or skips, give the gait a dance-like appearance.
Dystonic Gait
Dystonic gait may take the form of a simple limp, inadequate stepping down from a higher level, or foot dragging due to dystonic inversion or eversion. Dystonic postures are either constantly present or may appear only in the execution of some activities, such as walking. As a rule, these postures and motions propagate from the lower extremities to other muscle groups. A typical feature is its abatement in response to a variety of “tricks” or maneuvers, such as walking backward, trotting, or dancing. Even sensory tricks, such as putting one’s hands in pockets, around the neck, or behind the back, may improve gait substantially. Bizarre patterns of dystonic gait are sometimes likened to animal gait. For instance, the so-called dromedary gait has been described in cases of progressive lordotic dysbasia (i.e., gradually increasing lordoscoliosis of the lumbar spine in walking, inducing bizarre position of the trunk with the hip bulging backward and sideways and compensatory turning of the shoulders and neck with the head held vertically). Some patients with axial dystonia have such severe flexion of the trunk that it causes marked (even more than 90 degrees) stooping, so-called camptocormia. Camptocormia may be caused not only by axial dystonia but a variety of other disorders (33).
Characteristic features of these dystonic gait patterns include climbing movements of the legs or swinging flexion of the hips, often with contortion of the neck, trunk, and upper extremities, sometimes simulating wing-like movements (34). Patients with axial dystonia often adopt a variety of sensory tricks or alleviating maneuvers, such as walking backwards (33).
EPISODIC GAIT DISTURBANCES
EGDs are unique and most dangerous because of their association with falls (35). The unexpected and heterogeneous nature of the freezing or festination episodes can catch the patient unprepared, leading to inevitable falls. EGDs are sometimes difficult to quantify because they appear more frequently at home and not in the examination room or the gait laboratory (36). FOG can be defined as short (rarely exceeding 30 seconds), intermittent episodes of an inability to initiate or maintain locomotion or perform a turn. Most episodes are associated with a subjective feeling that the feet are “glued” to the ground. Patients either accept the situation and wait for its spontaneous disappearance or actively try to overcome the block, an effort that frequently causes ineffective movement forward with small steps (shuffling forward) (37). FOG episode is frequently associated with tremor-like movements of both legs in place, a phenomenon that may reflect the effort to overcome the block or an associated dystonic jerks which could be part of the FOG itself (35). Typically, most episodes can be overcome by motor, sensory, or mental tricks, but habituation has been described (38,39).
FOG episodes can be provoked most easily by asking the subject to turn around (36,40). In terms of everyday motor behavior, however, 360- or even 180-degree turns are rare and, as a result, start hesitation is experienced relatively more frequently in daily life (41). Other types of FOG occur while walking, passing through tight quarters, reaching the destination, or in stressful situations (40).
Phenomenologically, movement during FOG can be divided into three categories: small steps forward, trembling in place, or complete immobility (akinesia) (40,42). The three categories may be partially related to the amount of effort the patient expends to overcome the block. FOG appears to become more and more dynamic, less frequent, and of shorter duration as levodopa takes effect and parkinsonian symptoms improve (40).
Festination gait (FSG) is an intermittent episode that lasts a matter of seconds and involves disturbed locomotion characterized by uncontrolled propulsion associated with rapid small steps. Patients report a feeling that they were “pushed from behind” (43). Both FOG and FSG are similar in their transient nature, but the latter is experienced mainly during free walking, whereas the former is experienced more frequently during turning or initiation of walking. The two also differ in the unique subjective feeling that accompanies each: the feeling that the feet are “glued” to the ground in FOG and the feeling of being “pushed” by someone from behind in the FSG.
Although FOG is considered a typical sign of PD and has been traditionally attributed to dopaminergic deficiency, there is growing body of evidence that nondopaminergic systems play an important role in mediating this parkinsonian gait disorder (41). In addition to noradrenergic deficiency, the cholinergic system also appears to be involved in FOG. In a cross-sectional study involving 143 PD patients using PET imaging, patients with FOG had lower dopaminergic striatal activity, decreased neocortical cholinergic activation, and greater neocortical deposition of β-amyloid compared to nonfreezers (44). It has been postulated that in patients with FOG, the motor program for gait is intact, but the patients have difficulties accessing it. Indeed, neuroimaging studies have provided evidence that PD-related FOG is due to impaired interactions between frontoparietal cortical regions and subcortical structures, such as the striatum, and that FOG is due to decoupling between the cortical cognitive control network and the basal ganglia network (45,46). Furthermore, high β-oscillations in the subthalamic nucleus suggest that this high oscillatory activity might interfere with the frontal cortex–basal ganglia networks, which contributes to the pathophysiology of FOG in PD (47).
FOGs may improve with levodopa, but some patients with PD have FOG in both off and on states, especially in the more advanced stages of PD and when associated with progressive supranuclear palsy (PSP), vascular parkinsonism (48), or pure freezing syndrome (49). In contrast, festination is rarely improved by dopaminergic treatment. Both FOG and festination respond dramatically to cues and sensory or behavioral tricks or other alleviating maneuvers (43). Episodic disequilibrium is another distressing gait disorder that leads to sudden feelings of instability. The pathophysiology can be of a vestibular, hemodynamic hypoperfusion, or psychogenic nature. Fear of falling is a frequent consequence of EGDs. The psychological aspect of EGD is sometimes even more disabling than the physical difficulties.
Not all gait disturbances can be classified according to the six major categories previously presented. The most difficult group to characterize is that of frontal and psychogenic gait disorders.
FRONTAL GAIT: APRAXIC, DISEQUILIBRIUM, NORMAL-PRESSURE HYDROCEPHALUS
Frontal gait is seen in normal elderly people. It is characterized by a slightly widened base, shortened stride, slowness of walking, and turning en bloc. There is no hesitancy in the initiation of gait and no freezing or shuffling, and the rhythm of walking and foot clearance is normal. There is mild disequilibrium in response to a push and difficulty in balancing on one foot.
Frontal Gait Disorder
Frontal gait disorder is a disturbance that is often seen with multi-infarct dementia or vascular parkinsonism (50). Patients stand on a wide or normal base and take short shuffling steps. Typical FOG may sometimes be present. Moderate-to-severe disequilibrium is the next characteristic feature, and the individual may experience fear of falls. The patient usually feels considerable emotional relief and is able to walk better with external help. Associated findings could include frontal cognitive disturbances, pseudobulbar palsy, asymmetry of tendon reflexes and frontal release signs as well as urinary urgency, or incontinence.
Subcortical Disequilibrium
This gait disorder is seen with PSP and multi-infarct dementia. Patients have marked difficulty maintaining the upright posture and show absent or poor postural adjustments in response to perturbations. Some patients hyperextend the trunk and neck and fall backward (especially in PSP).
Frontal Disequilibrium
Many patients with frontal disequilibrium cannot rise, stand, or walk; some cannot even sit without support. When they try to rise from a chair, they lean backward rather than forward, and they cannot bring their center of gravity in between their feet. When they attempt to take a step, their feet frequently cross and move in a direction that is inappropriate to their center of gravity. Clinical examination usually reveals dementia, signs of frontal release, motor perseveration, urinary incontinence, pseudobulbar palsy, exaggerated muscle stretch reflexes, and extensor plantar responses. In some patients, however, psychogenic gait disorders may be difficult to diagnose. Atrophy of the vermis or epidermoid of the cerebellum can, however, result in frontal gait disorders with similar clinical manifestations (51).
PSYCHOGENIC GAIT DISORDERS
Psychogenic disorders of gait are very common in patients with psychogenic movement disorders, although they are relatively uncommon causes of gait disorders in general (52). They were encountered in 3.6% (530) of patients studied in a movement disorders clinic over a period of 16 years (53). The available information permits only a few general diagnostic principles. The first is that not all kinds of gait that appear bizarre are psychogenic in origin (54). Diagnosis must be based not only on the signs generally accepted as being nonorganic during the clinical examination in real time but also on data collected from video recordings (55). An unusual and illusive presentation of hysterical gait is known as “astasia-abasia.” In this condition, the patient is unable to turn or walk but retains normal use of the legs while lying in bed.
Patients with psychogenic parkinsonism may seem similar to those with organic PD, but often exhibit abrupt onset, typically in response to a stressful event, they tend to have nondecremental slowness when performing repetitive movements, voluntary resistance against passive movement without cogwheel rigidity, distractibility, generalized and “give-way” weakness, stuttering speech, and a variety of behavioral, sexual, and other motor and nonmotor symptoms (56). Furthermore, their symptoms may improve with placebo (e.g., carbidopa).
There are seven major features characteristic of functional gait disorders, which were initially elaborated by Lempert et al. (57):
1. Unilateral weakness of a leg, with it dragging behind the body as an alien object or a “log”: The hip is either held in external or internal rotation so that the foot points inward or outward. This may be associated with a tendency to heave the leg onto an examination couch with both hands.
2. Excessive slowness: Exaggerated delay in gait initiation and subsequent “foot-sticking.”
3. Falling toward or away from the doctor: Falls were the most frequent posture disturbances (51).
4. “Walking on ice” pattern: This pattern is similar to the gait of a normal person walking on a slippery surface, that is, cautious, broad-based steps with decreased stride length and height, and stiff knees and ankles.
| Classification of Gait Disturbances by Clinical Presentation* |
Continuous: Occurs consistently with locomotion (can vary in severity)
Ataxic: Disequilibrium and hypermetria of stance and gait
Somatosensory
Vestibular
Cerebellar
Spastic: Associated with increased postural tone
Hemiparetic
Paraparetic/tetraparetic
Bradykinetic/hypokinetic: slow or small steps and/or slow or small postural responses
Dyskinetic/choreic/dystonic: Involuntary movements
Paretic: Associated with muscle weakness or paralysis
Trunkal: Static, axial postural deformities
Antalgic: Secondary to musculoskeletal or central pain
Higher level (frontal)
“Apractic”
Anxious, fear of falling, cautious
Bizarre
Severely depressed
Psychogenic
Undetermined: Sometimes, it may be difficult to classify the continuous nature of the gait disturbance.
Episodic: Occurs intermittently during locomotion (may vary in severity and frequency)
Freezing: Transient inability to create effective stepping
Festination: Unintentional increase in speed, usually with small steps
Disequilibrium: Transient loss of balance
Mixed types: Where a person suffers from more than one continuous disturbance, or continuous and episodic disturbances, for example, are possible