Chapter 98 Disturbed Dreaming as a Factor in Medical Conditions
Abstract
Beyond common nightmares (see Chapter 97), dreaming disturbances appear as defining or comorbid symptoms of many medical conditions (Table 98-1). In this chapter, these disturbances are classified as falling along a continuum of increasing vividness or intensity, particularly of the apparent reality of the dream experience. At the lower extreme of this continuum, dream recall can cease or the realism of dream content can become impoverished in some respect. At the higher extreme, dream recall can become excessive or dream content unusually vivid and emotional, often being confused with reality or rigidly repetitive in structure. The full range of human emotions, be they dysphoric or euphoric, can appear in disturbed dreams (Fig. 98-1).
Table 98-1 Medical Conditions in which Dreaming is Disturbed
| DISTURBANCE | CONDITIONS COMMONLY AFFECTED | ESSENTIAL FEATURES |
|---|---|---|
| Global cessation of dreaming | Complete loss of dream recall; often sudden onset consequent upon illness or medical procedure | |
| Impoverished dreaming | Reduction in recall, vividness, or complexity of dreaming | |
| Excessive dreaming | Dreaming seems to continue throughout the sleep period; can involve dream vivification or banal or repetitive dream content | |
| Repetitive dream content | Frequent recurrence of repetitive or episodic memory content, e.g., features of prior trauma, epileptic aura, or cardiac symptoms | |
| Dream–reality confusion | Dream vivification; banal episodic content may be confused with actual events |
ICU, intensive care unit; PTSD, posttraumatic stress disorder; RBD, REM sleep behavior disorder.
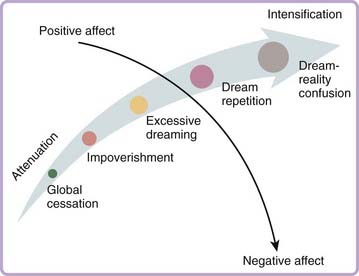
Figure 98-1 Dream disturbances may be conceptualized as falling along a continuum that captures variations in dreaming’s natural capacity to simulate waking-state experiences of reality (see Chapter 51 for discussion). On the x-axis, disruption of reality simulation during dreaming varies from one extreme of attenuation, associated with cessation and impoverishment of dreaming, to the opposite extreme of intensification (vivification), associated with excessive dreaming, content repetition, and complete confusion of dreaming with reality. On the y-axis, the reality simulation capacity is largely independent of the emotions represented in the dream, which can vary from positive to neutral to negative. However, the intensity of dreamed emotions likely does co-vary with the intensification of reality simulation.
The intensity dimension of disturbance varies globally in how intensely real the dream experience appears. As described in Chapter 51, reality simulation is widely viewed to be a basic function of the dream-production mechanism, approximating both the process and the contents of typical waking experience. One notable feature of this mechanism is the heightening of perception-like imagery or emotion to the point of equaling or exceeding what is normally perceived or felt during wakefulness. A second notable feature is the increased presence of episodic memory material in dream content. Such material is usually restricted to mere fragments of remembered (episodic) experience (see Chapter 55), but it can become more salient in replay nightmares (see Chapter 53), repetitive dreams, and so forth. Both of these features are likely in play during the most extremely intense dreams, such as those occurring in intensive care unit delirium or dream-reality confusion.
Global Cessation of Dreaming
About a third of patients with neurologic illnesses report having ceased dreaming altogether.1 Solms1 and Doricchi2 report that parietal lobe involvement differentiates patients with and without global cessation of dreaming (GCD); 42% of GCD patients have parietal lesions and an additional 7% have lesions in proximity to parietal lobe.1 Frontal lobe lesions characterize some patients (8%) with GCD,1 which is consistent with the reduced dream recall that follows upon frontal lobotomy3 (but see reference 2). An additional 43% of GCD patients have diffuse and nonlocalizable lesions.1 It is noteworthy, however, that few such patients are subjected to rigorous REM sleep awakenings to determine whether the capacity for dream recall under optimal conditions is, in fact, absent. Such studies might reveal that many patients who appear to have GCD instead have dream impoverishment.
Impoverished Dreaming
Dream impoverishment is an attenuation, but not total cessation, in the recall, length, vividness, emotionality, or narrative complexity of dream imagery. Impoverished dreaming has been documented for some types of brain syndromes, for patients with alexithymia, and for patients with posttraumatic stress disorder (PTSD), who also have a high incidence of comorbid alexithymia.4
Impoverished Dreaming in Brain Syndromes
In chronic brain syndrome, dream recall from REM sleep deteriorates as the illness progresses from mild (57% recall) to severe (35%) to aged and severe (8%).5 In patients with Korsakoff’s psychosis caused by chronic alcohol abuse, near-normal REM sleep time (29.4%) but poor dream recall (3%) is observed.6 Patients who have permanent amnesia for recent events due to mild encephalitis also have impoverished dreaming; the frequency of their REM awakening reports (28%) is less than normal (75%), and the reported dream content is simple, nonsymbolic and repetitious, stereotyped, and lacking in emotions and day residues.7 Impoverished dream recall has been noted following left8 but not right9 hemispherectomy and supports the more general conclusion10 that left hemisphere processes are more critical for dream generation than are right hemisphere processes.
Impoverished Dreaming in Alexithymia
Alexithymia refers to a difficulty in verbalizing emotions, literally, to a lack of a lexicon for describing feelings. Early investigations of patients who have psychosomatic disorders linked an alexithymic response style with diminished dream recall11 and an absence of affect in dreams.12 Reduced dream recall among alexithymic patients has since been replicated and linked with the difficulty identifying feelings subscale.13,14,14a One study of subjects with nocturnal asthma15—a population in whom comorbid alexithymia is common—revealed that REM sleep awakenings produced an elevated incidence of impoverished dreaming, especially dreams reported with short sentences and the frequent impression of dreaming but without recall of specific contents.
Studies have reported evidence that specific sensory and structural features in dreams are impoverished among alexithymic patients. One study found that alexithymic patients reported colorless dreams16 and a second found that subjects with nonclinical alexithymia had less fantastic dream content than did controls but did not differ on other measures of dream recall and emotion.17
Sleep studies have not yet identified a consistent pattern of changes that might explain dream impoverishment. In one study,18 higher alexithymia scores were associated with more frequent REM episodes, shorter REM latencies, and more stage 1 sleep during and immediately after REM sleep. However, alexithymia was also related to increased NREM stage 1 and decreased NREM stages 3 and 4. In a second study,19 alexithymia scores did not correlate with any polysomnographic variable or with REM density; however, an association with shortened REM latencies was observed. Finally, alexithymia is reliably associated with certain sleep disorders, including chronic insomnia and parasomnias.16
In sum, although converging evidence indicates that dream impoverishment is associated with alexithymia, more research is needed to clarify relationships between alexithymic factors and various attributes of dream recall, content, and emotion and sleep polysomnography. It also bears noting that other patterns of disturbed dreaming characterize some alexithymic patients, such as dreams that are extremely macabre, nightmarish, or lacking in ego and emotional control.20 A similar paradoxical combination of both impoverished and nightmarish dreams is also found among some PTSD patients.
Impoverished Dreaming in PTSD
In contrast to the high prevalence of nightmares in PTSD (see Chapter 53), one long-term consequence of PTSD appears to be impoverishment of some dreaming attributes (for review see reference 21). Both home and laboratory studies indicate that PTSD patients have lower than normal levels of dream recall and that dreams tend to be brief, to deal with trivial daily events, and to be associated with paradoxically high REM densities.22 One laboratory study of disturbed dreamers found dream recall 42% to 54% of the time compared with 89% to 96% for controls.22 Similarly, a group of 12 “well-adjusted” PTSD patients had a lower dream-recall rate from REM sleep (33.7%) than did 11 less-adjusted (50.5%) and 10 control (80%) subjects.23 Well-adjusted patients reported less complex, less salient dreams; fewer dreams with anxiety, aggression, and conflict; and higher denial of emotions toward their dreams.
In contrast, a few studies failed to demonstrate reduced dream recall in PTSD patients24,25 although one has reported that laboratory dream recall is negatively correlated with trauma severity.25
Two, likely interrelated, explanations for these findings have been suggested. First, dream impoverishment in PTSD might reflect an adaptive response or strategy that reduces dream recall and thereby suppresses the occurrence of nightmares.23 Second, mechanisms producing dream impoverishment in alexithymia might also be implicated in PTSD because of its high incidence of comorbidity with alexithymia4; up to 85% of PTSD patients may be alexithymic.26 Hyperarousal and emotional numbing may be common to the etiologies of both conditions. Emotional numbing (considered equivalent to alexithymia in PTSD4) is best predicted by the number of hyperarousal symptoms in PTSD patients.27 PTSD patients might expend so much cognitive, behavioral, and emotional effort on managing hyperarousal and reactivity that they exhaust their emotional resources including, possibly, a depletion of catecholamines.28
Excessive Dreaming
Several conditions are characterized by dreams that are excessively abundant or intense. Epic dreaming refers to complaints of excessive dreaming combined with daytime fatigue.29,30 Patients complain of dreaming all night long about continuous physical activity, often of a banal nature, such as repetitive housework or endless walking through snow or mud. Sensations of acceleration or spinning are also reported. Such dreams occur nightly in 90% of affected patients, and comorbid nightmares are reported by 70%.29 Unlike nightmares, however, epic dreams can lack vivid emotion altogether. The endless dreaming and feelings of fatigue can produce distress, which leads the dreamer to seek medical consultation. No clinical abnormalities have been observed, leaving its etiology and pathophysiology unclear. Cognitive, relaxation, and drug-based treatments and hypnosis have proved ineffective.29 Comparative studies of epic dreams and nightmares might clarify whether their repetitive motor imagery is a type of nightmare stripped of its emotions.
Excessive dreaming characterizes some patients with brain lesions1 and includes increases in both dream frequency and vividness.31 Some patients also report dreaming the same content throughout the night, despite intervening episodes of wakefulness.1,31 Neuropsychological evidence suggests anterior limbic system involvement.
Excessive, vivid, and early-onset dreaming can also appear after withdrawal from certain medications such as tricyclic antidepressants32 and short half-life serotonin reuptake inhibitors such as paroxetine or fluvoxamine (see Chapter 48).33
Repetitive Dream Content
Dream content repeats itself so often that a repetition dimension of dreaming has been postulated.34 The recurring emotions and themes of nightmares and other typical dreams exemplify this. Here, I consider mainly dreams that occur in conjunction with a medical condition and for which their content, structure, or affective quality has become so highly repetitive that it causes patients distress. Neurobiological and psychological features of the concomitant medical condition are widely thought to shape the repetitive content of such dreams.
Assault and Defense Dreams in REM Sleep Behavior Disorder and Parkinsonism
REM sleep behavior disorder (RBD) is characterized by sleep-related motor activity that appears to enact the patient’s ongoing dream or nightmare.35,36 Dream-enacting activities were reported by 93%, 87%, 82%, and 64% of patients in four large samples (N = 93, 96, 91, and 52, respectively). Polysomnographic (PSG) evidence suggests that RBD patients do not enact all of their REM dreams, although their partial enactment is suggested by elevated levels of muscle tone (e.g., submentalis37). Patients do not always recall dream content for specific episodes, possibly because most patients are elderly and have reduced dream recall or because some of the dreams lack salience. Nonetheless, a majority of patients report retrospectively that their dreams are more vivid, violent, action-filled, and nightmarish since the onset of their RBD.38
Clonazepam suppresses dream-enacting behavior and the disturbing dreams accompanying them.39 Pramepexole and melatonin have limited effects; melatonin appears to re-establish REM atonia.40
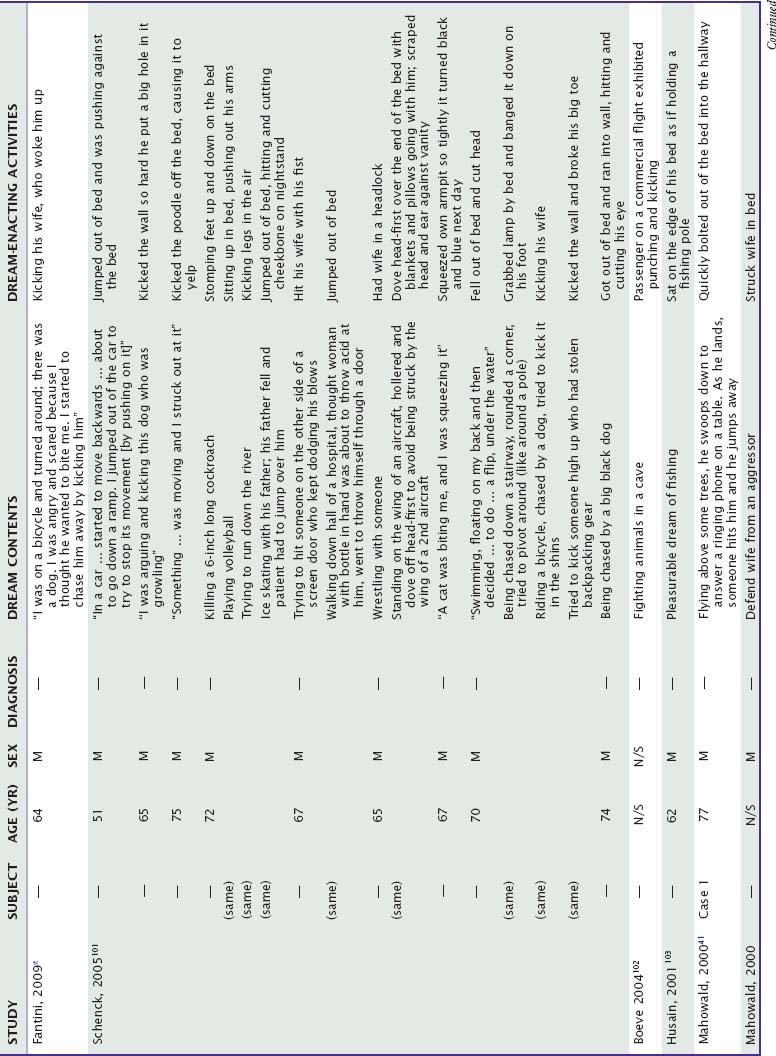
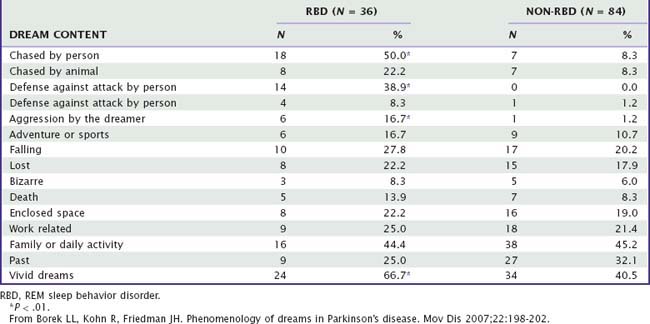
Although a panoply of dream-enacting activities has been reported, associated dream themes are largely repetitive in their structure and emotional content.41,42 This is shown in Table 98-2, which summarizes examples of dreams for which specific enacting activities have been identified by authors. The most common repetitive pattern is that of imminent threat (29/37 or 78.4%), to which patients reacted with vigorous defensive actions (19/29 or 65.5%), attempts to escape (24.1%), or unspecified reactions (10.3%). Most threats (16/29 or 55.2%) were from humans; the rest were from animals (37.9%) or machines (6.9%). Six (6/37 or 16.2%) pleasurable dreams were also reported. Similar results have been reported for a sample of 37 RBD patients reporting dreams to their physicians43: 89% were aggressive in nature and attacks were by humans for 57% of patients and by animals for 30%. Another study of RBD dream content (Table 98-3) reveals similar fractions (e.g., chase by humans, 50%; chase by animals, 22%).44
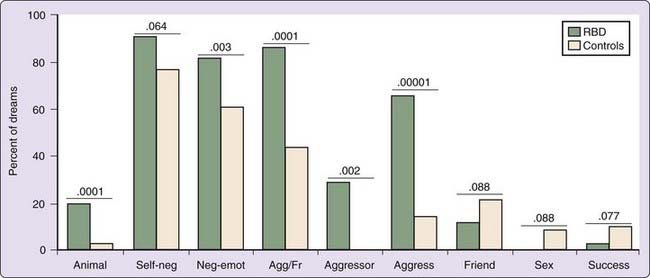
Although RBD patients report more dreams with aggressive interactions (especially self as aggressor) than do controls (Fig. 98-2), they do not have higher scores on a daytime Aggression Questionnaire; in fact, they score lower than controls on physical aggressiveness.45 Dream aggression may be less prevalent for female RBD patients; compared with male RBD patients, their dreams are nonviolent, contain only fear (rather than anger and fear), and do not depict physical confrontation with an assailant.44 Samples of women studied to date are small, however.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree