12
CHAPTER
![]()
EEG of Epilepsy
Rajdeep Singh
EEG is largely a recording of excitatory and inhibitory postsynaptic potentials generated by the large vertically oriented pyramidal neurons located in layers 3, 5, and 6 of the cerebral cortex. The EEG recording has limited specificity in terms of localization and spatial analysis as various factors such as dipole orientation, volume conduction, synchronization, and evolution of ictal activity can influence the final recording. However, despite advances in medical technology, including functional neuroimaging and recording magnetic brain field with magnetoencephalography (MEG), EEG remains the mainstay for the diagnoses and monitoring of epileptic activity. In this chapter, interictal and ictal EEG patterns for common types of epilepsies will be discussed.
EPILEPTIC ACTIVITY—GENERAL CONSIDERATIONS
Interictal Epileptiform Activity
Interictal epileptiform dischages (IED) can present as single spikes, sharp waves, or complexes that contain spikes and sharp waves that can last for up to a few seconds. In addition, IEDs can also present as intermittent rhythmic focal slowing such as temporal intermittent rhythmic delta activity (TIRDA) in adults or occipital intermittent rhythmic delta activity (OIRDA) in children.
Epileptic spikes are sharply contoured waveforms with lasting between 20 and 70 ms (Figure 12.1). Sharp waves, by contrast, are not as sharply contoured and last for 70 to 200 ms. The clinical importance of distinguishing between spikes and sharp waves is uncertain. Epileptic spikes and sharp waves are commonly surface negative due to the depolarization of the superficial laminae (1). They are episodic and should clearly stand out from the underlying background activity. Often they disrupt the underlying background activity and can have an aftergoing slow wave, to form a spike-and-wave complex. Spikes and sharp waves should also have a voltage field, which should make biological sense in regard to the underlying location of the cortical source. Analyzing the voltage field can help distinguish them from artifacts. It is also important to distinguish epileptiform activity from normal variants such as vertex waves, lambda waves, and wicket spikes.
Ictal Activity
Electrographic seizures or ictal patterns can be a longer-lasting epileptiform activity or an electrographic deviation from the baseline that shows an organized, rhythmic pattern and has evolved in terms of frequency, field or distribution, morphology, and amplitude.
EEG findings can be very useful in distinguishing between different epilepsies and remains integral part of syndromic classification. Ictal recordings can provide further data in characterizing and quantifying seizure types over the interictal findings. The ictal recording is also indispensable when considering surgical treatment for epilepsy.
EEG OF LOCALIZATION-RELATED EPILEPSIES
Localization-related epilepsies have several types of abnormal EEG findings, including focal IEDs and slowing. The type of seizure depends on the seizure-onset zone, though the clinical manifestations can be from the spread of ictal activity. It is important to recognize that occasionally the EEG can be normal in a focal seizure. The cortical region of synchronous activity needs to be at least 6 cm2 (1) and create changes on the surface of the cortex large enough to be picked up by scalp electrodes.
Benign Epilepsy With Centrotemporal Spikes
Benign epilepsy with centrotemporal spikes (BECTS), previously also referred to as benign rolandic epilepsy (BRE), has characteristic interictal EEG abnormalities. The background EEG is normal. Typical central-midtemporal spikes are seen with maximal voltage in the C3/4 electrodes and a field that extends to the T3/4 electrodes when viewed in a longitudinal bipolar montage. The spikes are stereotyped, diphasic (occasionally triphasic), and often have a horizontal anterior–posterior dipole with frontal positivity rather than a typical vertical dipole that is brain surface negative (Figure 12.2). They can occur singly or in runs, especially accentuated in light non-REM sleep. It can be easier to differentiate them from vertex waves by looking at them in transverse bipolar montage.
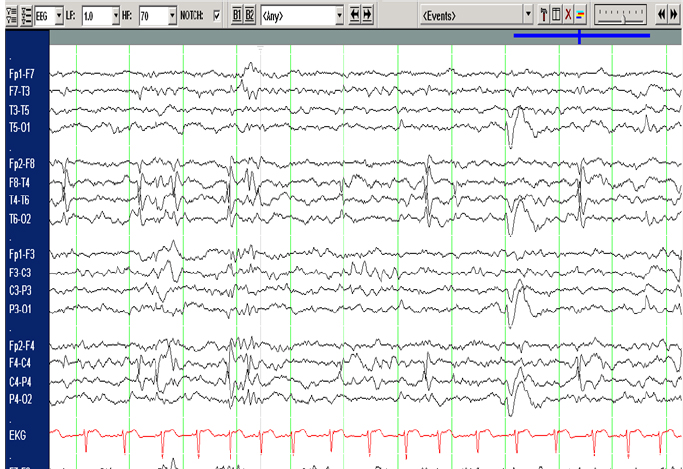
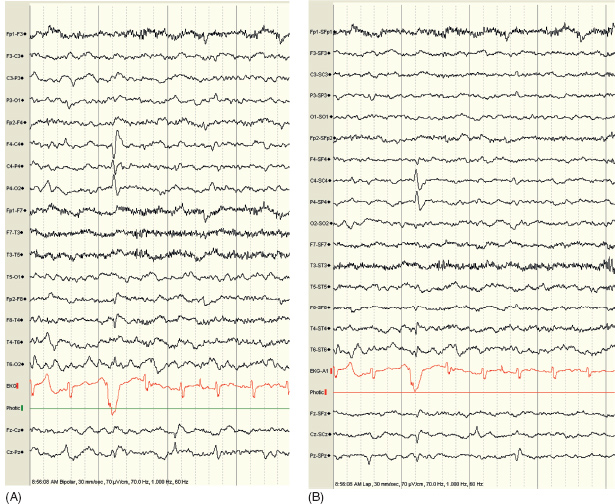
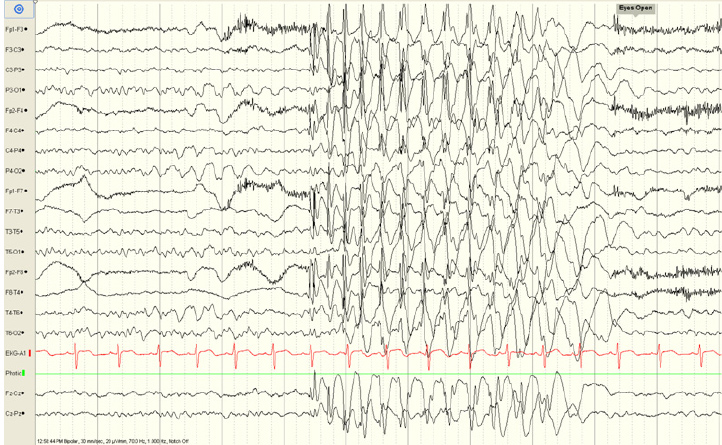
FIGURE 12.1 Interictal spikes as may be seen in localization-related epilepsy.
![]()
Temporal Lobe Epilepsy
Temporal lobe epilepsy is the most common form of localization-related epilepsies. Mesial temporal lobe onset accounts for majority of the temporal lobe seizures. Interictal EEG findings in mesial temporal lobe epilepsy (MTLE) show anterior temporal lobe discharges along with intermittent temporal slowing (Figure 12.3). Voltage of the IEDs is maximal in the sphenoidal or “true” anterior temporal electrodes (T1, T2) (2). Epileptiform discharges with maximum voltage in the lateral temporal leads can be seen, however, their predominance should raise the suspicion for a neocortical or extra mesial temporal generator (3). In approximately one-third of the patients, IEDs can be bilateral (2,4). TIRDA is seen only in minority of the patients, but when present, is highly associated with temporal lobe epilepsy (3).
The characteristic ictal EEG pattern of MTLE consists of unilateral 5- to 9-Hz rhythmic ictal theta or alpha epileptiform activity maximal in the anterior temporal scalp electrodes (3) (Figure 12.4). This pattern appears about 30 seconds after onset of clinical symptoms and signs (2). Postictal focal slowing or attenuation on the side of the seizure onset is more commonly seen in MTLE than with partial seizures originating outside the temporal lobe (2).
The EEG features of neocortical temporal lobe epilepsy tend to be more broadly distributed and less specific than those of MTLE. The IEDs are more likely to be lateral temporal, but these can be difficult to differentiate from MTLE IEDs (5). The ictal pattern is widely distributed in the hemisphere at onset and consists of an irregular, polymorphic rhythmic delta activity. Spread to contralateral hemisphere tends to develop earlier and more often than the MTLE (6) (Figures 12.5A and 12.5B).
Frontal Lobe Epilepsy
Frontal lobe epilepsies frequently lack lateralizing or localizing features on scalp EEG. Often, especially with mesial frontal lobe epilepsies, there is no electrographic correlate on the scalp electrodes (Figure 12.6). The IEDs, when present, can be bilateral synchronous, multifocal, or lateralized to the temporal lobe (7). Patients with mesial frontal lobe epilepsy can have rhythmic midline theta during wakefulness or bilateral frontal synchronous discharges (8). It is important to exclude periods of drowsiness and mental activation when evaluating rhythmic theta activity. Midline or frontocentral IEDs can be seen from electrodes Fz, Cz, F3, and F4 (9), but again need be to differentiated from sleep and drowsiness. IEDs from dorsolateral frontal cortex are more likely to be present and lateralized.
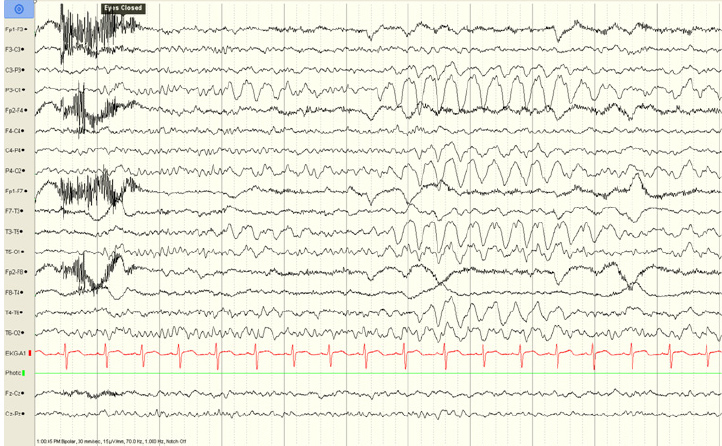
FIGURE 12.2 A central spike of benign epilepsy with centro temporal spikes (BECTS), (A) shows the spike in a longitudinal bipolar montage and (B) shows it in a Laplacian montage. Note the horizontal dipole with frontal positivity.
![]()

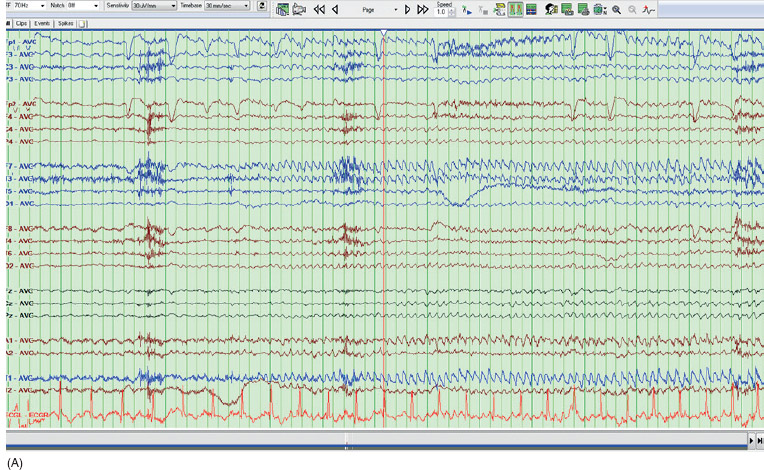
FIGURE 12.3 Left anterior temporal sharp waves and spike in an average reference montage.
![]()
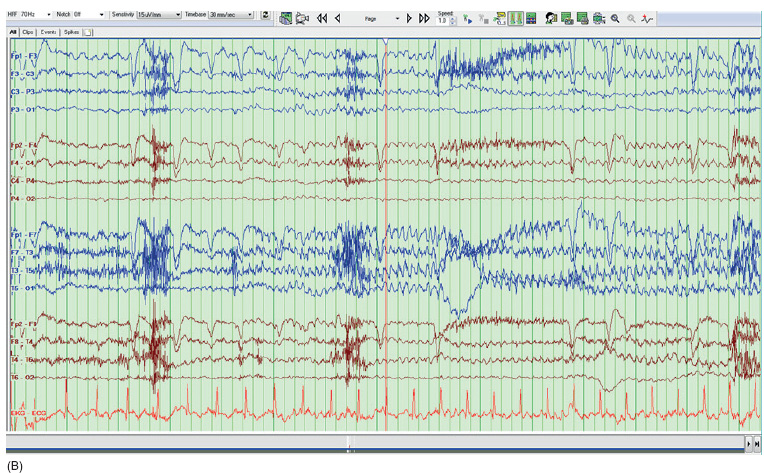
FIGURE 12.4 Rhythmic ictal theta in the left anterior temporal leads representing the onset of a temporal lobe seizure. (A) Demonstrates this in an average referential montage. (B) Shows the same seizure in a longitudinal bipolar montage.
![]()
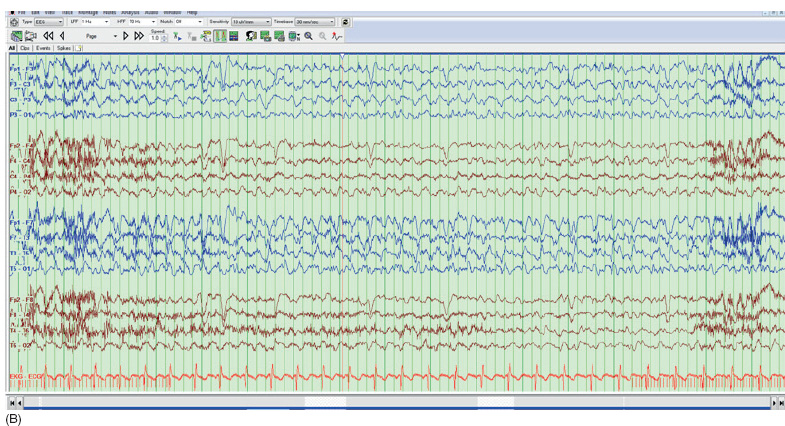
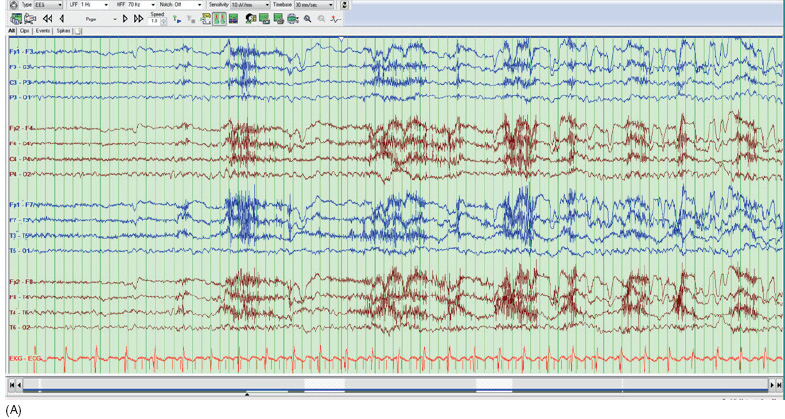
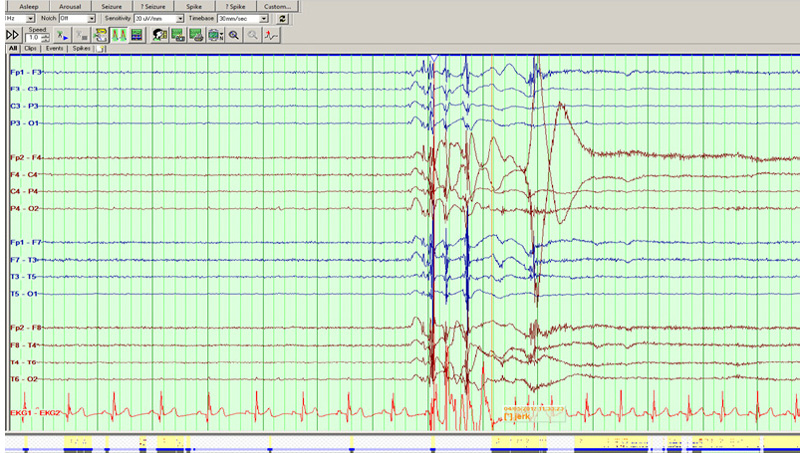
FIGURE 12.5 Left neocortical temporal seizure shown in a longitudinal bipolar montage. Notice the slower rhythmic activity over the temporal leads. The patient had lateral temporal focal cortical dysplasia.
![]()
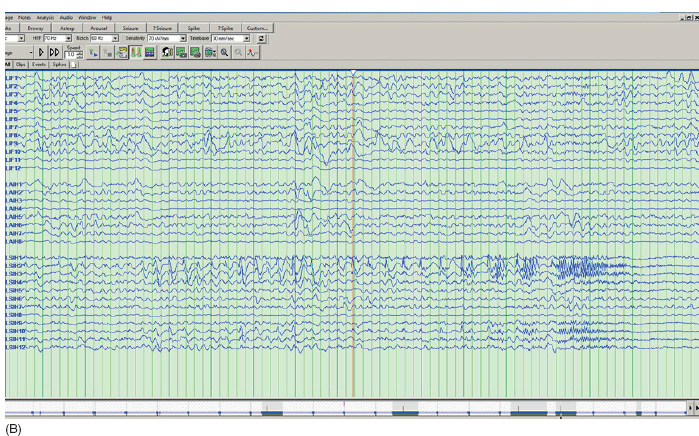
FIGURE 12.6 This is a mesial frontal lobe seizure. (A) Shows scalp EEG in a transverse bipolar montage that has no clear electrographic correlate except for possible subtle slowing in the left fronto-central leads. (B) Shows the same seizure with subdural electrodes showing spikes and seizure onset in the left inter-hemispheric subdural strip electrode (LSIH).
![]()
Parietal Lobe Epilepsy
Parietal lobe epilepsy is much less common than temporal or frontal lobe epilepsy. The conventional scalp EEG is of limited utility in these cases as the discharges are rarely localized. Interictal discharges can project to frontal or occipital head regions, causing false localization. Secondary bilateral synchrony of interictal discharges has been reported in more than 30% of patients undergoing surgery (11). Seizures are also rarely localized, though can be lateralized.
Occipital Lobe Epilepsy
Interictally, spontaneous or photic-induced occipital spikes are the main abnormalities in idiopathic occipital lobe epilepsy. However, it is important to keep in mind that occipital spikes can occur normally in 0.9% of preschool age children (12). Ipsilateral occipital slowing is more common than spikes in cryptogenic or symptomatic occipital lobe epilepsy. This can present as asymmetrical physiological rhythms such as alpha, lambda waves, photic driving, or positive occipital sharp transients of sleep.
Ictal manifestation is in the form of paroxysmal fast activity, fast spiking, or both, localized to the occipital regions with occasional gradual anterior spreading and generalization with spike–wave discharges (Figure 12.7).
EEG OF GENERALIZED EPILEPSIES
Childhood and Juvenile Absence Epilepsy
The classic EEG finding in childhood absence epilepsy is a generalized high-amplitude surface negative 3 Hz (range 2.5 to 5 Hz) spike and slow wave discharges (Figure 12.8). The discharges are most prominent in the frontal or frontocentral regions. Prominent OIRDA may also be present in children between the ages of 6 to 10 years (13). OIRDA is distinguished from normal slow waves of youth by its persistence, disruption of the alpha rhythm, and high voltage (Figure 12.9). Hyperventilation elicits discharges in 95% of patients. Photoparoxysmal response may also occur but is not as common. During sleep, spike wave complexes may appear polyphasic embedded within the normal sleep architecture.
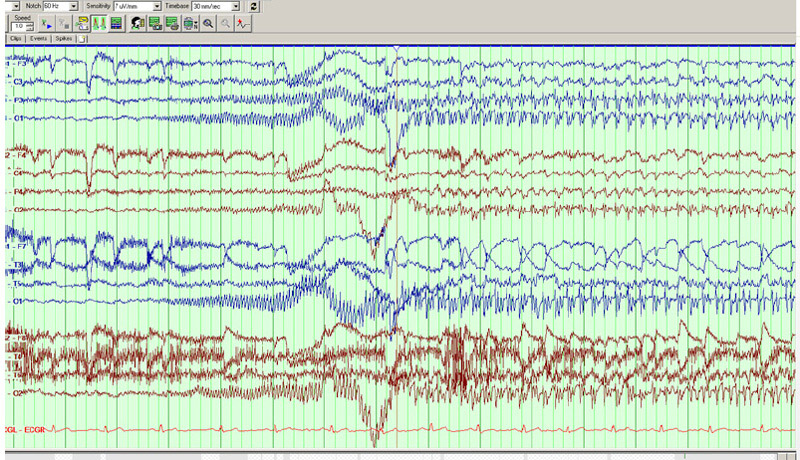
FIGURE 12.7 An occipital lobe seizure in a longitudinal bipolar montage.
![]()
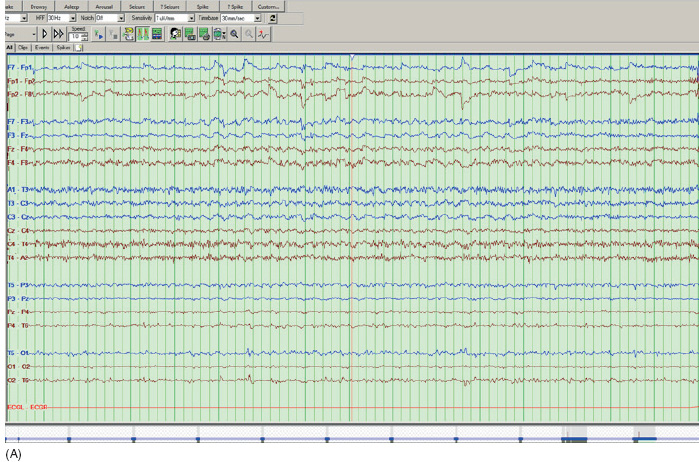
FIGURE 12.8 Interictal activity in patient with absence seizures showing the classic generalized 3 Hz spike wave discharge. The EEG is shown in a longitudinal bipolar montage.
![]()
Ictal discharges are similar to the interictal discharges, but prolonged, unless they cause generalized tonic–clonic seizure. The discharges are fastest in the first few seconds with a gradual slowdown as the activity terminates, followed by rapid return to normal background rhythm (Figure 12.10).
Juvenile absence epilepsy has similar interictal and ictal EEG findings as noted previously except polyspike wave discharges (PSW) are more commonly seen (13). OIRD activity is not usually seen in juvenile absence epilepsy.
Juvenile Myoclonic Epilepsy and Epilepsy With Generalized Tonic–Clonic Seizures Alone
EEG is highly sensitive for interictal discharges in patients with untreated juvenile myoclonic epilepsy (JME). It typically reveals a normal background with paroxysmal, generalized, bilaterally symmetric 4- to 6-Hz PSW discharges. The discharges like the generalized spike wave discharges of absence epilepsy are more prominent in the frontocentral region. Polyspikes may occur independently or in prolonged runs lasting up to a few seconds that can be followed by 2 to 5 Hz irregular high-amplitude slow waves with intermixed spikes. Photic stimulation can stimulate discharges in up to 40% of the patients (14). About half the patients have been shown to have focal or asymmetric generalized IEDs on prolonged recordings (15).
Ictally, myoclonic seizures are associated with polyspike or PSW bursts similar to the interictal discharges described earlier. Occasionally, the frequency of the multiple spikes seen is higher, about 10 to 16 Hz, with the discharges accompanied by a clinical jerk (2) (Figure 12.11). Generalized tonic–clonic seizures may be preceded by repetitive myoclonic jerks, resulting in a pattern known as clonic–tonic–clonic. The EEG during these seizures reveals 10- to 16-Hz spikes (corresponding with the myoclonus) followed by diffuse rhythmic fast activity (corresponding with the tonic phase), followed by rhythmic slow wave discharges (corresponding with the clonic phase) (Figure 12.12).
FIGURE 12.9 This EEG in a 6-year-old girl with frequent staring spells showing occipital intermittent rhythmic delta activity (OIRDA). The EEG is shown in a longitudinal bipolar montage.
![]()
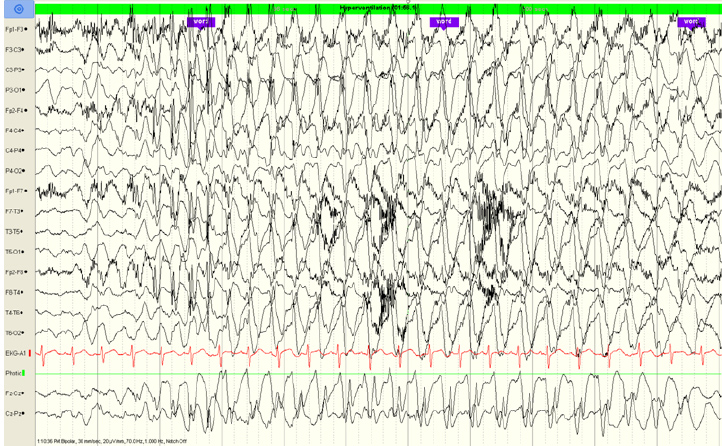
FIGURE 12.10 This is an EEG in the same patient as Figure 12.9. The patient stops hyperventilation and stares; the EEG shows a long run of a generalized 3 Hz spike wave discharge. The EEG is shown in a longitudinal bipolar montage.
![]()
FIGURE 12.11 EEG of a myoclonic jerk in a patient with JME. The EEG is shown in a longitudinal bipolar montage.
![]()
Lennox-Gastaut Syndrome
Lennox-Gastaut syndrome (LGS) is a severe epilepsy syndrome in which there are several types of seizures and cognitive impairment. The interictal EEG shows slowing of the background rhythms. IEDs are typically generalized “slow” spike wave discharges. The typical frequency of the spike wave discharges is less than 2.5 Hz, differentiating them from the discharges seen in absence epilepsy (Figure 12.13). At times, these IEDs can appear lateralized, but the lateralization can vary depending on the discharge.
There are several types of seizures that can occur with LGS. Tonic seizures typically manifest as an electrodecrement on the EEG. An electrodecrement consists of suppression of the background activity and appearance of generalized low-amplitude, fast-frequency activity (Figure 12.14). Atypical absence seizures show a long, generalized run of slow spike wave activity, similar to the IED. Drop, or atonic, seizures have similar slow spike wave activity.
West Syndrome
West syndrome is an epilepsy syndrome seen in young children, typically starting in the first year of life. The typical seizures are infantile spasms, and the interictal EEG shows a characteristic chaotic, high-amplitude EEG with multifocal spike and spike wave complexes. This pattern is known as hypsarrythmia (Figure 12.15). The EEG during the spasms resembles EEG of tonic seizures described earlier (electrodecrement).