History
The earliest recorded documentation of encephaloceles can be found in ancient sculptures and medieval art. These abnormalities were commonly depicted in individuals portrayed as demons and monsters. The earliest recorded descriptions can be credited to Forestus (1590).1 A century and a half later, Friderici (1737)2 published his findings of an autopsy performed on a stillborn with a severe form of Robert’s syndrome and associated anterior encephalocele. The first monograph on encephaloceles was written by Corvinus in 1749.3 The pathogenesis of nasal frontal encephaloceles has been a subject of debate and controversy over the years. Multiple theories have been proposed to explain the development of these congenital anomalies.
In the 19th century, Saint-Hillaire (1827)4 published a theory based on experimental work on chicken embryos. He proposed that adhesions resulting from intrauterine pressure caused a malformation known as hernie du cerveau (“hernia of the brain”) to form between the brain anlage and germinal membranes, which led to an arrest in the development of the anterior cranial vault. Herniation of the brain thus occurs through this pathologic opening (▶ Fig. 17.1).
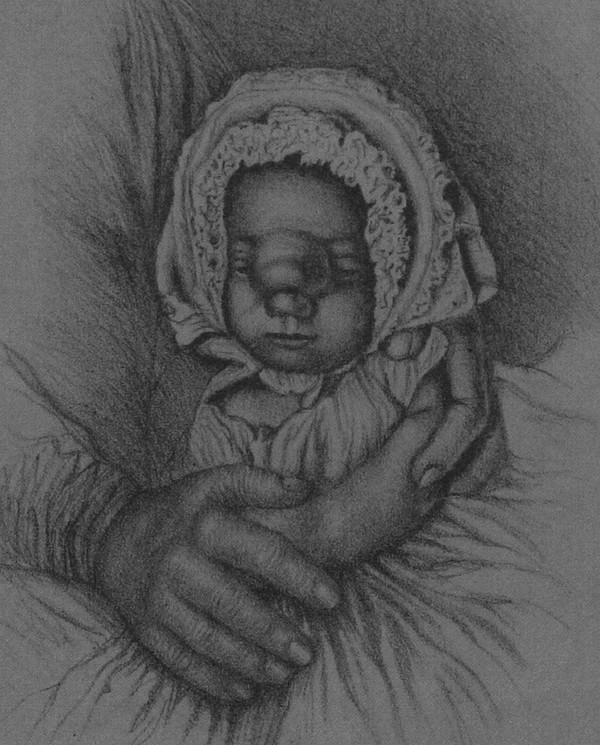
Fig. 17.1 Illustration of a clinical case showing an infant with a large nasofrontal encephalocele.
(From Hutchinson, 1875. Courtesy of Dr. James T. Goodrich.)
Several years later, Himly (1829)5 and Serres (1832)6 proposed that hernias formed through normally present bony channels, as opposed to a mild developmental formation through abnormal bony slits. In 1854, Spring7 hypothesized that encephaloceles arose as a consequence of various forms of ventricular dilation. In 1850, Rokitansky8 theorized that “congenital herniation of the brain was caused by an extreme increase in organ bulk.” In 1868, Klementowsky9 proposed that these congenital anomalies were secondary to bone-related pathologic processes such as cranial tabes, rickets, and syphilis. Ankermann10 in 1882 continued to attribute these lesions to hydrocephalic states. Schmidt11 in the 1900s blamed olfactory bulb remnants as the primary cause of encephaloceles (▶ Fig. 17.2a,b).
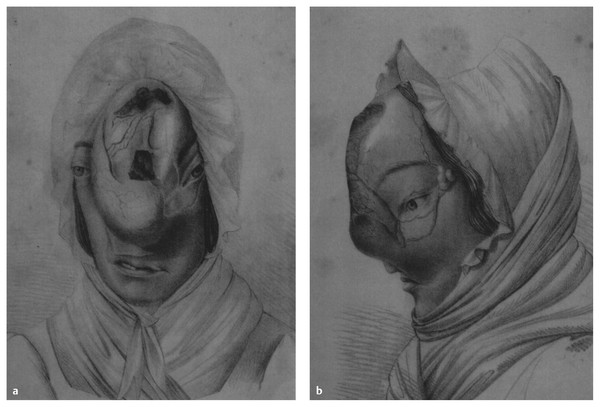
Fig. 17.2 (a) An adult with a frontal lesion consistent with a large sincipital encephalocele. (b) An adult with a frontal lesion consistent with a large sincipital encephalocele.
(From Chelius, 1831. Courtesy of Dr. James T. Goodrich.)
17.1.2 Classification
Several classification schemes have been proposed by multiple authors in the past, leading to confusion in the nosologic categorization of the lesions.12–17 A currently well-accepted classification is based on the anatomical location of the skull defect.18 Primary encephaloceles are those lesions that either are present at birth or have a congenital substrate. Secondary encephaloceles are acquired lesions that are most commonly the result of trauma or surgery.
Primary encephaloceles are divided into three major types: cranial vault, frontoethmoidal, and basal. Cranial vault encephaloceles can occur anywhere in the skull, and in North America they most commonly present in the occipital region (see box “▶ Classification of Encephaloceles”). Atretic encephaloceles are forme fruste encephaloceles; they characteristically present as small, noncystic nodular or flat lesions located in the midline near the vertex (parietal type) or anterior to the inion (occipital type) (▶ Fig. 17.3, ▶ Fig. 17.4a,b). The overall incidence of encephaloceles is approximately 0.8 to 3.0 per 10,000 live births,19–22 and when compared with their spinal counterparts, encephaloceles account for approximately 10 to 20% of all cases of craniospinal dysraphism. Encephaloceles comprise approximately 10 to 15% of all neural tube defects.
Classification of Encephaloceles
Primary
Cranial vault
Occipital
Cervico-occipital
Interparietal
Temporal
Interfrontal
Anterior fontanel
Posterior fontanel
Frontoethmoidal (sincipital)
Nasofrontal
Nasoethmoidal
Naso-orbital
Basal
Transethmoidal
Transsphenoidal
Sphenoethmoidal
Sphenomaxillary
Spheno-orbital
Sphenopharyngeal
Temporal
Posteroinferior (endaural)
Anteroinferior
Cranioschisis
Acrania: exencephaly
Cranial: upper facial cleft
Basal: lower facial cleft
Secondary
Traumatic
Postsurgical
Inflammatory
Neoplastic

Fig. 17.3 Newborn male with a small, pulsating bony defect and an abnormally colored scalp. A small amount of cerebral tissue herniates through the opening.
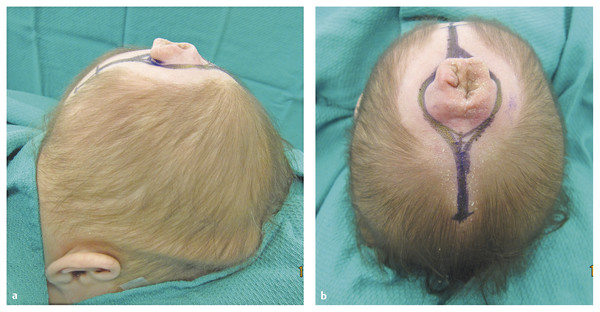
Fig. 17.4 (a) Lateral view of a child with an atretic encephalocele. A small cranial defect allowed passage of a gliotic tract associated with abnormally developed skin. (b) Scalp marks for proposed incision to resect an atretic encephalocele. No spinal fluid is associated with this lesion, which was fully resected with excellent long-term effects.
17.1.3 Epidemiology
The incidence of encephaloceles varies worldwide with geographic location and race.23 Occipital encephaloceles are the most common type in North America and western Europe, with an incidence varying between 1 in 3,000 to 1 in 10,000 live births; they comprise ~85% of all encephaloceles.24–26 Seventy percent of occipital encephaloceles occur in females, and 15 to 20% are found in association with neural tube defects.27,28 In contrast, anterior encephaloceles occur with greater frequency (1 in 3,500 to 1 in 5,000 live births) in Southeast Asia (Thailand, Indonesia, Burma, Philippines, Malaysia), parts of Russia, and central Africa.23–33 The incidence of anterior encephaloceles in North America is estimated to be 1 in 35,000 live births. Basal encephaloceles are much less common and comprise fewer than 10% of encephaloceles.34 Temporal encephaloceles are extremely rare malformations and are thought to comprise fewer than 1% of cerebrospinal malformations.35–37 The true incidence of encephaloceles secondary to trauma or surgery is not known.
17.1.4 Associated Anomalies
An encephalocele may present as a single isolated congenital anomaly or in association with other anomalies to comprise a syndrome or association (▶ Table 17.1).28 Encephaloceles are most commonly associated with Meckel syndrome and amniotic band syndrome.38 Meckel syndrome consists of occipital encephaloceles, polydactyly, polycystic kidneys, holoprosencephaly, micro-ophthalmia, retinal dysplasia, cardiac anomalies, orofacial clefts, and other anomalies. Occipital encephaloceles were found to occur in 39 of the 49 cases tabulated by Mecke and Passarge.39
| Syndromes | Prominent Features | Etiology |
| Occipital encephaloceles | ||
| Meckel syndrome | Polydactyly, polycystic kidneys, holoprosencephaly, micro-ophthalmia, retinal dysplasia, cardiac anomalies, orofacial clefts, ambiguous external genitalia, other abnormalities | Autosomal-recessive |
| Pseudo-Meckel syndrome | Arrhinencephaly, absent corpus callosum, Arnold-Chiari defect, no evidence of retinal dysplasia, cleft palate, congenital heart defects, accessory spleen, clubfoot, hallucal hammertoes | t(3p+) |
| Chemke syndrome | Hydrocephaly, agyria, absent cortical laminar structure, cerebellar dysgenesis, retinal dysplasia, corneal opacities, cataracts | Autosomal-recessive |
| Cryptophthalmos syndrome | Extension of forehead skin to cover one or both eyes, unusual hairline, ear anomalies, notching of the nasal wings, soft tissue syndactyly of hands and/or feet, genital anomalies | Autosomal-recessive |
| Knobloch syndrome | High myopia, vitreoretinal degeneration, retinal detachment, meningocele, normal intelligence | Autosomal-recessive (presumed) |
| von Voss syndrome | Aplasia of the corpus callosum, hypoplastic olives and pyramids of the medulla oblongata, phocomelia, urogenital anomalies, thrombocytopenia | |
| Warfarin syndrome | Nasal hypoplasia, bone stippling, limb shortening, low birth weight, optic atrophy, mental retardation, seizures, hydrocephaly | Warfarin during pregnancy |
| Frontal encephaloceles | ||
Frontonasal dysplasia | Ocular hypertelorism, widow’s peak, anterior cranium bifidum occultum, widely set nostrils with lack of elevation of the nasal tip, notching of nostrils, other abnormalities | Most cases sporadic, some familial, probably etiologically heterogeneous |
| Amniotic band syndrome | Ring constrictions and amputations of digits or limbs, distal syndactyly, irregular or asymmetric encephaloceles, microcephaly, micro-ophthalmia, bizarre orofacial clefts, other facial disruptions, tissue bands, various other anomalies | Aberrant tissue bands |
| Source: Adapted from Cohen MM, Lemire RJ. Syndromes with cephaloceles. Teratology 1982;25:161–712.38 | ||
Amniotic band syndrome occurs because of amniotic tissue bands that form in utero and lead to the constriction of fetal parts and disruption of normal development (▶ Fig. 17.5). Most commonly affecting limbs or digits, these bands can become directly attached to the cranium or face, producing “nonanatomical” encephaloceles. The lesions are unusual because they have irregular surfaces, are asymmetrically placed with respect to the midsagittal plane, and have multiple sites of involvement (▶ Fig. 17.6, ▶ Fig. 17.7, ▶ Fig. 17.8, ▶ Fig. 17.9). Chemke syndrome is characterized by occipital encephaloceles, hydrocephalus, agyria, retinal dysplasia, corneal opacities, and cataracts.40 Cryptophthalmos syndrome involves extension of the forehead skin to cover one or both eyes, unusual hairline, ear abnormalities, notching of the nasal wings, soft tissue syndactyly of hands and feet, genital anomalies, and a 10% incidence of occipital encephaloceles. It is inherited as an autosomal-recessive trait. Knobloch syndrome presents with myopia, vitreoretinal degeneration, retinal detachment, and occipital meningoceles.41 von Voss syndrome involves aplasia of the corpus callosum, hypoplastic olives and pyramids of the medulla, phocomelia, urogenital anomalies, thrombocytopenia, and occipital encephaloceles. Warfarin syndrome has been associated with the ingestion of warfarin during pregnancy. It presents with nasal hypoplasia, bone stippling, limb shortening, low birth weight, optic atrophy, mental retardation, seizures, hydrocephalus, and occasionally occipital encephaloceles.

Fig. 17.5 T1-weighted gadolinium-enhanced coronal magnetic resonance image shows herniating cerebral tissue with a large meningocele and large vascular channels secondary to amniotic bands in utero.

Fig. 17.6 A newborn girl with a large parietal encephalocele secondary to amniotic band syndrome. Eccentrically located lobulated mass was associated with cleft lip and palate and with amputated feet and digits.

Fig. 17.7 Lateral view of a patient with a large paramedian encephalocele. Although most of the lesion was covered with skin, the distal end leaked cerebrospinal fluid and had a thin neovascularized membrane.

Fig. 17.8 Ten-month-old boy with a large right parietal encephalocele and amniotic band syndrome. Note results of the bands: damage to ear and eyelids, cleft lip and palate.

Fig. 17.9 Highly disorganized encephalocele secondary to amniotic bands.
Associated anomalies (see box “▶ Associated Anomalies Seen in Patients with Encephaloceles”) include absence of the corpus callosum, optic nerve abnormalities, cleft lip, cleft palate, Tessier facial clefts, craniosynostosis, Dandy-Walker cyst, Chiari malformations, ectrodactyly, hemifacial microsomia, hypertelorism, Klippel-Feil anomalies, myelomeningoceles, and anophthalmia.38 Hydrocephalus is relatively common in patients with occipital encephaloceles, and the incidence may be as high as 65% (▶ Fig. 17.7).42 In contrast, hydrocephalus is seldom seen in patients with nasofrontal encephaloceles.
Associated Anomalies Seen in Patients with Encephaloceles
Tessier facial cleft
Craniostenosis
Dandy-Walker cysts
Chiari malformations
Ectrodactyly
Hemifacial microsomia
Hypothalamic–pituitary dysfunction
Iniencephaly
Klippel-Feil syndrome
Myelomeningocele
Hypertelorism
Optic nerve abnormalities
Holoprosencephaly
17.1.5 Occipital Encephaloceles
The etiology of occipital encephaloceles is not well understood, but these anomalies have been correlated with maternal low-fibrate levels and the use of vitamin A and sodium arsenate. In North America, occipital encephaloceles are the most common type seen clinically and account for approximately 80% of these lesions. The diagnosis is now commonly made with routine prenatal ultrasonography, which helps guide the treatment plan. Given the common association of multiple intracranial anomalies, complete examination of the patient’s cranial vault and cervical spine should be undertaken with magnetic resonance (MR) imaging. Although the diagnosis of occipital encephalocele is usually obvious at birth, subtle brain herniations may require a high level of suspicion. Occipital encephaloceles can be located high in the occipital squama or lower at the level of the foramen magnum level; they may even involve the upper cervical spinal levels.
Clinical Presentation
The presence of an occipital encephalocele is obvious at the time of birth, and many of these lesions are now being diagnosed in utero with ultrasonography. Vaginal delivery may be possible with relatively small lesions, whereas larger encephaloceles may necessitate cesarean section. The clinical presentation may vary significantly, depending on the size and contents of the lesion. Infants who have small encephaloceles with little or no herniating brain may act normally, with adequate breathing and normal neurologic examinations. Almost all lesions are fully covered with skin and can be electively repaired. Larger masses may be associated with neurologic deficits: cranial nerve abnormalities, poor sucking and feeding, spasticity, blindness, and developmental delay. Patients may present with large sacs and microcrania. Associated neural tube defects may be seen in 15 to 20% of the patients.16 Reported associated congenital malformations include hypoplastic left cranium, bilateral clinodactyly, web neck and micrognathia, thyroglossal cyst, and external annular dermoids.42
Pathology
Encephaloceles are believed to result from the failure of separation of the surface ectoderm from the neuroectodermal elements. The result is a bony defect in the skull that permits herniation of neural elements as well as CSF. The pathology of these lesions directly correlates with their site and location. Small lesions, located in the subtorcular area, may have only CSF and gliotic nonfunctional tissue. Larger masses with bony defects involving the entire occiput and upper cervical levels may have massive infra- and supratentorial brain herniation. The sites of encephaloceles vary significantly. They are often large: larger than 20 cm (16%), 15 to 20 cm (14%), 10 to 15 cm (12%), 5 to 10 cm (30%), and smaller than 5 cm (28%).42 The occurrence of associated hydrocephalus varies with published series: 16%,42 36%,25 50%,43 and 65%.44 The skull base may be deformed, and microcephaly has been reported in from 9 to 27% of cases.20 The falx and tentorium are often in an abnormal anatomical position. Bony defects may also vary in size and extent; they may involve just the occipital bone or may include the posterior elements of adjacent vertebrae and even extend superiorly, above the inion. The contents of the sac may be extremely variable. Simpson et al reported that 32% of the patients‘ lesions contained recognizable cortex, 11% contained cerebellum and fourth ventricular structures, and 20% contained glial nodules. The brainstem may be partially or completely herniated. Thalami were found in 20% of the cases.28 Postmortem examinations24,27 have revealed multiple abnormalities, including a small posterior fossa, hypoplastic falx and tentorium, and asymmetric herniation of the cerebral hemispheres ranging from an occipital pole to an entire hemisphere (see box “▶ Associated Findings in Patients with Occipital Encephaloceles”). The intracranial contents tend to shift posterocaudally, leading to frontal lobes occupying variable portions of the middle fossa and temporal lobes partially displaced into the posterior fossa (▶ Fig. 17.10a,b). Notable distention of the ventricular system, optic pathways, corpus callosum, and hypothalamus has been noted. The posterior fossa shows the most remarkable anomalies, with marked brainstem distortion that is often seen as an s-shaped kink (▶ Fig. 17.11). The cerebellum may be rudimentary and associated with cleftlike fissures extending into the dorsal brain stem from the fourth ventricle. The “inverse cerebellum” described by Padget45 shows ventral protrusion of the cerebellar hemispheres to envelop the anterior lateral aspects of the brainstem, with vermian agenesis or hypoplasia and brainstem kinking. The fourth ventricular roof opens into the sac, leading to a “fourth ventriculocele.”
Associated Findings in Patients with Occipital Encephaloceles
Brainstem kinking
Inversion of the cerebellum
Temporal lobe herniation
Occipital lobe herniation
Dysgenesis of the cecum
Dysgenesis of the vermis
Corpus callosum dysplasia
Thalami fusion
Hydromyelia
Hydrocephalus
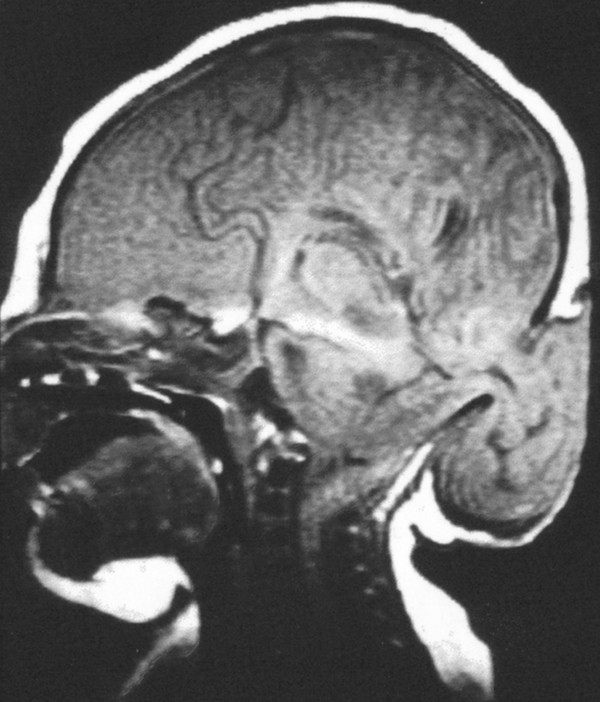
Fig. 17.10 Sagittal magnetic resonance image demonstrates a large amount of herniating cerebellar tissue, along with occipital lobe, through a small cranial defect. Coronal magnetic resonance image showing a large meningocele associated with the encephalocele in.
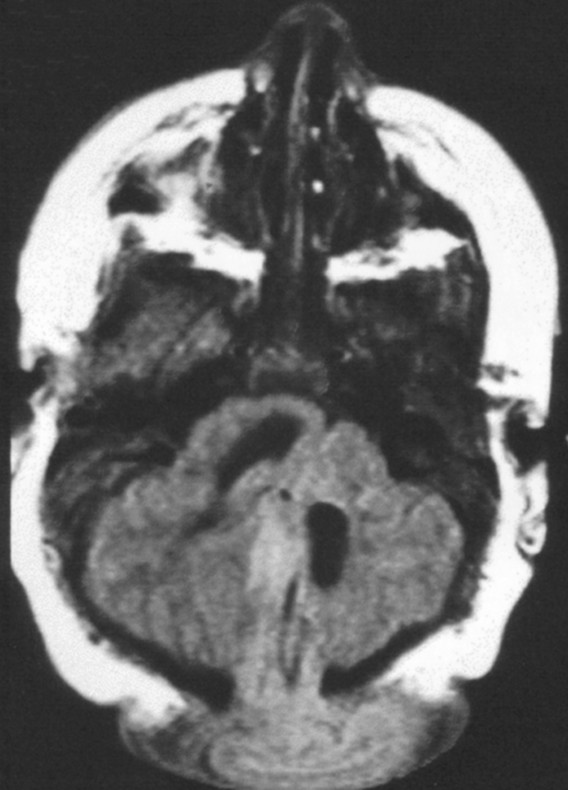
Fig. 17.11 Axial T2-weighted magnetic resonance image of a patient with an occipital encephalocele shows marked dysplasia of the posterior fossa contents.
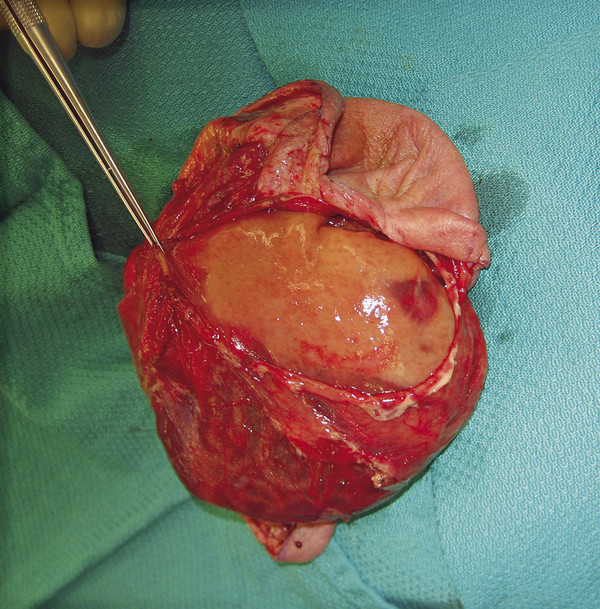
Fig. 17.12 Occipital encephaloceles can present with large amounts of herniated abnormal cerebral tissue. This intraoperative photograph show an infant with such a lesion and a cortex without a gyral–sulcal pattern.
Prognostic Factors and Outcomes
The prognosis and long-term outcome for patients born with occipital encephalomeningoceles are directly proportioned to the amount of neural tissue found in the sac and the severity of the associated neural anomalies. The infant who has only CSF or small nodules of dysplastic neural tissue in the sac has a relatively good chance of attaining normal or nearly normal neurologic and physical development. Patients with few anomalies and a small amount of neural herniation will have approximately a 53% chance of being physically and mentally normal, a 28% chance of normal intelligence but physical impairment, and a 19% chance of mental retardation.22 Conversely, the greater the neural involvement and number of associated neural abnormalities, the greater the rate of mental retardation and poor outcomes. When all patients with occipital encephaloceles are considered, approximately 17% will be normal and 83% will be significantly mentally and physically impaired.22 The appropriate treatment of hydrocephalus plays an important role in the long-term outcome of these patients.66
Surgical Treatment
Unless the sac has ruptured and there is concurrent leakage of CSF, surgical repair may be done electively (▶ Fig. 17.13). The patient is placed prone on an appropriately padded cerebellar horseshoe headrest (▶ Fig. 17.14a). A single dose of an antibiotic (first-generation cephalosporin) is given before induction. The occipital and upper cervical areas are prepared and draped, with application of povidone–iodine solution. If a large sac is present, it may be elevated with grasping forceps by an assistant to allow complete skin preparation. Using a very low-level (15-W) monopolar electrocautery, the surgeon creates a plane of dissection between the junction of “normal” skin and epithelialized skin. This plane is carefully followed circumferentially and toward the neck of the encephalocele (▶ Fig. 17.14b,c). A transverse incision is extended to expose the underlying bone and bony defect. A dissection plane is developed between the dura and the skin. Entrance into the dome of the sac will allow CSF to drain and the contents of the sac to be explored. At this point, careful examination of the encephalocele should help guide the surgeon on the proper surgical approach. If the herniating mass is deemed to be composed of fibrous, gliotic, nonfunctional tissue, a decision to transect the mass flush with the skull can be safely made. Some authors have advocated “expansion cranioplasties” to accommodate large amounts of herniated neural tissue. If the herniated tissue is deemed “viable” or resembles normal cerebral architecture, it should be saved, and the expansion cranioplasty technique should be employed. Barrel stave osteotomies can be created with a drill and expanded outward. The open end of the encephalocele can then be covered with full-thickness calvarial grafts from the surrounding parietal bones (▶ Fig. 17.15a–c). This maneuver will provide complete osseous coverage of the encephalocele area. However, it should be done only in young infants who are fully capable of regenerating new calvarial bone at the donor site. Another technique uses tantalum mesh to create an extracranial compartment to enclose the neural elements.46 The mesh is attached to the periphery of the skull defect. As the intracranial pressure increases, the calvaria is forced to expand, and the mesh is gradually imbricated with the skull by daily digital compression. Another approach is simply to close soft tissues over the neural mass and perform a revision as a second stage.43 A ventricular volume reduction technique has been proposed by Oi et al47 to deal with this problem. Using the associated hydrocephalic state, they do a first-stage procedure that involves closing the encephalocele defect with a dural patch graft. The repaired dura allows the intraventricular pulse pressure to produce ventriculomegaly. Once hydrocephalus develops, a ventriculoperitoneal shunt is placed to allow transposition of the herniated brain into an enlarged intracranial cavity.48 However, despite attempts at preserving neural tissue by these techniques, profound morbidity continues to be associated with large occipital encephaloceles.

Fig. 17.13 Newborn female infant with a very large occipital encephalomeningocele.

Fig. 17.14 (a) The patient is placed prone in a padded cerebellar horseshoe headrest. Care must be taken not to allow the encephalocele to move inadvertently and cause torsion of the cerebral contents of the posterior fossa. (b) A plane of dissection is developed between the scalp and the encephalocele. A vascular scalp is often seen, and care must be taken not to violate the galea and cause significant blood loss. (c) Successful resection of the encephalomeningocele of the patient in ▶ Fig. 17.13.
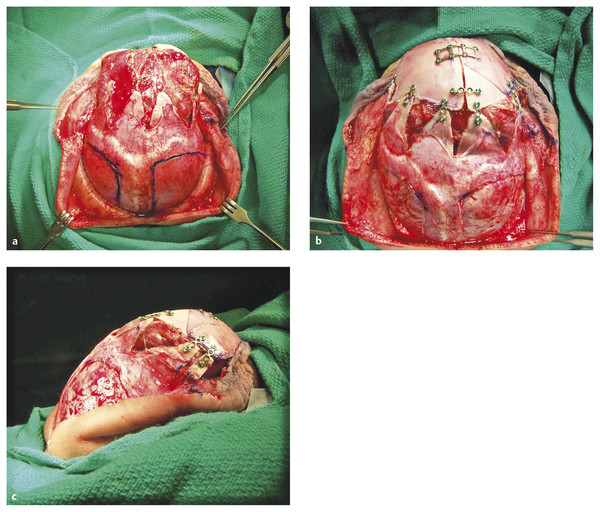
Fig. 17.15 (a) Scalp has been reflected to show the area below the lambdoid and sagittal sutures. The occipital bone was cut radially to create wedge osteotomies and accept herniated cerebral tissue. (b) Bilateral full-thickness calvarial grafts have been harvested and secured to the surrounding expanded occipital bone with titanium miniplates. (c) Lateral view demonstrates complete bony coverage of the occipital encephalocele. The donor site fully reossifies over the ensuing months.
If the skull defect is small (pedunculated encephalocele), no specific management of the bone defect is necessary. Whenever large calvarial defects are present, a simple way to manage them is to extend the skin opening into adjacent parietal regions. A full-thickness craniotomy fitting the shape of the skull defect may be harvested and transposed. The donor site contains osteogenic dura that will ossify and create new bone within 2 to 6 months (▶ Fig. 17.16a–f). Another acceptable method for dealing with large calvarial defects is to close the encephalocele first, and then later (when the child is about 2 years old) proceed to an autologous cranioplasty with a split-thickness calvarial graft. Hydroxyapatite bone cement (Bone Source; Howmedica Leibinger, Dallas, TX) is commercially available for the closure of cranial defects up to 25 cm.13 The cement is composed of tetracalcium phosphate and dicalcium phosphate powder reactants that, when mixed with water, lead to the isothermic formation of a solid implant composed of carbonated hydroxyapatite. This compound has been used successfully to reconstruct posterior fossa calvarial defects68 and perhaps should be considered for reconstructing small encephalocele defects in selected patients. Yet another method for closing a skull defect associated with an encephalocele involves the use of HTR-PMI, which is a combination of PMMA (poly-methylmethacrylate) and PHEMA (poly-hydroxyethylmethacrylate) and has a rigidity similar to that of bone (W. Lorenz Surgical, Jacksonville, FL). A proprietary computed tomographic (CT) scan protocol is used to produce a custom-fitting implant.
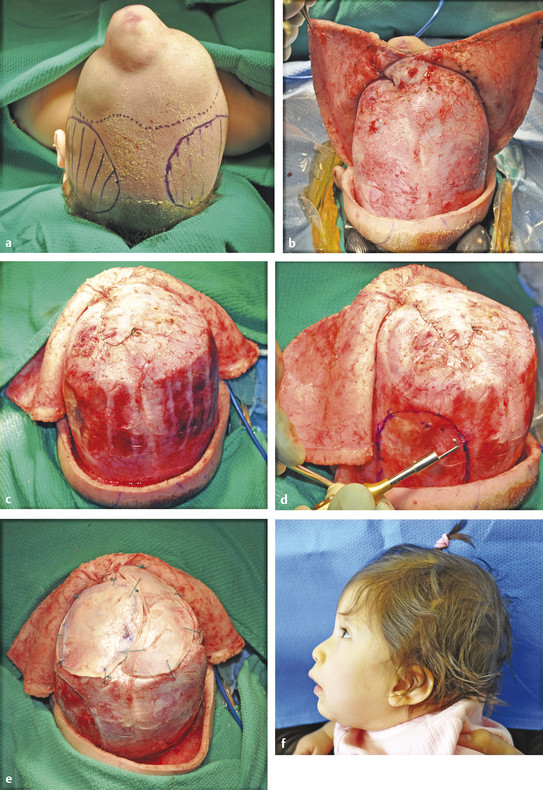
Fig. 17.16 (a) Top view of patient with a large encephalocele of the occipital area. The dotted line demarcates the edge of the bony defect surrounding the encephalocele. The rounded (solid lines) parietal areas indicate the donor site of the parietal bones. (b) A bicoronal scalp incision that is a “T” toward the encephalocele is needed to provide a large area of exposure for encephalocele repair and bone harvesting and reconstruction. (c) Following complete encephalocele repair and dural closure, a large calvarial defect is noticed over the occipital area. (d) The donor site over the right parietal area is prepared. A very small bony opening is made large enough to fit the foot attachment of the drill. The solid line demarcates the osteotomy line. (e) The full-thickness calvarial grafts have been secured to the surrounding bone with nonabsorbable Ethibond (Ethicon, Somerville, NJ) sutures. (f) A lateral photograph of the patient 1 year after closure shows an excellent result with full ossification of the donor and recipient sites.
17.1.6 Anterior Cranial Fossa Encephaloceles
Various classifications have been proposed for categorizing encephaloceles located in the anterior cranial fossa. Sincipital encephaloceles are those lesions that are associated with the skull defect at the foramen cecum, anterior to the cribriform plate. Suwanwela and Suwanwela proposed the most useful and widely accepted classification of sincipital encephaloceles in 1972.18 They classified these lesions as nasofrontal, nasoethmoidal, naso-orbital, and interfrontal encephaloceles. Basal encephaloceles are those lesions that protrude through the floor of the anterior cranial fossa (cribriform plate, planum sphenoidale). These lesions have been classified as sphenopharyngeal, spheno-orbital, sphenomaxillary, and sphenoethmoidal.
Pathology
The pathogenesis of frontal encephaloceles is not known. Currently, two schools of thought exist regarding the origin of these lesions. The first concept involves the point of weakness in the facial skeleton. The frontal bone is a membranous bone that forms from the underlying dura, whereas the ethmoid bone develops during endochondral bone formation. The function of the membranous and endochondral bone (foramen cecum is thought to result in a weak area through which the neural elements can herniate).43,44 A second hypothesis states that a delayed closure of the neural tube ultimately prevents normal union of the facial bones.45 Findings of a trapped meningocele and peripheral nerve elements, as well as isolated neural tissue remnants along the original tract, appear to substantiate the second theory. However, the fact that most anterior encephaloceles are covered with normal skin indicates that these defects are not simply a failure of neurulation. Thus, their precise etiology remains speculative. On histologic examination, the herniated tissue can vary between normal brain to fibrous atrophic nonviable tissue.46 In the majority of cases, however, the herniating mass of a nasofrontal encephalocele consists of gliotic, nonfunctional neural tissue.21,31
In contrast, occipital encephaloceles contain a much wider variety of tissue types. Simpson20 reported that 32% of patients had recognizable cerebral cortex within the sac, 11% had cerebellum and fourth ventricle, and 20% had glial nodules. Oi et al47 reported temporal lobe herniation, occipital lobe herniation, dysgenesis of the tectum, dysgenesis of the vermis, corpus callosum dysplasia, thalami fusion, brainstem kinking, and cerebellar inversion as findings associated with occipital encephaloceles. Other authors have reported the presence of supratentorial cortex with or without herniation, cerebellar tissue, and fourth ventricular tissue (see box “▶ Associated Findings in Patients with Occipital Encephaloceles”). Disorganized fibrous and vascular tissue was also commonly found in many patients with occipital encephaloceles.24,27,48
17.1.7 Sincipital Encephaloceles
Clinical Presentation
The clinical presentation of a sincipital encephalocele can range from an occult, nondiscernible lesion to marked craniofacial deformity (see Box ▶ Signs and Symptoms of Sincipital Encephaloceles). A sincipital encephalocele may vary in size from a barely noticeable mass to a lesion larger than the patient’s head.
Signs and Symptoms of Sincipital Encephaloceles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








