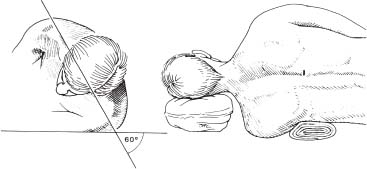
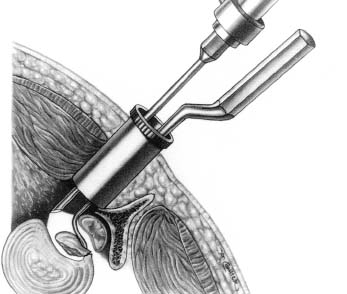
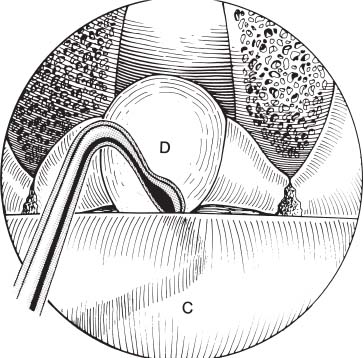
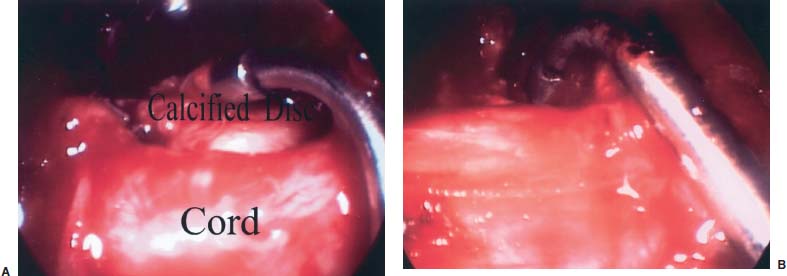
Minimalism for the surgical treatment of thoracic disk herniation has several surgical goals: cure or resolution of symptoms, minimal disruption of biointegrity, minimal risk from the surgical procedure itself, minimal chance of postoperative complications, rapid surgical recovery, and cost effectiveness. Regardless of the anatomical approach, surgical treatment must provide high rates of symptomatic resolution with low risks of intraoperative complications. Surgical results among the various posterolateral approaches have been comparable. As for surgical risks, spinal cord damage has been the most serious potential risk in thoracic disk surgery. Postoperative paraplegia was not uncommon when thoracic disk herniation was treated with the midline posterior laminectomy technique.1 Surgical treatment for thoracic disk herniation via the posterior approach has gradually shifted from the traditional midline laminectomy to such posterolateral approaches as costotransversectomy, lateral extracavitary, and a transpedicular approach in an attempt to avoid catastrophic spinal cord injury.2–9 The posterior surgical approaches have extended further laterally to provide a maximum ventral view of the spinal cord, which has significantly reduced the risk of intraoperative spinal cord damage; however, posterolateral surgical approaches often necessitate extensive surgical incision and tissue dissection. The least invasive among the various posterior approaches is the transpedicular approach, but because this approach is usually paramedian rather than posterolateral, the ventral aspect of the spinal cord is not directly visualized during surgical decompression. The transthoracic approach was also developed to avoid intraoperative spinal cord damage. Although the main advantage of this thoracotomy approach is direct access to the anterior aspect of the spinal cord, the thoracotomy procedure itself involves an extensive surgical incision and entrance into the pleural cavity. An endoscopic transthoracic approach has been developed to minimize invasiveness of the conventional thoracotomy technique10; however, this endoscopic transthoracic technique still necessitates three to four separate skin incisions in the chest wall and often requires postoperative chest tube drainage. The depth of the surgical tract is also very long, thus maneuvering such delicate surgical tools as a power drill can be challenging. In an attempt to achieve the ideal surgical goals of minimalism for thoracic disk herniation, an endoscopic transpedicular approach was adopted. The transpedicular approach involves a relatively small skin incision and minimal tissue dissection. The required skin incision is 1.5 to 2 cm in length when an endoscope is adopted. The medial portion of the facet joint and rostral-medial one-third portion of the pedicle are removed to access the protruded disk under a 0-degree-lens endoscope. A 4 mm diameter rigid endoscope with a 70-degree lens is then mounted to a custom-made endoscope holder. The use of a 70-degree lens enables the surgeon to visualize the ventral aspect of the spinal cord directly.3 Under this steady image provided by the mounted endoscope, decompression of the ventral spinal cord is executed utilizing 90-degree-curved surgical instruments. The invasiveness of this transpedicular thoracic diskectomy becomes quite comparable to that of cervical or lumbar microdiskectomy.4 In this chapter, the details of endoscopic transpedicular thoracic diskectomy will be described. Surgical Indications and Preoperative Tests Surgical indications for endoscopic transpedicular thoracic diskectomy are as follows: Clinical symptoms of thoracic disk herniation can be divided into these three groups. The first group of symptoms can be considered thoracic spine symptoms due to local disruption of the anatomy. Thoracic spine symptoms may include midline thoracic pain, paramedian thoracic pain, and retrosternal pain. Because cervical spine pathology can also produce scapular or interscapular pain, upper thoracic disk herniation may mimic symptoms related to cervical disk disease. The second group of symptoms is radiculopathy related to compression of the nerve root or ganglion. The resulting focal muscle weakness can produce protrusion of the abdomen. The third group of symptoms is myelopathy caused by spinal cord compression. Surgical treatment is indicated in patients with myelopathy or radiculopathy unresponsive to trials of medical treatment; however, the sole presence of midline paramedian thoracic pain related to local disruption of the anatomy does not respond well to surgical treatment. Patients without radiculopathy or myelopathy must be fully aware that surgery may fail to relieve their thoracic pain. In addition to the clinical evaluation of symptoms, high-resolution MRI scans should be the diagnostic choice, although CT with myelography is still occasionally used (Fig. 12–1). As surgery on the correct level is absolutely essential in thoracic disk surgery, the sagittal scout film should include all levels of the spine. The levels of the thoracic spine in MRI are counted from the cervical spine; however, intraoperative corroboration of the correct level of pathology often involves fluoroscopic vertebral counting from the lumbar spine. Because anatomical variations are relatively common, a complete spine roentgenogram or MRI scout films are necessary. FIGURE 12–1 (A) Preoperative sagittal CT-myelogram and (B) sagittal T-2 weighted MRI of the thoracic spine (middle) disclose calcified disk herniation with severe spinal cord compression in a patient with radiculomyelopathy. (C) The postoperative sagittal MRI demonstrates excellent decompression of the spinal cord. Surgical Instrumentation and Preparation The following instruments are necessary to perform endoscopic transpedicular thoracic diskectomy: As previously mentioned, the use of a fluoroscopic C-arm is necessary for localizing and operating at the correct level of pathology. The endoscope used for this procedure is a 4 mm diameter, 18 cm length rod-lens rigid endoscope. A 3 mm endoscope can be used, but it does not produce a full-screen image. The image quality is much better with a 4 mm than a 3 mm endoscope. For the start of the endoscopic transpedicular approach, a 0-degree-lens endoscope is used. Disk removal in front of the spinal cord is then performed under a 70-degree-lens endoscope. An endoscope holder is an important tool for tightly securing the endoscope during disk removal because it allows the surgeon to use two hands simultaneously. Two different types of endoscope holders are currently available. The first is a manual holder, which has joints that need to be tightened manually. The other is a nitrogen gas-powered holder, which is controlled with one-touch buttons. An endoscope lens-cleansing device is an essential tool for intermittent cleaning of the lens and is controlled by a foot pedal. A slender power drill is another important tool; the shaft of the drill is ~5 mm, and the drill tip is a round 2 mm cutting bit. A special down-cutting curette system is used. A disposable 1.1 or 1.5 cm diameter trocar is threaded at the outer surface and has a stylet for introduction. Other instruments used are pituitary rongeurs (i.e., straight, curvedup, and curved-down), Kerrison rongeurs (i.e., 1 and 2 mm tips), French number 7 suction cannulas (i.e., straight and curved-down), and suction-coagulators. Somatosensory monitoring is also useful for monitoring intraoperative spinal cord function. Anesthesia General anesthesia with conventional orotracheal intubation is used. Because the operating time is usually 1 to 2 hours, Foley catheterization is not necessary. Positioning The patient is positioned 60 degrees ventrally inclined lateral, with the operating side facing up (Fig. 12–2). An axillary roll is placed, and a pillow is folded as a floating armrest with bear hugging. The legs are cushioned; the shoulders, pelvis, and legs are securely taped with 2-inch adhesive tapes. The operating level is corroborated using a fluoroscopic C-arm, and an 18-gauge spinal needle is placed obliquely under sterile conditions. The skin entry site of the spinal needle is 2 to 3 inches lateral from the midline, with the needle tip aiming at the upper edge of the pedicle. The surgeon and scrub nurse stand at the dorsal aspect of the patient. The video-system tower and the endoscope lens-cleansing motor are placed on the other side of the patient. FIGURE 12–2 This schematic drawing demonstrates patient positioning. The patient is positioned lesion-side-up lateral decubitus. The patient is inclined forward at 60 degrees. An axillary roll is placed under the axilla to prevent neurovascular injury. The correct level of herniated disk is corroborated using fluoroscopic C-arm or roentgenogram. Surgical Technique The localizing spinal needle is left in position, while preparation and draping are done following aseptic technique. The endoscope system is assembled with a 0-degree lens, and the endoscope is mounted to the holder. A 1.5 cm (for the use of a 1.1 cm trocar) or 2 cm (for the use of 1.5 cm trocar) transverse skin incision is made laterally from the lateral margin of the corresponding spinous process. The paraspinal muscles are dissected from the spinous process, lamina, and transverse process using a small periosteal elevator. A localizing spinal needle is used again to confirm correct surgical trajectory and is then removed. A tubular threaded trocar measuring 1.1 or 1.5 cm in diameter is introduced, exposing the facet and lamina (Fig. 12–3). A smaller 1.1 cm diameter trocar is used in the approach to laterally herniated disks causing radiculopathy. The 0-degree-lens endoscope is mounted to the endoscope holder and introduced into the trocar. Endoscopic view will demonstrate surgical landmarks (e.g., the inferior edge of the lamina and inferior edge of the facet), and transverse process is confirmed. The medial portion of the facet, the very lateral portion of the lamina, and the rostral-medial one-third portion of the pedicle are removed with a high-speed drill. When the yellow ligament is removed, a ~2 to 3 mm portion of the very lateral margin of the spinal cord dura mater is exposed. The nerve root can usually be identified rostral to the intervertebral disk, but it may occasionally be found just rostral to the resected portion of the pedicle. The nerve root compression can be identified at this point for radiculopathy. Using a high-speed drill with a 2 mm cutting bit, the lateral bony spurs rostral and caudal to the herniated disk are removed, creating a small cavity, ~5 mm in depth, in the posterior portion of the vertebral bodies. Limited exposure of the spinal cord dura mater will prevent the surgeon from injuring the spinal cord because the main portion of the spinal cord will still be covered by the remaining ipsilateral lamina. The exposed portion of the dura mater corresponds to the subarachnoid space. After a ~1 cm wide cavity is created at the lateral intervertebral disk space by resection of the bony spur and disk material, the 70-degree-lens endoscope is introduced. FIGURE 12–3 This photo shows placement of a 1.5 cm diameter threaded trocar (green) toward the thoracic disk in a thoracic spine model. The trajectory of a trocar is aimed toward the operating intervertebral disk. A 0-degree-lens endoscope will provide a view at the ipsilateral lamina and facet joint. The 70-degree-lens endoscope is mounted to the endoscope holder. It is used to visualize the ventral aspect of the spinal cord dura mater directly. Under this direct endoscopic visualization, the cavity created lateral to the spinal cord is extended further medially by removing disk material and bony spurs with down-biting curettes (Fig. 12–4). An extended tunnel is made underneath a thin layer of dorsally protruded disk and bony spur that is compressing the spinal cord. The shell of disk material and bony spur are pushed away from the spinal cord toward the created cavity and are removed using a longarmed down-biting curette and a curved pituitary rongeur (Fig. 12–5). Because the common pathology in thoracic disk herniation is calcified disk or protruded bone spurs along the edges of the inter-vertebral disk rather than soft disk herniation, creating a small cavity anterior to the compressive pathology is an important step of surgical maneuvering to prevent spinal cord damage. Operating under the 70-degree-lens-endoscope image requires an advanced level of endoscopic technique. When adequate decompression has been performed, the ventrally concave curvature of the spinal cord dura mater bulges out ventrally to make a convex curvature toward the intervertebral space (Fig. 12–6). Bone bleeding is controlled with the application of bone wax, and the trocar retractor is removed. A couple of stitches are placed at the paraspinal fascia if possible, and local anesthetic is infiltrated to minimize postoperative incisional pain. Subcuticular skin closure is done, and a small bandage is applied. This transpedicular thoracic diskectomy can be performed on an outpatient basis or with overnight stay in the hospital. FIGURE 12–4 This schematic drawing depicts the placement of a 1.5 cm trocar retractor via a 2 cm paramedian transverse skin incision, the application of the 70-degree-lens endoscope, and the use of a right-angle down-biting curette for removal of the protruded disk ventral to the spinal cord. The patient is positioned right-side up and inclined 60 degrees ventral and lateral. FIGURE 12–5 This schematic drawing demonstrates removal of a herniated disk in front of the spinal cord with use of a curved down-cutting curette under a 70-degree-lens endoscope. C, Spinal cord; D, herniated disk. Discussion Patterson and Arbit first introduced the transpedicular approach to thoracic disk herniation in 1978.7 Stillerman et al reported a similar surgical technique to thoracic disks and called their surgical maneuver a transfacet pedicle-sparing approach.9 The surgical procedure adopted in the authors’ endoscopic transpedicular approach is very similar to that microscopic technique.3 Minimally invasive surgical technique requires tremendous precision because the margin of error is so narrow that being a bit off the surgical target will lead to frustration and a possible surgical disaster. Accurate localization of the surgical target with the fluoroscopic C-arm is essential to achieve precision to the surgical target. The surgical landmark is the crossing point of a line drawn along the inferior margin of the facet process horizontally and a vertical line drawn along the midpoint of the facet joint. The crossing point of these two lines will lead to the rostral portion of the pedicle. Other landmarks are the transverse processes of adjacent vertebrae and the inferior margin of the lamina. The facet joint can be identified just medially between the transverse processes. The intervertebral disk in the thoracic spine is located at the level of the facet joint. To expose the intervertebral disk laterally to the spinal cord, the facet joint has to be partially removed. In addition, the rostral edge of the pedicle in the thoracic spine is so close to the intervertebral disk that the rostral-medial one-third portion of the pedicle at the lower vertebra has to be removed for adequate exposure of the superior bony edge of the lower vertebra adjacent to the intervertebral disk. The surgical procedure from the skin incision to trocar placement is fast and straightforward, lasting only a few minutes. The very lateral portion of the laminae and the medial portion of the facet joint are removed using a high-speed drill with a 2 mm cutting bit. Drilling of the bone under a 0-degree-lens endoscope requires practice because it is performed under a two-dimensional view, which eliminates visual depth perception. Surgical approach is made under a 0-degree-lens endoscope, and diskectomy ventral to the spinal cord is performed under a 70-degree-lens endoscope without normal depth perception. When a 3D endoscope is fully developed, endoscopic stereoscopic images will provide the surgeon with improved depth perception; however, a surgeon who is fully advanced in endoscopic surgery can have adequate perceptional surgical guidance even under a two-dimensional image using other visual and tactile cues. As Patterson and Arbit originally reported, it is important to create a small cavity lateral to the spinal cord first by removing the bony spur of the rostral and caudal vertebra in addition to the removal of the intervertebral disk before any attempt at removal of the disk is made medially.7 A surgical exposure, however, should not produce postsurgical mechanical instability. The lateral portion of the facet joint has to be preserved for that purpose. In addition, the cavity created anterior to the herniated disk should not compromise the spinal integrity. The remaining disk in the intervertebral disk space is preserved, not disintegrated. FIGURE 12–6 An intraoperative picture taken with a 70-degree-lens endoscope reveals a protruded calcified disk, which is indenting the ventral aspect of the spinal cord (A). When the protruded disk is removed, the ventral aspect of the spinal cord dura mater bulges out toward the cavity created at the intervertebral disk space (B). Surgical tools are curved to access the ventral aspect of the spinal cord. Operating under the 70-degree-lens endoscope is very difficult and confusing until the surgeon becomes skilled in endoscopic technique. The lateral 2 mm portion of the spinal cord dura mater is exposed, and this limited exposure of the spinal cord helps to avoid inadvertent spinal cord damage. In addition to the confusing view of the 70-degree-lens endoscope, the use of oddly curved surgical instruments may prove to be an initial technical challenge for the surgeon. An endoscope holder is essential to maintain a steady image on the monitor and to allow the surgeon to use both hands. An endoscope-cleansing device is another integral element in this technique. Although the endoscope cleaner that is commercially available at present is not yet ideal, it does significantly aid the surgeon in operating continuously without the frequent interruption of having to move the endoscope to clean a foggy or blood-stained lens. Although we have not experienced any cases of intraoperative spinal cord damage, the main potential risk of this endoscopic transpedicular technique is still spinal cord damage. SEP monitoring has been used in all patients; however, its use does not preclude the development of spinal cord injury intraoperatively. The display of SEP changes occurs a few minutes after they actually happen. In addition, it provides only posterior column function of the spinal cord. Once a surgeon desires to use an endoscope through a posterior approach to the treatment of thoracic disks, a posterolateral extracavitary approach may be an easy operation to start with. With this wider and further lateral exposure, a surgeon can become accustomed to the use of a 70-degree-lens endoscope more easily. Once the surgeon’s endoscopic skill has improved with practice, a more restricted surgical exposure such as a transpedicular approach can be applied. Endoscopic inspection of the ventral aspect of the spinal cord alone is not difficult. When decompression of the spinal cord is achieved, the spinal cord dura mater bulges out ventrally toward the diskectomy cavity, showing convexity on the endoscopic view. The lack of this dural ventral bulging means inadequate decompression of the spinal cord. Inadequate decompression of the spinal cord is obviously another potential undesired outcome, and nerve root damage is another possible complication. The lack of depth perception in two-dimensional endoscopic images may lead to injury of the nerve root while the facet joint is removed. When the surgeon becomes familiar with the surgical technique, the patient’s postoperative recovery, the amount of surgical invasiveness, and the complexity of the surgical procedure may become comparable to that of cervical or lumbar diskectomy. The endoscopic transpedicular approach provides a minimally invasive surgical option for treating thoracic disk herniation. Access to the ventral spinal cord is obtained through a 1.1 or 1.5 cm trocar with the use of a 0-degree-lens rigid 4 mm endoscope for visualization during drilling of the medial portion of the facet, lateral lamina, and rostral-medial pedicle of the lower vertebra. A mounted 70-degree-lens endoscope provides direct visualization of the ventral spinal cord during decompression of the spinal cord with 90-degree-curved surgical instruments. As adjuncts, fluoroscopic C-arm and somatosensory monitoring aid in the guidance of the surgical approach and in the detection of intraoperative complications, respectively. When skillfully performed, endoscopic transpedicular thoracic diskectomy provides high levels of symptomatic resolution and low complication risks. REFERENCES 4. Jho HD. Endoscopic transpedicular thoracic discectomy. J Neurosurg. 1999;91:151–156.
12

Endoscopic Transpedicular Thoracic



< div class='tao-gold-member'>
Endoscopic Transpedicular Thoracic Diskectomy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








