Fig. 10.1
Effect of collagen shrinking by heat
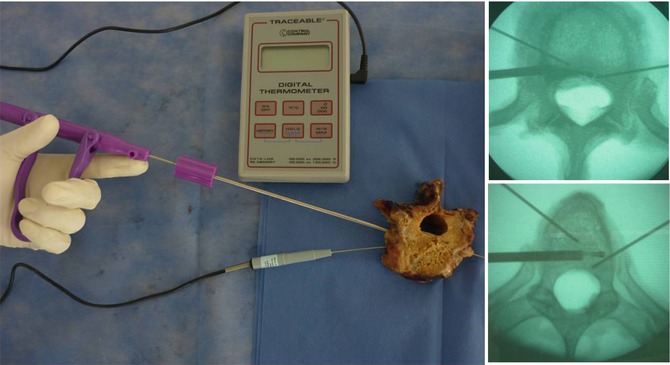
The evidence of the effectiveness and safety of this method in low back pain has been described in various reports. Saal and Saal [13] stated a hypothesis in which thermal energy may play a role in the treatment of radial tearing of the intervertebral disc and thus treat low back pain. Later, Feldman and Hellinger [3], Hellinger [4], and Ramirez et al. [9] independently studied the intradiscal thermal effect of high frequency using radio frequency in human specimens. These studies showed a significant shrinking of the intervertebral disc and widening of the spinal canal. These studies also indicated the safety of the energy, which was done through continuous surveillance of the energy. This was done by continuous monitoring, using temperature sensors, and observing with an infrared camera during nucleus ablation (Fig. 10.2) and annulus modulation. These studies, along with the ones done by Yeung et al. [16], proved that radio frequency is a more refined and easier to canalize tool, which allows the surgeon to treat specific areas of the disc with a minimal impact on the adjacent tissue.
Among the indications for the performance of the procedure, we must find a patient with a previous clinical history longer than 6 months of discogenic pain, treated with NSAID, analgesics, lumbosacral support and physical therapy during at least 3 months. In radiological findings, images coherent with degenerative disc disease, black disc disease, bulging disc disease, annular tearing, contained disc herniation, or facet osteoarthritis must be found [8].
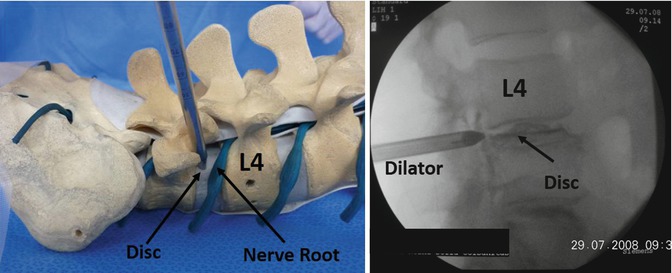
There are some pathologies in which thermal diskoplasty is contraindicated. These exceptions are discopathy with height loss over 50 %, segment instability (Fig. 10.3) [1], disc extrusion or sequestering, cauda equina syndrome, infection, incontrollable coagulopathy and bleeding disorders, and discography that does not agree with previous low back or radicular symptoms [14].


Fig. 10.3
Contraindications Left dots show the instability; Right circle show a extruded central hernia
To perform a thermal diskoplasty, there are several thermal therapy devices like the laser (now outdated due to its limited security margin) and radio frequency (Fig. 10.4). Thus, it is essential to have an energy source designed for this. Thermal therapy is applied using fibers that percutaneously or through the endoscope’s work channel get to the inner part of the disc and, being bipolar, guarantee even and safe heat transmission.
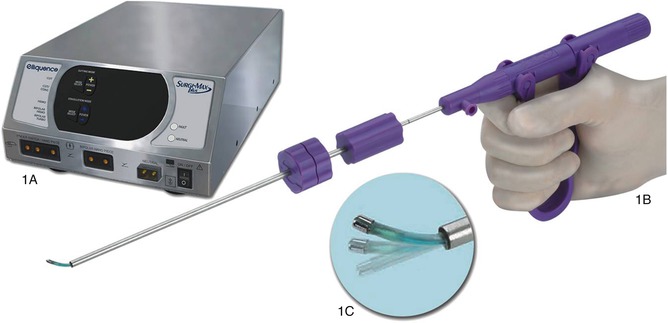
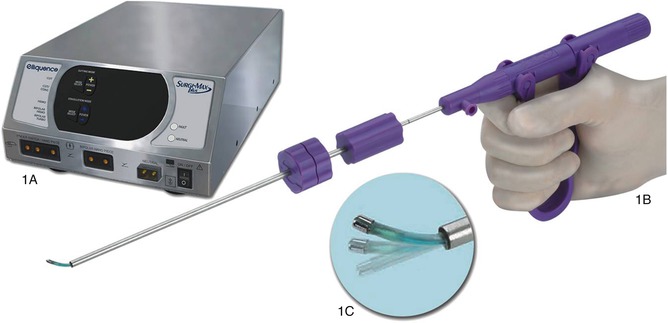
Fig. 10.4
Radio-frequency console and fiber (ElliquenceTM). 1A Energy source (Surgimax, Elliquence NY). 1B Disc Fx RF Fiber. 1C Disc Fx Tip
Surgical Technique: The patient lies prone on a radiolucent table, and two cylindrical pillows are placed, one in the thoracic zone and the other in the pelvic zone, flexing the hip from 60° to 90° (Fig. 10.5). The place of the surgeon is on the ipsilateral side of the affected disc, with the assistant next to him.


Fig. 10.5
Patient position
The approach is achieved entering percutaneously keeping a midline between 8 and 12 cm, with an epidural needle with a 45° angle. After verifying an adequate positioning using the fluoroscope with anteroposterior and lateral projections, we proceed to perform the discography (Fig. 10.6).
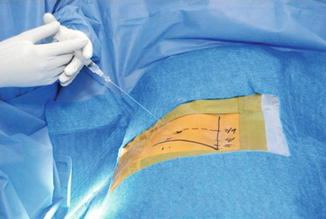
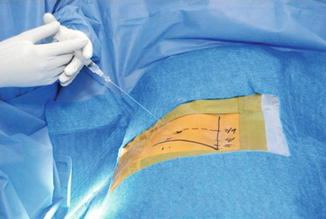
Fig. 10.6
Positioning of the needle and injecting the contrast agent in the disc
Discography is a diagnostic test, which allows an assessment of the disc from two points of view: the anatomical, because it allows observing its radiological pattern and the physical properties of the nucleus, along with the presence of rupture in the annulus, and the functional, because it allows the surgeon to obtain a subjective measurement of the resistance to injecting the contrast agent and the reproducing of pain or the aforementioned discogenic test.
TDP: After determining the affected level, we proceed to obtaining access to the disc and the annulotomy using a dilating cannula and trephine system, which are passed sequentially and always under the safety and verification of the fluoroscope.
To allow an adequate access to the radio-frequency fiber and at the same time perform a nucleus resection, we do a mechanized diskectomy using grasping forceps. This procedure permits removing a great volume of the affected disc and, in this way, proceeding to perform the thermal therapy with radio frequency achieving ablation of the nucleus and modulation of the annulus with the aforesaid effects (Fig. 10.7).
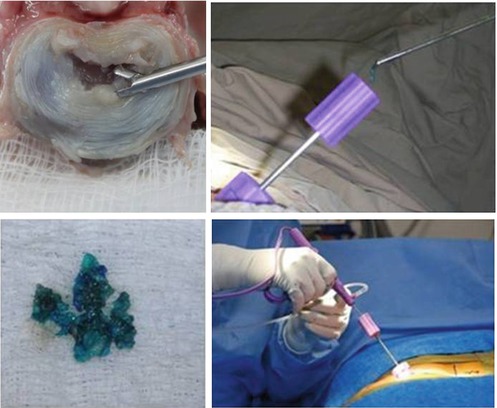
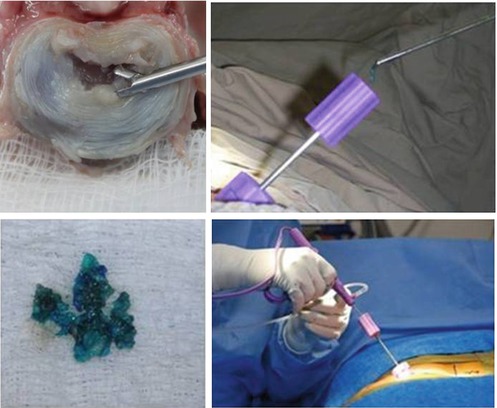
Fig. 10.7
Mechanized diskectomy and percutaneous thermal therapy
Depending on the indication and the pathology, this procedure may be complemented with an endoscopy, taking into account that it allows the visualization of the structures that might be compromising the nerve root, therefore being the source of radicular pain.
360° Rhizolysis for Facet Syndrome: Denervation with radio frequency in the facet articulation is a complementary measure to low back pain treatment, and its success is based on the adequate selection of the patients, along with a strict following of the surgical procedure. One of the biggest advantages of this type of procedures is that both techniques may be done in the same surgical act without moving the patient, only changing the approach.
The entry site is determined, which is the most lateral point of the pedicle, a caudal level of each lumbar level, except in L5–S1 (Fig. 10.8). Under fluoroscopic vision, we identify the facet of the affected level where the dilator and the cannula, which will allow to the radio-frequency fiber to pass, are to be inserted.
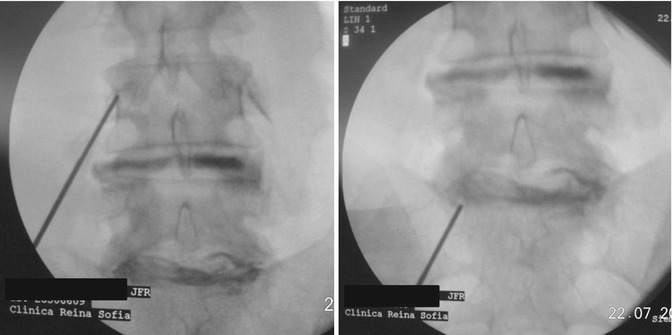
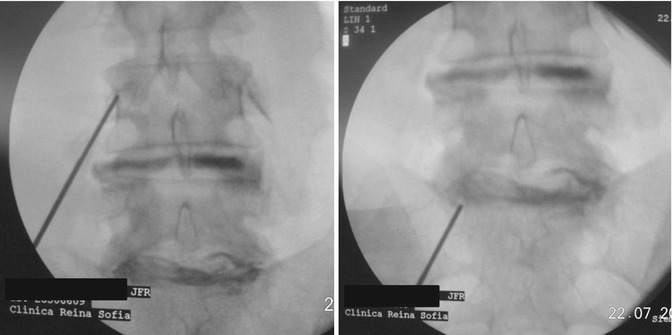
Fig. 10.8
Positioning of the cannula for levels L4–L5 and L5–S1
Radio-frequency fiber is moved until contact with the bone is lost and its position is identified with fluoroscopy. A lateral view assures that the tip of the radio-frequency fiber does not go into the limits of the intervertebral foramen.
With the tip of the radio-frequency fiber located inside the facet articulation, the Surgi-MaxTM (Elliquence LLC, New York) energy source is activated on the bipolar Hemo-mode to a standard intensity of 25 during 6 s. This reaches a 75–80 °C temperature. Four points are established (cranial, lateral, caudal, medial), and the handle of the fiber is rotated 360° to completely cover the extension and, in this way, apply thermal therapy to nerve endings of the articular capsule (Fig. 10.9).
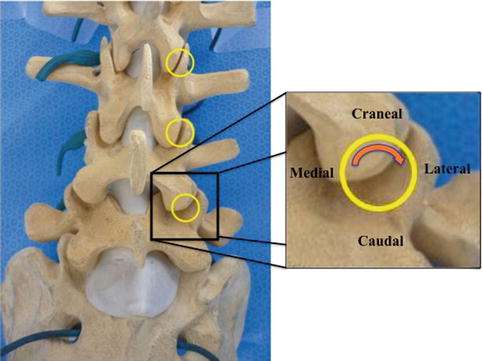
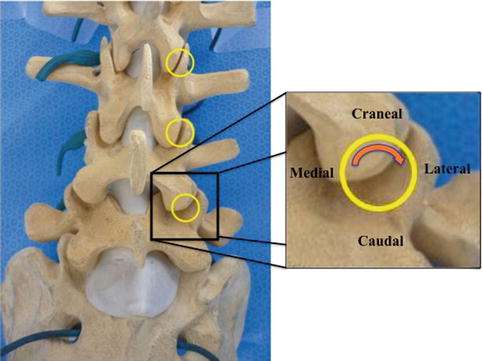
Fig. 10.9
Facet 360° rhizolysis diagram. Circle are the entry point toward the Facet Joint
The levels that are going to be treated have been previously identified based on clinic and radiological findings, taking into account that the most common ones correspond to the levels between L3 and S1 (Fig. 10.10).
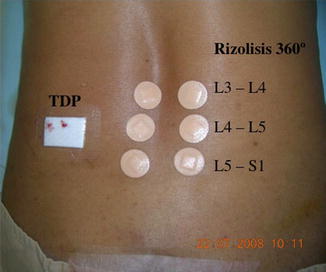
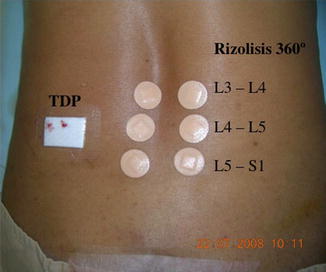
Fig. 10.10
Thermodiskoplasty with posterolateral approach and rhizolysis with posterior approach, in the same surgical act
10.2 Disc Hernia and Low Back Foraminal Stenosis Treatment via Endoscope
Given its characteristics, endoscopic spine surgery requires special devices to be implemented. The endoscopic video tower is vital, and, in general terms, a standard tower comprises a screen, a video processor, a light source, and a camera; it can also have a shaver console and an irrigation pump (Fig. 10.11).


Fig. 10.11
Endoscopic tower (Richard Wolf GmbH, Germany)
Percutaneous endoscopic lumbar discectomy is recommended in contained hernia diagnoses by MRI, failure in conservative therapies (6-week physical therapy, NSAID, analgesics, and lumbosacral support showing no improvement), low back radicular persistent pain, and epidural or radicular blockage with partial improvement, in agreement with the discography and a positive discogenic test before the procedure done by the attending. Nevertheless, it is contraindicated when there is anatomical abnormality, segment instability, narrow lumbar canal, extruded and migrated hernia, and cauda equina syndrome.
10.2.1 Transforaminal Approach
Surgical Technique: We used a prone position and a posterolateral approach like TDP. A dilator is passed over the guide to separate the tissue. With a scalpel, we make a 1 cm incision that lets the endoscope sleeves pass through the muscles and over it, the endoscope (Fig. 10.12).