Tremor is the most common movement disorder and denotes a rhythmic involuntary movement of one or several regions of the body (1). Although most tremors are pathologic, a low-amplitude, high-frequency physiologic action tremor can be detected in all normal subjects. Pathologic tremor is visible to the naked eye and mostly interferes with normal motor function. The disabilities caused by these tremors are as diverse as their clinical appearance, pathophysiology, and etiologies. Although there are numerous medical treatment options, their efficacy is limited, and therefore, refined stereotactic surgical approaches have become increasingly important for the most severe cases.
CLINICAL DEFINITIONS
The clinical examination of tremor patients should focus on certain aspects of the tremor, which are the basis for the differential diagnosis and should always be documented.
Tremors can occur in any joint or muscle that is free to oscillate. The patient should be examined carefully under different conditions to be able to detect all the affected body parts. Both distribution and symmetry are important. Tremor is also described depending on the activation condition leading to appearance or a marked increase of tremor severity. Resting tremor occurs when the muscles of the affected body part are not voluntarily activated. Rest tremor must cease or be suppressed when a voluntary movement is initiated or performed. Action tremor is any tremor that is produced by voluntary contraction of muscles and covers postural and kinetic tremor. Postural tremor is present while voluntarily maintaining a position; kinetic tremor occurs during voluntary movement. Simple kinetic tremor is seen during purposeless voluntary movements. Goal-directed tremor (most commonly labeled as intention tremor) occurs when a target is reached. Rarer forms of action tremor occur only during certain positions or tasks (task- or position-specific tremor or isometric tremor).
With some experience, the three main frequency ranges can be separated on inspection: high (>7Hz), medium (4–7 Hz) and low (<4 Hz). Analysis with accelerometers and electromyography (EMG) might also complement tremor assessment (Fig. 27.1).
Additional signs and symptoms are equally important as the tremor characteristics. For example, a parkinsonian syndrome, neuropathy, cerebellar ataxia, and dystonia are important diagnostic and etiologic hints.
ESSENTIAL TREMOR
DEFINITION
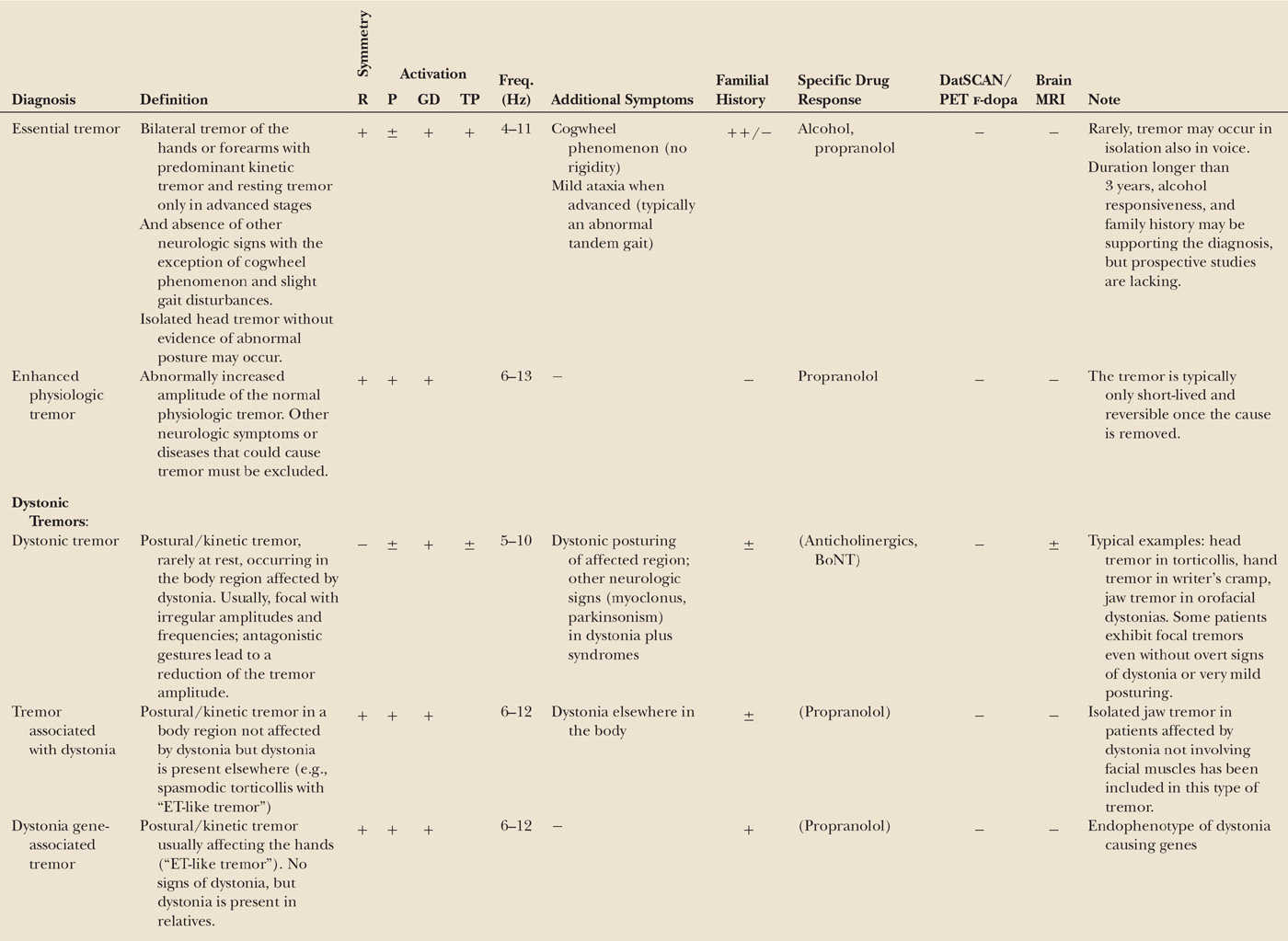
Essential tremor (ET) is a slowly progressive tremor disorder which is sometimes causing severe disability but is not life-limiting. The traditional view of ET as a monosymptomatic disorder has been revised, as this disorder is more complex and heterogeneous. A physiologic or laboratory test for the validation of the diagnosis is still lacking. Therefore, the heterogeneity may partly be due to diagnostic uncertainty, with different sets of diagnostic criteria all using only medical history and clinical findings (Table 27.1). Some stricter criteria used for research purposes involve a disease duration longer than 5 years and the severity of the tremor (2). There is general agreement that this definition is too broad and needs revision.
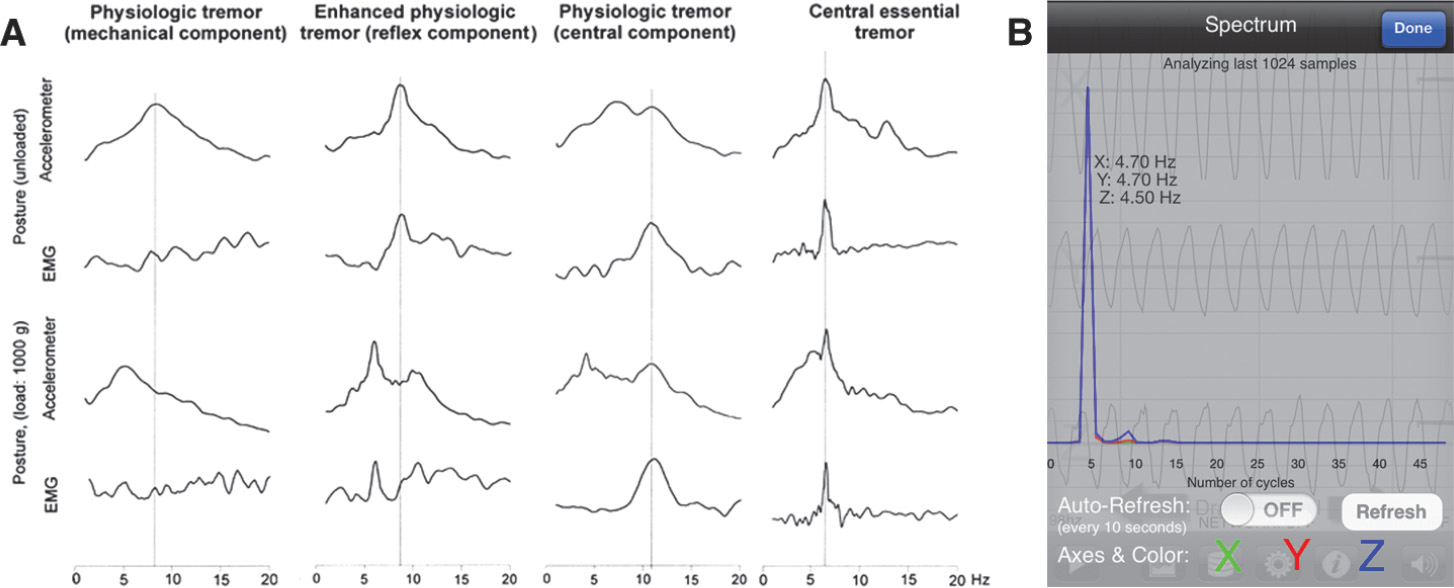
Figure 27.1. (A) Spectral analysis of four different postural hand tremors with the accelerometer spectrum and the EMG spectrum of the wrist extensors unloaded and with a load of 1,000 g mounted on the back of the hand. In physiologic tremor, the tremor is detectable on accelerometer, but there is no EMG activity, and a load-dependent mechanical resonance peak is present (note the shift of the frequency). In enhanced physiologic tremor, a reflex-activated tremor might be detectable because the EMG frequency peak decreased with the accelerometer peak during loading. The third example is from a normal subject having a central, frequency-invariant component in addition to the load-dependent mechanical component. In essential tremor, like most pathologic tremors, there is a central component with a frequency-invariant EMG peak. (B) A very easy and rapid measurement of tremor frequency is to use the in-built accelerometer of smartphones. Accuracy closely matches the more sophisticated tremor analysis. (A from Deuschl G, et al. The pathophysiology of tremor. Muscle Nerve 2001;24(6):716–735.)
| Movement Disorder Society Consensus Criteria for the Diagnosis of Essential Tremor |
Inclusion Criteria
1. Bilateral, largely symmetrical postural, or kinetic tremor involving hands and forearms that is visible and persistent
2. Additional or isolated tremor of the head might occur but in the absence of abnormal posturing
Exclusion Criteria
1. Other abnormal neurological signs; especially dystonia
2. Presence of known causes of enhanced physiologic tremor, including current or recent exposure to tremorogenic drugs or presence of a drug-withdrawal state
3. Historical or clinical evidence of psychogenic tremor
4. Convincing evidence of sudden onset or evidence of stepwise deterioration
5. Primary orthostatic tremor
6. Isolated voice tremor
7. Isolated position-specific or task-specific tremors, including occupational tremors and primary writing tremor
8. Isolated tongue or chin tremor
9. Isolated leg tremor
CLINICAL FEATURES (Table 27.2)
Motor Features
The topographic distribution shows hand tremor in 94%, head tremor in 33%, voice tremor in 16%, leg tremor in 12%, jaw tremor in 8%, facial tremor in 3%, and tremor of the trunk in 3% of the patients (3,4). Head, voice, or chin might be involved in isolation (5), but these tremors are considered dystonic in nature by many researchers (and are rarely seen in familiar forms of ET). Fifty percent to 90% of the patients improve with ingestion of alcohol which is used as a secondary criterion, but the finding is not specific for ET (e.g., it might be effective in dystonia).
ET often starts with a postural tremor which can still be suppressed during goal-directed movements. In advanced stages, an intention tremor can develop and is accompanied by signs of cerebellar dysfunction of hand movements like movement overshoot and slowness of movements (6). A population survey found that 80% of ET patients were never seen by a neurologist. Also, difficulties during tandem gait are frequently found (7); this accounts for the fragility and balance difficulties sometimes observed in older patients with ET. In more advanced stages, a tremor at rest can develop (8) which can be separated from other resting tremors as it is not or only mildly suppressed during movement onset (9). Subtle signs of cerebellar dysfunction have been shown also for hand and elbow movements (10,11), subclinical eye movements (12), cerebellar rhythm generation (13), motor learning deficits during an eyeblink conditioning protocol (14), and temporal discrimination task (15).
Nonmotor Features
Several recent studies have described clinically subtle dysfunction of attention and executive functions, such as deficits on tests of verbal fluency, naming, mental set-shifting, verbal and working memory, complex auditory attention, visual attention, and response inhibition (for a review, see (16)). A distinct personality profile has been found in ET (more tender-minded and less aggressive than the normal population with a trend toward social introversion) (17) matching with higher scores in the harm avoidance scale of the tridimensional personality questionnaire in another study (18). Behavioral symptoms that are found to be associated with ET include anxiety, phobic anxiety, and depression (19–21). Both the mild frontal dysexecutive syndrome and the slight personality changes have been interpreted to reflect a relative dysfunction of frontal areas due to a remote effect within the cerebellothalamo–cortical circuits as a consequence of cerebellar dysfunction (22,23). A deficit of hearing (primarily caused by cochlear involvement) (24) and olfaction is still controversial (25–27) and probably irrelevant.
A series of prevalence and incident studies, including the large NEDICES Study Project, which was a survey of major neurologic disorders in people aged ≥65 years living in three communities of central Spain (for a review, see (28)) described an association of senile ET (onset >65 years) and dementia (28–30). Other nonmotor features include poor sleep quality and reduced body mass. The significance of these results remains unclear given the fact that the ET patients were almost twice as likely to be depressed (31).
CLINICAL COURSE
The condition may begin in childhood, but the incidence is increasing above 40 years with a mean onset of 35 to 45 years in different studies and an almost complete penetrance at the age of 60 (4,32). Young-onset ET is very often familiar and probably represents a subtype different from classic form and senile ET (33). Progression of tremor severity was found to be 1 point on the rating scale per year, and predictive factors were older age, longer disease duration, and the presence of voice tremor (34). There is a decrease of tremor frequency and a tendency to develop larger amplitudes (35). Intention tremor develops at various intervals between 3 and 30 years after the onset of postural tremor (10). For a generic quality-of-life (QoL) questionnaire, ET patients scored worse in all eight domains of the SF-36. Tremor severity correlated with some of the physical domains as well as with social function of the mental domains (17). Up to 25% of the patients seeking medical attention must change jobs or retire from work (36,37).
EPIDEMIOLOGY
ET is the most common adult movement disorder albeit its epidemiology is still not clear. Due to application of imprecise and variable diagnostic criteria, prevalence estimates are ranging from 0.008% to 22%, with a substantial increase with age. Patients with ET were assumed to have mortality rates similar to those in the general population (38). However, in a retrospective study they were found to live longer (39), while another longitudinal prospective population-based study found the risk of mortality to be slightly increased (28,40). These controversial results suggest only a minor effect of the disease on mortality and also critically depends on the definition of ET, but additional studies are needed.
PATHOGENESIS
Genetics and Environment
The majority of cases are hereditary. The families which have been described hitherto have shown an autosomal-dominant inheritance with an almost complete penetrance at the age of 60 to 70 years. Twin studies suggest a heritability of up to 95% (33,41). However, 20% to 40% of the patients are sporadic.
So far, no gene has been found. Linkage mapping studies have found at least three loci for familial ET on chromosome 3q13 (ETM1, OMIM 190300) (42), on chromosome 2p24.1 (ETM2, OMIM 602134) (43,44) and in two families the third ET susceptibility locus (ETM3, OMIM611456) (45) on chromosome 6p23. ETM1 is the only locus independently replicated and contains the gene DRD3, whose variant has a nonsignificant trend toward an overrepresentation in ET compared with controls and has been also found to determine severity and age at onset of tremor. Among the candidate genes included in the ETM2 region, the Ala265Gly rs11680700 variant of HS1BP3 exon 7 (heat shock1–binding protein 3) was reported in families with ET but not replicated by others.
A stop mutation (c.868C>T; p.Gln290*) in the FUS gene was found as the possible cause of ET in a large Franco-Canadian family (46). This study and three follow-up studies identified three further missense mutations in 718 sporadic and “familial” patients (46–49). In addition, a large study identified a novel risk variant (Met392Ile) in the FUS gene that increases susceptibility of ET among ethnic Chinese (50). If this is the first genetic variant of ET, it seems to be very rare. In addition, many candidate gene approaches (including the genes involved in other movement disorders or in the metabolism of GABA) have been unsuccessful so far, but many of them were only applied in small populations (for review, see (51)).
Genome-wide association studies (GWASs) have found the “leucine-rich repeat and Ig domain containing 1” (LINGO1) in Icelandic people with ET (52). Replication studies have shown mixed results, and a recent meta-analysis has suggested a relationship between LINGO1 rs11856808 polymorphism and the risk for both familiar and sporadic ET, while rs9652490 polymorphism was only related with the risk for familial ET (53). A GWAS found an association between the SLC1A2 gene and ET (54). SLC1A2 encodes the major glutamate reuptake transporter (EAAT2) in the brain and is highly expressed in the inferior olive. So far, no replications have been published.
The environmental factors which may cause tremor are understudied. β-Carboline alkaloids (including harmine and harmane) are known to cause tremor in animals and men and were found to be elevated in the blood of patients with either sporadic or familiar ET (55). Other studies describe an association between ET and blood lead concentration as well as a possible interaction with allele status for the d-aminolevulinic acid dehydratase, a principal enzyme involved in lead kinetics (56). The regular assumption of small quantities of alcohol seems to be protective, while larger use seems to be a risk factor (57). One study reported the protective role of smoking.
Animal Models
Harmaline, which induces synchronized rhythmic activity of inferior olive neurons by increasing their electrotonic coupling, induces a postural/kinetic tremor in laboratory animals that is similar to ET in humans (58). The GABA-A1 knockout mouse represents a novel model (59) and has strengthened the “GABA hypothesis” (see below).
Neuropathology
No consistent pathology is found in ET. One group is finding two pathology types, one with Lewy bodies in the locus coeruleus and another with a cerebellar pathology with torpedoes and a reduction of Purkinje cells (60). The latter shall be more frequent, but two other groups were unable to reproduce these findings (61,62). Interestingly, a very recent study found that the protein levels of LINGO1, but not LINGO2, were significantly increased in the cerebellar cortex of ET patients compared with controls (63). One study failed to find pathologic changes in the inferior olive nucleus (64), whereas another one did not find any reduction of enzymes involved in the metabolism of dopamine (DA) and noradrenaline but a significant reduction of GABAergic neurons containing parvalbumin, a finding particularly present in senile cases (62). This finding is in keeping with the reduction of the density of receptors GABA-A and -B found by another postmortem study (65).
Imaging
One study using the technique of voxel-based morphometry (66) and a controlled diffusion-weighted MRI study (67) could not demonstrate any structural abnormalities in ET. One study found a cerebellar atrophy in patients with head tremor, and it was replicated by following voxel-based morphometry (68). A number of studies used diffusion-tensor imaging (DTI) demonstrated that a widespread disintegrity of cerebral and cerebellar fiber tracts is common and likely underlies tremor generation (for a review, see (69)). Magnetic resonance spectroscopy studies reported a reduced N-acetylaspartate/creatine ratio in ET, possibly indicating neuronal damage or loss in ET which again raised the question of neurodegeneration in ET (70,71). Early positron emission tomography (PET) studies have provided evidence for bilateral overactivity of cerebellar connections in ET and other tremors (72–75). PET studies using [11C] flumazenil found a hyperactivity of GABA receptor (76). Sonography in patients with ET revealed a hyperechogenicity of the substantia nigra in 16%. Nine percent of normal individuals have this feature and 90% of patients with Parkinson’s disease (PD) (77). Again, the significance of these results remains unclear.
Neurophysiology
At cortical-level tremor-related activity can be detected with electrophysiologic techniques. Electro- and magnetoencephalography have been used to analyze the relationship between activity of the motor cortex and the muscles. Coherence tests have shown coherence between activity in the motor cortex and the contralateral hand tremor, indicating a transcortical pathway of these tremor-related signals. Even the premotor cortex is intermittently involved in the generation or transmission of these rhythmic signals to the spinal cord (78). The findings have been interpreted to represent a spatiotemporal pattern of intermittent synchronization within a complex cortical network that is responsible for tremor (79). This “central tremor” network is active in most tremors, but what seems to differ is the cause for the oscillating behavior of this network (80,81).
The cause for this oscillation is unknown but likely to reside within the CNS. Several lines of evidence suggest that the oscillator is located within the Guillain–Mollaret triangle (rubral nucleus, olivary nucleus, and cerebellum), assuming that the tremor may result from abnormal intrinsic oscillations originating in the inferior olive or the cerebellum and spreading throughout the olivocerebellar network (6,82). Hypotheses on the pathophysiology of ET are based on the above-quoted studies on environmental and genetic factors and on several other evidences. In recent years, animal and neuropathologic findings along with the PET studies and the response to GABAergic drugs (see below) have supported the “GABA hypothesis” (83).
TREATMENT
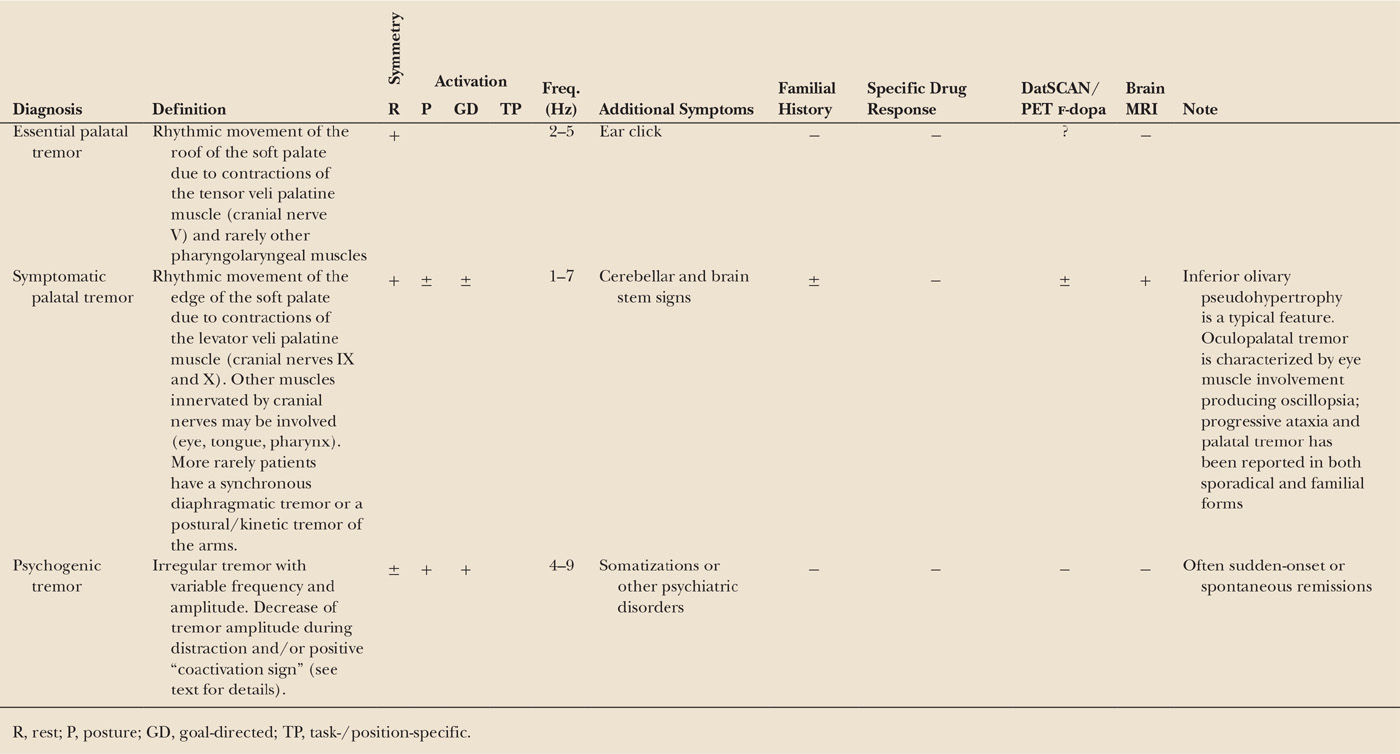
Fig. 27.2 depicts the general principles of tremor treatment, regardless of etiology.
Medical Therapy
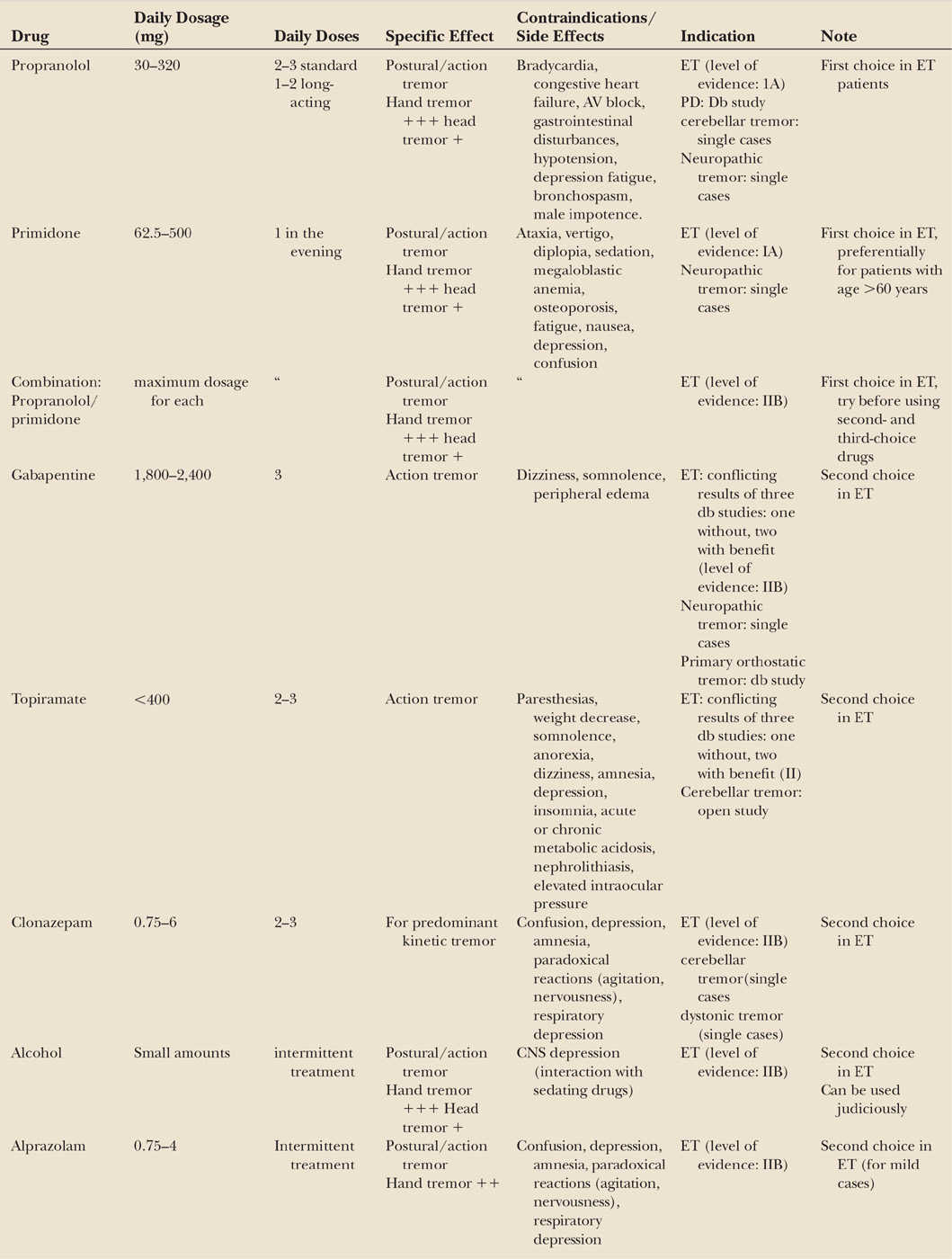
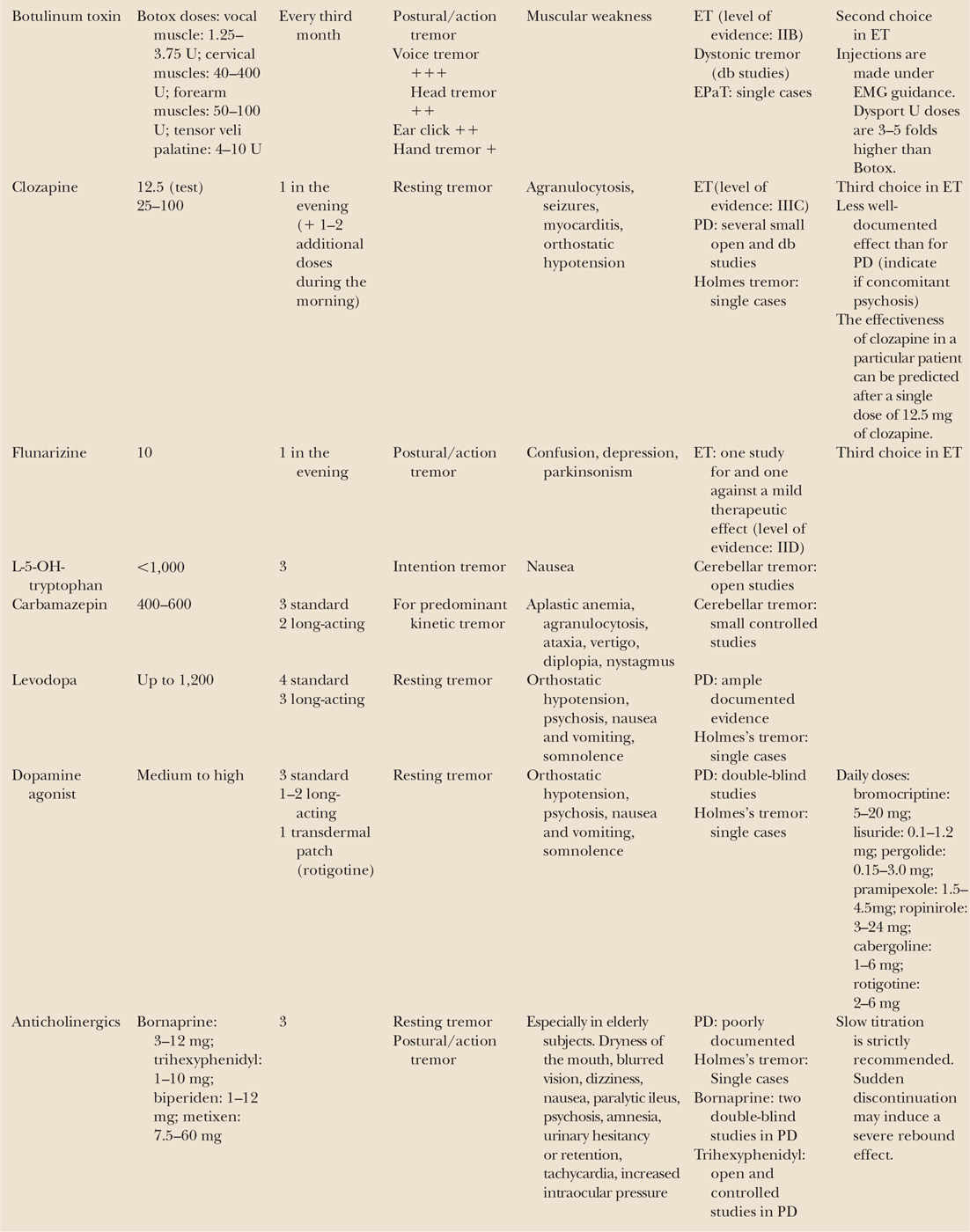
Presently, the medical treatment of ET involves numerous drugs, but only some of them have been studied within randomly assigned, double-blind studies (see Table 27.3 for dosages, side effects, and contraindications). An evidence-based medicine (EBM)-based review on treatments for ET (84) and the guidelines of the AAN (85) have suggested that the first-line (level A, established as effective) pharmacologic agents are propranolol and primidone. Propranolol and primidone are the drugs of first choice for this indication, and both have been carefully studied in the past. They both provide a moderate benefit in almost 60% of patients, but tolerance can develop few years later. Patients who need only intermittent tremor reduction might benefit from taking 10 to 40 mg oral propranolol about 30 minutes before the event. Primidone can result in multiple side effects especially during the titration phase even when a very low initial dose and a graduated titration schedule is used (86). The combination of propranolol and primidone is recommended whenever one of the drugs is insufficient. Topiramate was shown to be effective in two double-blind studies (87,88), while another study failed to prove benefit (89). It might be considered a first-line therapy even if the high number of dropouts has limited the level of evidence for its use and it has been classified as a level B by the AAN.
Second-line (level B, probably effective) drugs include alprazolam, gabapentin monotherapy, atenolol, and sotalol. Alprazolam is helpful especially when anxiety worsens transiently the tremor (90). Gabapentin is effective following two double-blind studies (91), but another double-blind study showed no convincing effect (92). Other β-adrenergic receptor antagonists such as atenolol and sotalol might reduce tremor (93). Generally, drugs with predominant β-1 effects and less potential to cross the brain–blood barrier have been shown to be less effective than those acting on the β-2 receptor, and none has proved superior to propranolol.
Third-line drugs (level C, possibly effective) include clonazepam, nadolol, and nimodipine. Clonazepam is recommended for patients with predominant action and intention tremor in ET (94) but not effective in uncomplicated ET (95).
There is insufficient evidence (level U) to support or refute the use of clonidine, clozapine, gabapentin (adjunct therapy), glutethimide, L-tryptophan/pyridoxine, metoprolol, nicardipine, octanol, olanzapine, phenobarbital, pregabalin, quetiapine, T2000, theophylline, tiagabine, sodium oxybate, and zonisamide.
Figure 27.2. General management of tremor patients. As tremor not always limits function and quality of life, a treatment might become necessary according to patient’s needs.
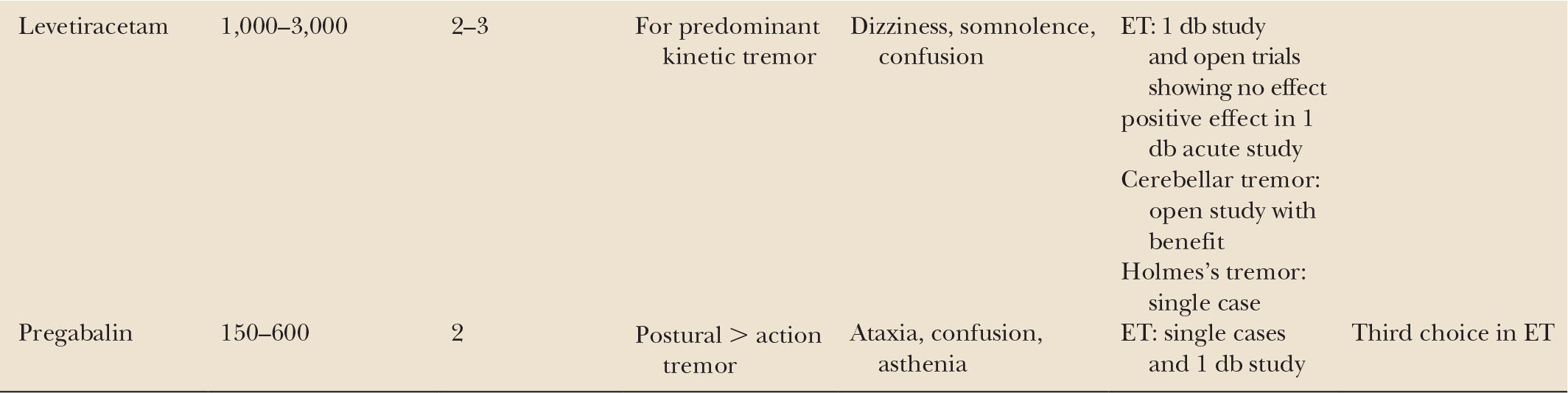
Octanol has been explored by pilot studies with positive effects in patients with alcohol-responsive tremor. The anticonvulsant pregabalin has been reported to be effective in open (96) and double-blind study (97). An open-label trial with sodium oxybate, which is the sodium salt form of γ-hydroxybutyric acid, could demonstrate improvements in postural and kinetic tremor (98,99). Zonisamide, another antiepileptic agent, was tested in a small double-blind and placebo-controlled trial including 20 ET patients but did not provide significant improvements in clinical rating scales and was only modestly well tolerated (100).
Agents with recommendations against use (ineffective) are trazodone (level A), acetazolamide (level B), amantadine (level B), carisbamate (level B), isoniazid (level B), levetiracetam (level B), pindolol (level B), 3,4-diaminopyridine (level B), methazolamide (level C), mirtazapine (level C), nifedipine (level C), and verapamil (level C).
Pharmacologic treatment of head and voice tremor is less efficient than the one of hand tremor. Propranolol and primidone, each alone or both combined, have been recommended for essential head tremor (101,102). Clonazepam is often recommended for this indication, but careful studies are not available.
Botulinum Toxin
Botulinum toxin A (BoNT-A) has been proposed as a treatment for ET (level C, possibly effective), since it may reduce tremor by weakening the muscles or by blocking γ-motor efferents and muscle spindle afferents. Injections with BoNT-A is effective in the treatment of head and voice tremor (84,85,103). Objective acoustic measures have shown the efficacy of BoNT for voice tremor in only a small number of treated patients (104). Subjective evaluations reported benefit in the majority of patients (105–108), and if oral treatment does not work, it should be considered as an option. Head tremor can also be significantly improved (109). BoNT has been used also for hand tremor in a carefully controlled study but showed only limited effect (110).
Surgical Therapy
Surgery is meanwhile the accepted treatment for patients with severe disability but resistance to medical treatment; in absence of class I or II studies, the level of recommendation is C (possibly effective). Multicenter studies have shown that deep brain stimulation (DBS) of the thalamus is effective (111–114), and one study has shown that ventral intermediate nucleus (Vim) DBS has a better effect than Vim-thermocoagulation and more importantly less side effects (115).
DBS reduces tremor severity by about 60% (functionally relevant) in 80% of the ET cases. The standard stereotactic coordinates for thalamic DBS cover a region including the ventral border of the Vim and the adjacent subthalamic white matter (84). In patients with limb tremor, unilateral stimulation may sometimes be sufficient to reduce the disability. In case of disabling bilateral limb tremor or head, voice, and trunk tremor, a bilateral procedure is necessary. As bilateral thalamotomies carry a high risk of dysarthria, dysphagia, or balance problems (116,117), mostly Vim stimulation is applied (113,118). A problem of DBS is the decay of benefit over time (reported up to 73% of patients) (119), whose mechanism is partially unknown and can be explained by disease progression, target choice, or neuronal tolerance.
Other targets, mainly proposed for more difficult tremors (e.g., proximal) are in the caudal zona incerta (Zi) and the prelemniscal radiation (84). These targets warrant further controlled studies because they represent a bottle neck with several fibers, might be associated with less tolerance and require less battery use, as fibers are more sensitive to stimulation than cell bodies.
γ-Knife surgery for the treatment of tremors is proposed in some centers (120), but cases with slowly growing lesions over months (“running lesions”) and subsequent tremor worsening have been published (121). Focused ultrasound producing thalamic lesions in ET was effective in small series, but the side effects need to be studied in larger series particularly because of possible side effects (122,123).
IMPORTANT DIFFERENTIAL DIAGNOSES OF ET
ENHANCED PHYSIOLOGIC TREMOR
Definition
Normal physiologic tremor (PT) is an action tremor and usually not visible. It can only be measured with sensitive accelerometers. An increase of the amplitude leads to the visible enhanced PT (EPT) (see Table 27.2). The pathologic tremor amplitudes are typically only short lived and reversible once the cause is removed. Other neurologic symptoms or diseases that could cause tremor must be excluded (1).
Epidemiology
A recent cross-sectional population-based study has found the prevalence of EPT to be 9.5% in subjects over 50 years of age. EPT was much more common than ET (3.06%) and parkinsonian tremor (2.05%) (124). There are no studies available on the natural cause of the condition. As most of the causes of EPT are treatable and/or reversible, it is believed that it can be corrected for many causes.
Pathophysiology
EPT relies on the same physiologic mechanism as normal PT, which mainly comprises peripheral mechanisms (mechanical properties of body segments and stretch reflex) and—in less than 10% of subjects—a central component with oscillations around 8 to 10Hz (see Fig. 27.1).
Etiology
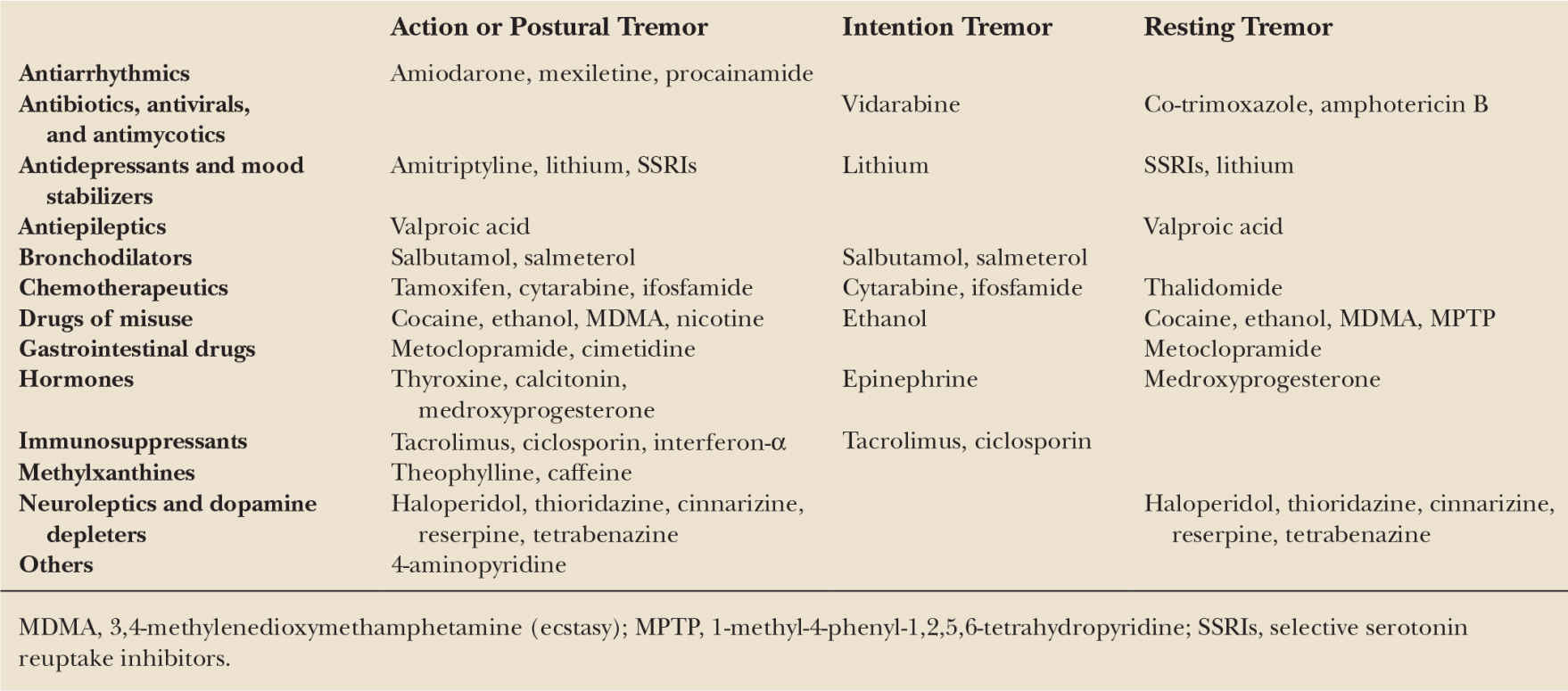
Table 27.4 lists the causes of EPT, the majority of which are related to drugs or toxins enhancing the peripheral or the central component of PT (Table 27.5).
Treatment
Depending on the etiology, a causative treatment is always the first step. The short-lived emotional trembling in certain situations requires only rarely treatment. A single dose of a β-blocking agent (e.g., propranolol 30–100 mg) just before a stressful situation can usually help to suppress this transient tremor that may interfere with important (e.g., professional) functions. Other β-blockers (atenolol <200 mg daily), metoprolol (<200 mg), acebutolol (<400 mg), oxprenolol (<160 mg), nadolol (<80 mg), and molol (<20 mg), have a similar effect. Propranolol improves the tremor of ophthalmic surgeons when given prior to surgery (125). Treatment of thyrotoxic tremor is recommended with propranolol (<160 mg).
| Causes of Enhanced Physiologic Tremor |
• Drugs (see Table 27.5)
• Toxins (mercury, lead, manganese, alcohol, DDT, lindan)
• Metabolic disturbances (hyperthyroidism, hyperparathyroidism, hypoglycemia, hepatic encephalopathy, magnesium deficiency, hypocalcaemia, hyponatremia)
• Others (anxiety, fatigue, hypothermia, sleep deprivation, sympathetic reflex dystrophy, withdrawal of alcohol or drugs)
DYSTONIC TREMOR
Different forms of tremor can be associated with dystonia (see Table 27.2). Typical dystonic tremor (DT) occurs in the body region affected by dystonia; typical examples are head tremor in torticollis, hand tremor in writer’s cramp, or jaw tremor in orofacial dystonias (126). It is defined as a postural/kinetic tremor usually not seen during complete rest (127). Usually, these are focal tremors with irregular amplitudes and variable frequencies (mostly below 7 Hz). Some patients exhibit focal tremors even without overt signs of dystonia (128), thus challenging the diagnostic abilities of neurologists, especially when the tremor is present at rest. These patients are often diagnosed with PD but then found with no progression and normal DAT-SPECT (SWEDD: subjects without evidence of dopaminergic deficit) (129).
In many patients with DT, antagonistic gestures lead to a reduction of the tremor amplitude. This is well-known for dystonic head tremor in the setting of spasmodic torticollis. A reduction in tremor is seen when the patient touches the head or only lifts the arm (130). The effect of these maneuvers can sometimes be difficult to observe clinically, and it can be helpful to record surface EMG from the affected muscles and look for EMG suppression (130). Particular types of DT are probably the task/position-specific tremors and “thalamic tremor,” when a thalami lesion induces also a dystonic posturing (see Holmes’s tremor). This tremor is part of a specific dystonia–athetosis–chorea–action tremor following lateral–posterior thalamic strokes (131,132). In the setting of a well-recovered severe hemiparesis, the combination of tremor with an intentional component, dystonia, and a severe sensory loss seems to be the important clue for the diagnosis together with this stroke. Proximal segments are often involved.
Tremor associated with dystonia (TAD) is a more generalized form of tremor in extremities that are not affected by the dystonia. This is a relatively symmetric, postural, and kinetic tremor usually showing higher frequencies than actual DT, often seen in the upper limbs in patients with spasmodic torticollis (133). This tremor might respond to drugs used for ET and might be present in absence of overt sign of dystonia, typically in pedigrees of dystonic patients (“tremor associated with the dystonia gene”). These “ET-like” tremors further complicate the nosology of ET, since many authors erroneously include ET among the expression of dystonia (e.g., in the context of genetic studies). Recently, isolated jaw tremor in patients affected by dystonia not involving facial muscles has been included in this type of tremor (126).
Epidemiology
The prevalence of DT was found to be between 17% (134) and 55% (135) in adult-onset primary dystonia, and 20% in an unselected group of dystonia patients (136). The proportion seems not to differ between primary and secondary dystonia but seems to be more common in cervical dystonia than other locations (134,137). In a large survey among patients from a large Indian movement disorder center, DT constituted for about 20% of all patients presenting with nonparkinsonian and noncerebellar/ET tremor (138).
Pathophysiology and Etiology
DT is still debated as a separate entity and different definitions have been proposed by clinicians (139–141). Virtually, every dystonic syndrome may present with DT.
The pathophysiology of DT is largely unknown but likely related to the CNS (especially basal ganglia) abnormality postulated for dystonia itself (127). TAD was considered a forme fruste of ET (140). However, it is not yet clear if they share common genes, and the pathophysiologic mechanisms seem to be different in some of the patients (15,133). During ballistic wrist flexion movements, the latency of the second agonist EMG burst was later in ET than patients with tremor associated with cervical dystonia (133). Reciprocal inhibition between forearm muscles differed in patients with tremor preceding torticollis or when tremor started simultaneously with torticollis (133). As patients with prominent tremor may develop dystonia, only late additional tests are needed. Preliminary data suggest that thresholds for temporal discrimination movement might provide such a test (15). DT showed abnormal thickening of the left sensorimotor cortex in DT (142).
Treatment
There is a paucity of information about the treatment of the DT syndromes. Several drugs (including anticholinergics, tetrabenazine, benzodiazepines) have been tried with inconstant results (for drug dosages, see Table 27.3). A recent systemic review on 487 patients published in 43 papers found that treatment outcome is highly variable, depending on the specific type of intervention and tremor distribution. Drug efficacy is generally disappointing, and a moderate effect is only found with anticholinergics, tetrabenazine, clonazepam, β-blockers, and primidone (143). Levodopa (L-dopa) is only efficacious on tremor due to dopa-responsive dystonia and can sometimes worsen the tremor (129,144). The largest amount of data was available for BoNT injections, which provided a marked improvement, particularly for the management of midline tremors (head or vocal cords) (143,145). TAD is often responding to the medication for classical ET.
Severe cases in the setting of a generalized dystonia have been successfully treated with DBS of the globus pallidus pars interna (Gpi) (146). Stimulation of Vim can also alleviate the tremor drastically but can occasionally lead to worsening of the dystonia itself. Considering the potential worsening of other dystonic features, the suggested target might be the GPi.
Bilateral subthalamic nucleus (STN) DBS has been reported to improve cervical dystonia, dystonic head tremor, and ET-like tremor of the hands in one patient (147). Others reported that DBS of the subthalamic white matter, including the Zi, remarkably improved proximal DT that had been refractory to Vim thalamotomy (148).
PRIMARY WRITING TREMOR AND OTHER TASK-SPECIFIC TREMORS
Primary writing tremor (PWT) is a condition in which tremor predominantly or only occurs during writing (149). No other neurologic signs are evident except for a slight postural and terminal intention tremor. PWT can be task-induced (type A) or position-sensitive (type B).
The epidemiology and the natural course of PWT are not well-known. Age at onset is variable, and even cases presenting during childhood have been reported; the disorder begins slowly, progresses for years, and becomes stabilized (150). Some patients report that at onset, they only had difficulties with specific letters, their condition might progress in terms of severity, topography (also involving the nondominant side), and type of tremor (becoming a resting/action tremor) (151). Familial history is generally negative.
PWT is the most common variant among many task-specific tremors frequently associated with specialist motor skill, like the musician tremor or golfer tremor.
Pathophysiology and Etiology
PWT is considered to be a focal task-specific tremor, which has been classified as among the ET syndromes, a form of focal dystonia, both, or neither (152,153). Although it resembles ET (where tremor is present on action, on maintenance of a posture, and may affect hand writing), its focal task-specific nature, the lack of response to propranolol, and a well-documented effect of central cholinergic drugs (150) have suggested that PWT may be more closely related to focal dystonia than ET (152,153). Abnormal coactivation of antagonist muscles on EMG recording has been used to support this claim. PWT is, however, distinguished from focal task-specific dystonia (writer’s cramp) by the lack of excessive overflow of EMG activity into the proximal musculature and abnormal reciprocal inhibition of the median nerve H-reflex on radial nerve stimulation (154,155).
Treatment
No double-blind studies of the condition are available. Propranolol, primidone, L-dopa, and neuroleptics were not effective. Anticholinergics, when tolerated, may have a role (143,150). Studies are available on the use of BoNT and were reported to be successful (143,156). Notwithstanding, treatment of PWT is often ineffective. The disability caused by this condition can vary from mild to considerable, depending on the profession of the patient. The handicap that it produces in Western cultures is not considered sufficient to merit the risks involved in stereotactic surgery. However, in Japan where calligraphy is an important occupation, thalamotomy has been successfully performed for this condition, as it can threaten the professional career of the patient (157). Successful Vim DBS procedures have been reported (158
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree