7 Examination This chapter details the examination process of the Neuro-Developmental Treatment (NDT) Practice Model. Emphasis is on the observations, handling, and clinical hypothesis generation that the NDT clinician organizes for the purpose of understanding how clients function and move the way they do. Examination is described as clinical observation, handling, and testing. Posture and movement are described and explained as multisystem body functions that affect participation and activity. The chapter includes a detailed review of body systems that the clinician using the NDT Practice Model examines, with current research information about each system. Learning Objectives Upon completing this chapter the novice clinician will be able to do the following: • List and define the different components of an NDT examination. • List at least three different purposes of examination and explain how the structure of an examination varies according to those three purposes. • Explain why information gathering, examination, and evaluation are interwoven and interdependent in the NDT Practice Model. • Explain the process of individualized examination according to the desired functional outcomes anticipated for a client. • Define at least eight reasons why a clinician uses handling in the NDT examination. • Describe the difference between a multisystem integrity/impairment and a single-system integrity/impairment. • Define posture and movement and then be able to create a list of posture and movement impairments for clients examined in daily practice. • List at least eight single body systems’ structure and function characteristics. Upon completing this chapter the experienced clinician will be able to do the following: • Generate questions and comments with clients and their families during examination, the answers to which provide direction to further individualize the examination. • Immediately use examination information to generate hypotheses about multiple influences on a client’s participation and activity. • Generate hypotheses about how the structure and function of single body systems interact with each other to produce multisystem functioning in clients. • Generate hypotheses about the contributions of single systems and personal and environmental contexts to a client’s multisystem integrities and impairments not detailed in this chapter, such as learned disuse, fear, and pain. Examination involves systematically gathering observations and measurements of the client in all International Classification of Functioning, Disability and Health (ICF) domains: participation, activity, and body systems. The Neuro-Developmental Treatment (NDT) clinician organizes the examination based on these domains, as well as on the particulars of the information gathering previously described. This examination provides information that the clinician will use to seek an understanding of relationships among the domains during the evaluation portion of practice (Fig. 7.1). Where and how should the clinician begin examination? The NDT clinician starts with function, or observations of participation and activity. What can the client do today? Then the clinician begins to ask How? How does the client do what he or she does? How leads to examination of participation and activity, then to examination of multisystem structures and functions, such as posture and movement. Examination includes the environmental and personal contextual factors in which participation, activity, and posture and movement usually occur for that client. Finally, the clinician examines the contributions of body systems specific to the client’s functional abilities and inabilities. This structure leads the NDT clinician to an individualized organization of the examination with flexibility that meets the needs of each client. How will later lead to why during evaluation once the clinician gathers data from the entire examination. There is no official NDT examination format. Each clinician, working with each client and family under particular advantages and constraints, structures an examination that fits the context of the situation. Examination may serve different purposes. Sometimes, an examination is a screening for further examination or referral to another agency, such as when clients attend specialty clinics (e.g., a spasticity clinic). An examination may serve the purpose of qualifying a client for services, such as special education, Medicare-approved visits, placement in a skilled nursing facility, or early intervention. These types of examinations are therefore specific to the criteria for qualification for services and are often limited in scope. A large part of practice for many clinicians consists of performing in-depth examinations with recommendations for intervention (episodes of care). Examination is detailed in this situation and is shaped by the environment where subsequent intervention management will occur, such as in the home, or in a school, rehabilitation center, or long-term care facility. These considerations affect the emphasis of what is examined under particular conditions. For example, a school therapist who will implement an individualized educational plan (IEP) along with other professionals considers the functional outcomes that are most necessary for a child to succeed in a particular classroom at a particular school with particular teachers. The examination may therefore begin with observing functions the child can and cannot perform in the classroom, cafeteria, or gym class and at recess. A therapist working in home health care with a retired mechanic who had a stroke structures the examination around functioning the client can and cannot perform within the home and in excursions from home to other places in the immediate area and community, focusing on the relatively new retirement routine the man had begun to establish. If this man had recently taken up a gardening hobby, the therapist will examine his ability to tend to the garden as well as examine function in the basic daily routine. Because there are many purposes and environments for examinations, clinicians and facilities tend to develop their own formats and forms to suit their needs. The clinician using NDT may work within these formats and specific forms to create an examination that allows for observation and measurement of participation, activity, multisystem structures and functions, and single-system structures and functions. This chapter therefore presents comprehensive examination strategies that each clinician will then tailor to each client’s situation. What should be examined? Should every body structure and function be examined and measured? As the reader will soon discover with the review of systems in this chapter, examining each one of them, thoroughly measuring each category in each system, would require an inordinate amount of time, as well as exhaustive work for both client and clinician. Therefore, the clinician streamlines and customizes examination based on the initial interview and observations. Prior to examination, the clinician has seen and heard the concerns of the client/family, observed posture and movement within some activities, and asked the client and family to state their goals for intervention. All of this information determines what the clinician will emphasize in examination and helps to prioritize what will be examined in detail. During the initial portion of the examination, the clinician observes function. For example, the case report of Perry in Unit V (B3) of this text describes him as a 9-month-old boy with left hemiplegia due to right middle cerebral artery infarct (Fig. 7.2). He lives with his parents and two older siblings. Perry gestures for communication and uses his right arm, but not his left, in play. His mother says that he is able to sit in a high chair and is carried for mobility. He attends an infant/parent group at a university setting with his mother. Perry’s examiner notes that he makes no transitional movements between positions (supine or prone to sit, up and down from standing), refuses to move away from his mother, and cries when the examiner tries to encourage him to use his left hand in play. His mother can place him in sitting, and he grasps toys using only his right hand as he sits. He takes weight through both legs when held in a standing position. With only a sample of Perry’s participation and activities and a few observations of his posture and movement skills, the clinician examining Perry questions why he does not move between postures, why he does not use his left hand, and why he cries when the examiner touches his left hand. The examiner may or may not be concerned about Perry’s unwillingness to separate from his mother. (Developmentally, 9-month-olds frequently show reluctance to separate, and this could be a sign of Perry’s appropriate cognitive and social awareness. Furthermore, the examiner is a new person to Perry, and he may be appropriately wary of new people.) The examiner discusses with Perry’s mother her priorities and global goals for intervention. Fig. 7.2 Perry at 4 months of age. Although this picture shows asymmetry of his cervical and upper extremity posture, Perry’s therapist observes him in various postures and positions under different contexts (held by his mother, placed on the floor, sitting on his mother’s lap, standing with support) to note whether this position persists or whether he has more variety to his postures. The examiner will try to engage Perry, perhaps through play with his mother, to determine if he shows any more postures and movements not seen so far. The examiner would like to place her hands on Perry but knows he may react adversely and so may choose not to do this at first, saving handling until rapport is established, or touching Perry only briefly in playful activity. This strategy is used because the examiner knows that establishing rapport, even if the first few sessions do not yield as much information as the examiner would like, is important for the long-term relationship with Perry and his family. The examiner observes Perry’s posture and movement, including alignment, symmetry/asymmetry; responses to the environment; and interaction with his mother. The examiner will attempt interaction with Perry, offering him toys or giving them to his mother for them to play with. The examiner continues to watch, listen, and ask questions about Perry’s abilities in function in the context of his life. With this work, the clinician begins to formulate clinical hypotheses about why Perry functions as he does. Is his nonuse of the left hand likely due to muscle activity imbalance, sensory sensitivities or ineffective processing of sensory information, lack of postural stability in the trunk and left shoulder for which he compensates by increasing distal muscle contraction, or loss of joint mobility? The clinician continues to observe and consider these options, perhaps adding more options or beginning to prioritize which she or he thinks are more likely. At this point, the examiner may suspect neuromuscular and sensory impairments as the most likely systems interfering with function for Perry and will examine these through handling when possible, to feel muscle activity and tension, assess how easily Perry changes muscle activity, and gauge how he responds to various types of touch. Opportunities and needs to examine other systems will evolve as the clinician begins to work with Perry. The clinician chooses the systems to examine based on a knowledge of stroke pathology in infancy; the knowledge of sensorimotor, cognitive, and social development and how Perry is faring in his development; observations of Perry’s posture and movement; and Perry’s mother’s descriptions of what he can and cannot do. The examination is therefore focused and customized for Perry. As shown in the example of Perry, observation during examination starts with observations of activity (functional skills) and any participation that is possible in the examination setting. The skills observed spontaneously and by request will vary according to the profession of the clinician performing the examination and the setting (e.g., home, school, outpatient rehabilitation center, long-term residential center, etc.), but these are usually the easiest and most spontaneous domains to observe in any examination session. The clinician begins by recording activities and participation the client can perform, tries to perform but cannot complete, and cannot perform at all. Activities and participation are also the domains that the client and family know about in detail, so beginning with these aspects can be empowering to them; they find that they can question, comment on, and demonstrate these domains confidently, and they remind the clinician that participation and activity occur in a variety of contexts (see Chapter 6, Information Gathering). Rapport and trust building are therefore encouraged, and the examination is truly a team effort. For example, an SLP may examine the activities of communication and speech, observing the variety of successful and less successful abilities of a client in the examination setting. The SLP will observe how the client produces any sounds or gestures or otherwise communicates to others and will note the contexts under which the communication takes place, specifically observing the variety of postures and movements the client achieves. An SLP examining a 2-year-old may start with trust building among the parent, child, and SLP by engaging the child in activities the parent mentioned were favorite activities. The SLP observes a range of information as the child plays and interacts with the parent and therapist. The SLP notes the various ways the child communicates with parent, therapist, and the environment, using spontaneous gestures, vocalizations, and verbalizations. Then the SLP notes postures and movements available to the child for this interaction: respiratory pattern, depth, endurance, and coordination with swallowing and voicing; arousal and attention span; preferences and variety of play; and interaction skills. This list is not exhaustive. During this observation, the SLP begins to hypothesize about how to structure the handling portion of the examination and which tests and measures would be the most appropriate for this child. The SLP may wonder, “If the child’s postural and respiratory muscles were more actively sustained in contraction when she voices, could she vary the pitch and loudness of her speech or say more words per breath?” Then during the handling portion of the examination, the SLP could support trunk position and posture, including rib cage support, to note the effect on respirations and voicing. The SLP might elongate the pectoral muscles to enable more thoracic extension for posture and position of the trunk, noting the effects on the quality and quantity of speech production. The SLP may leave her hands in full contact with the trunk, waiting until the child voices to note what segment of the body or muscle groups the child uses to initiate voicing. The observations of activity directed the SLP in specific handling choices and will direct the choices of tests and measures too. Although the SLP may have preselected a language test based on the child’s age, she may decide that other tests that measure the same domain may be more appropriate because the child has more or fewer capabilities than most children her age. The foregoing example demonstrates how observation and measurement of participation and activity lead the clinician to select which multisystem and single-system body structures and functions to focus on first in examination. The clinician asks, “What can this client do and not do? What postures and movements do I observe this person using to perform participation and activities? Which single-system body structures and functions probably contribute to these postures and movements that I should test? Which test or measure would be the most appropriate to gain this information?” Finally, our current understanding of motor control and motor learning (see Chapters 12 and 13) shows that posture and movement selection, along with all of the supporting contextual factors, is organized around a functional task. The clinician using NDT will therefore examine postures and movements within the context of functions and will later design intervention around functional outcomes (see Chapter 9 on session intervention). In summary, in any examination situation, the client, family, and clinicians all have roles to perform during information gathering and observation. Examination in NDT continues as multidirectional communication with all participants. The client reports and demonstrates participation and activity (function), both spontaneously and by request. The client, family, and other caregivers ask questions of the therapist and offer further information as they demonstrate skills. For example, a client may say, “I can walk on the kitchen hardwood floor like I’m doing it here, but our bedroom carpet is so thick that I often trip and I’m afraid I’ll fall.” Or, “When I feed her formula out of the bottle, she drinks like you see her doing now, but after about two minutes she seems to get so tired that she can’t suck any more out of this nipple. I wonder if another type of nipple would work better.” The last statement is a hypothesis that the family generated based on their description of how their infant bottle-feeds. Baseline observation of participation, activity, and body system functions initially requires hands-off as much as possible, and information-gathering questions will continue to be generated as the clinician performs the examination. The clinician observes spontaneous activities, postures, and movements. The clinician may request that the client, or client and family together, demonstrate a particular activity, posture, or movement that the clinician has not yet seen the client perform. Once satisfied that the client has demonstrated a good sample of the repertoire of each ICF domain, the NDT clinician begins hypothesizing about why some functions, postures, and movements cannot be completed or are completed inefficiently. The clinician begins hands-on handling of the client to examine muscle activity, respirations, structure of the musculoskeletal system, and responses to the sensory input of the handling. The clinician also examines how easily the client changes muscle activity, sensory organization and responses, arousal/attention, behavioral organization, posture, movement, alignment, and range of motion to specific handling strategies. This information assists the clinician in determining how the client changes and adapts. Thus it ultimately affects outcome setting. Handling involves placing the hands (and sometimes forearms or segments of the trunk and lower extremities) in physical contact with the client to sense the following: • Muscle initiation and how long the muscle stays in contraction. • How many muscles contract together and the order of recruitment. • Stiffness and compliance of body segments. • Joint stability/instability. • Reactions to graded support of a body segment. • Active weight shifting initiated by the client, which assists in determining which muscles and body segments participate. • Sensitivity and reactivity to tactile and deep-pressure contact. • Respiratory pattern, timing, and rate. • The speed and ease (or difficulty) of change in any of the above—this information will be used when setting functional outcomes. For example, a clinician handles the trunk and shoulder complex of a client poststroke. She notes the tension in various muscle groups. She supports the trunk to assist posture and notes if the client is able to control more stability and movement options in the shoulder complex of the involved arm with this minimal postural support. This information assists the clinician in determining how quickly she thinks the client will be able to achieve functional outcomes, such as picking up the newspaper from the bedside tray table or using a fork to eat dinner. After observation and handling for examination, the clinician selects specific tests to measure the domains of human functioning. The clinician chooses these measures carefully based on the domains the test is designed to measure. Many times, the clinician needs to measure participation and participation restrictions, activities and activity limitations, and body system integrities and impairments. Tests are designed to measure one or more of these areas, and it is the clinician’s responsibility to select appropriate measures. For example, handheld dynamometers measure force production. This is a measure of body structure and function integrity/impairment. The results of this test indicate strength and duration of strength, but they do not measure activity or participation. A dynamometer will not measure a client’s ability to feed himself dinner. This example seems obvious, but clinicians may not always think about choosing a test to measure specific domains. For this reason, the clinician must understand the validity of a test (the test measures what it is supposed to measure, and the clinician understands what the test is supposed to measure) and the domain of human functioning the test was designed to measure. Clinicians who work with clients with neurodisabilities often select several tests to measure each of the three domains of human functioning (according to the ICF). Table 7.1 gives examples of tests a PT who examines an adult client poststroke may select. An OT working with a 7-year-old with cerebral palsy (CP) at her school selects testing shown in Table 7.2. An SLP examining a teenager post–traumatic brain injury (TBI) selects the following test items shown in Table 7.3. According to the ICF model, impairments in single systems and multisystem impairments, such as absent or delayed balance, ineffective posture and movement, apraxia or dyspraxia, fear, and pain, are all categorized under the Body Structure and Function domain. However, clinicians using the NDT Practice Model perform a detailed analysis of multisystems because they involve the interaction of many single body systems and contextual factors. To sort out the contributions of single systems and the interaction of these systems as they relate to participation and activity, these multisystem impairments must be thoroughly analyzed to effectively manage clients. Posture and movement as multisystem integrities/impairments are considered first.
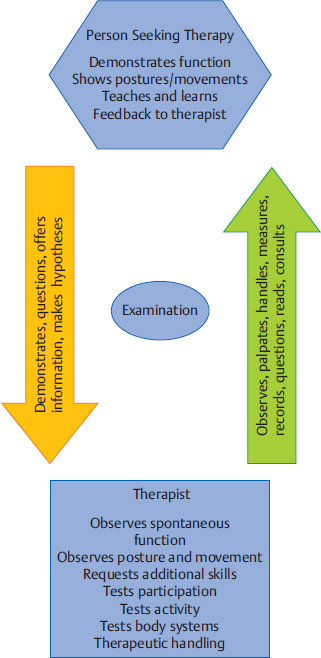
7.1 Examination Using the Neuro-Developmental Treatment Practice Model
7.1.1 The Purpose of Examination
7.1.2 The Roles of the Clinician and Client/Family in Examination
7.1.3 Examination: An Overview
Observation
Therapeutic Handling
Standardized and Nonstandardized Testing
Examining the Interaction of System Integrities and Impairments within the Context of Participation and Activity: Posture and Movement
ICF domain | Tests (examples) |
Participation | Stroke Impact Scale |
Activity | Timed Up and Go |
Body structure/function | • Gait and observational movement analysis • Modified Ashworth Scale • Fugl–Meyer: LE • Berg Balance Scale |
Table 7.2 The tests that an occupational therapist testing a child at school may select
ICF domain | Tests (examples) |
Participation | School Function Assessment |
Activity | Manual Ability Classification System |
Body structure/function | Posture and movement observation and handling; Sensory Profile; goniometric measures of passive range of motion (PROM) |
Table 7.3 Examples of tests a speech-language therapist might use with a teenager posttraumatic brain injury
International Classification of Functioning, Disability and Health domain | Tests (examples) |
Participation | Functional Independence |
Activity | Comprehensive Assessment of Spoken Language (CASL); Test of Early Communication and Emerging Language (TECEL) |
Body structure/function | Posture and movement observation; respiratory pattern, rate, endurance, coordination with voicing and swallowing; oral examination of motor abilities and sensory reception; Rancho Los Amigos Scale (cognitive functioning) |
Posture
Posture refers to alignment of body segments, the positions of those segments, and the relationship of body segment positions to each other.1 Therapists are interested in the characteristics of this multisystem function. Active posture encompasses postural tone and postural control (orientation, alignment, symmetry, weight shifting, and balance).
Postural Tone
Often, when PTs, OTs, and SLPs talk about muscle tone, they are referring to dynamic posture and movement. The Bobaths defined normal muscle tonus as “sufficiently high to give proper support tonus, but low enough to permit movement.”2 Their definition is akin to current definitions of postural tone. Shumway-Cook and Woollacott3 refer to the readiness to contract muscles in quiet stance as postural tone, whereas Smith et al4 use the term to mean muscular tension used to hold alignment in various positions. Gurfinkel et al5 correlated electromyographic (EMG) activity in trunk musculature to torque during slow movements in very small degrees of rotation to avoid stretch reflexes and biomechanical influences, showing that muscle activity produces resistance to the imposed torque. They referred to this active resistance as postural tone, and it measured higher in trunk musculature relative to the active resistance of similar imposed motions of the neck or hips in adults without disability. Years prior to this study, the Bobaths focused on postural control and adaptations in their descriptions of CP and stroke. They viewed postural adaptations as “provid[ing] the constantly changing background for every movement.”2
Historically, the term postural tone was used to describe the big picture of neuromuscular activity that contributed to antigravity control. Clinicians noted stereotypic, predictable, and limited repertoires in movement patterns in clients with stroke, TBI, and CP and referred to this collection of movement patterns as tone. However, this labeling did not direct the clinician to examine the possible components of tone.
Currently, the term postural tone encompasses a multisystem phenomenon of change in muscle activity to maintain the body upright against gravity.3 All sensory systems, body segment alignment, muscle length and fatigue levels, muscle morphology, emotions, attention, and nervous system structure and functioning influence postural tone. Researchers study the relationships of the many systems contributing to postural tone with the hope that understanding this multisystem phenomenon may assist in a better understanding of the mechanisms of neural activity regulated by the central nervous system (CNS), including reflexive muscle tone.5
Research has shown a relationship between abnormal passive muscle reflex activity (muscle tone) and mechanical and morphological changes in muscle,6,7,8,9,10 thereby suggesting that expression of muscle tone itself could be a multisystem phenomenon, just as postural tone is. Its neurological and biomechanical components are difficult to examine clinically with passive movements testing, even when consistent body and joint positions are ensured; several consistent velocities of passive movement are repeated in testing; consistent environmental conditions are ensured; and consistent client cooperation/relaxation is attained. As clinicians using the NDT Practice Model examine, evaluate, intervene, and constantly assess the outcomes of intervention, they can provide clinical insights to researchers and other clinicians about the complexity of muscle tone that may lead to new questions about this phenomenon.
Postural Control
Postural control and movement were introduced in Chapter 3 as multisystem body structure and function. Postural control orients a person with the head vertical and the eyes horizontal to the external environment. Postural control is a complex skill that relies on the interactions of multiple body systems.11,12 These systems include biomechanical constraints, movement strategies, sensory strategies (somatosensory, visual, and vestibular), perception of an upright position, control of dynamics (center of mass changes), cognitive processing, and the environmental context. Motor expression through CNS output to the musculoskeletal system is adjusted to contextual conditions through sensory input and perceptual processing.13 In addition to orientation, postural control includes balance. Postural control develops during human development gradually, as neuromuscular coordination and balance control become more skilled.14 The Bobaths stated as early as 1964, “Postural changes not only accompany a movement but also precede it.”2
Postural Control: Orientation
Postural orientation is one of two functions of postural control. This multisystem function includes alignment of the trunk and head with respect to gravity and support surfaces, the visual environment, vestibular structure and function, proprioception (especially from the head and neck), and internal body referencing (interoception).11,15
In a study on reaching skills, typically developing babies first gained head and gaze stabilization as a frame of reference for reaching, followed by successful reach and grasp movements, and eventually achieved multijoint coordination by age 15 months.14 Reaching skills were first referenced relative to a support surface. Roncesvalles et al14 hypothesize that the trunk is the first body segment reference for orientation in reach, followed by gravitational referencing in older children (ages 7–9), similar to that of adults.
Contraversive pushing after stroke is hypothesized to challenge gravitational orientation to posture primarily in the frontal (coronal) plane (Fig. 7.3).16,17,18 Researchers are searching for networks in the human body that receive and process graviceptive information. Karnath16 also proposes that the spatial neglect seen in other patients poststroke represents damage to networks that perceive and adjust body position and awareness in the transverse plane. Still other patients poststroke diagnosed with visuospatial impairments have shown that they misperceived vertical orientation in the sagittal and frontal planes compared with controls and that their errors were statistically significant.12
Postural Control: Alignment
Postural alignment is a part of orientation and balance and refers to the relationship of one body segment with another or of the position of the entire body to the base of support.3 Postural alignment contributes to the selection of movements a person makes to change position. Postural alignment also refers to joint angular measurement and its deviation from a predetermined neutral position.19 Joint angle neutral positions would need to be determined for a particular position of the body and would be based on age, functional task, and context for any research study examining alignment.
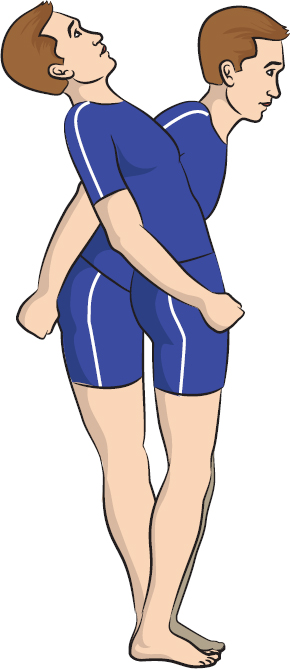
Alignment for posture and movement depends on more than the integrities or impairments of the musculoskeletal system that affect muscle length and joint range of motion. Ineffective alignment may be assumed because of decreased muscle strength, delayed muscle onset latencies and decreased EMG amplitude, and sensory or perceptual impairments. In two studies of children with spastic diplegic CP, Tomita et al20,21 hypothesize that any of these impairments may affect the standing alignment and characteristics of muscle activity (selection, latencies, and direction-specificity) during voluntary anterior and posterior sway control (Fig. 7.4).
Wilson Arboleda and Frederick22 hypothesize that malalignment of head and neck position in relation to the trunk and hip position affects the length–tension relationship of the muscles that elevate the larynx and consequently affect pitch control and resonance of voicing.
Fig. 7.3 Carol, a client poststroke with contraversive pushing who is described in Case Report A3 in Unit V, practices orienting her body with visual vertical. The therapist works with Carol with active postural control and movement as well as using visual environmental cues to orient her posture for functional skills, such as moving through her home.
Postural Control: Symmetry
Symmetry in posture and movement refers to the distribution of a person’s mass and pressure on a support surface and is considered to be one aspect of postural control.23 Although symmetry can be observed and measured in all three cardinal planes, most descriptions of symmetry and research examine the frontal plane (right/left symmetry).
Gait and single-leg balance studies in children and adults without impairments show slight asymmetries between right and left limbs; asymmetry is therefore considered to be an expected finding.24,25 However, studies that have analyzed more marked asymmetrical sitting and standing postures in people with neurological impairments are concerned with the inefficiency of postural adjustments or the initiation of movement and with fall risk when asymmetry of posture and movement affects balance responses.23,26,27
Fig. 7.4 This young man assumes a crouched alignment for standing. According to Tomita et al,20 crouch must be controlled largely by the quadriceps femoris muscles for the person to stand successfully. People who cannot control trunk and hip extension may rely primarily on these knee extensors to stand as they assume a crouched alignment. In another study, Tomita et al21 showed in one child with spastic diplegic cerebral palsy that training the trunk and hip extensors to control postural sway improved standing alignment for the child.
Clinicians are also concerned that marked asymmetry in any cardinal plane could increase the severity of body system impairments over time and limit function. Clients with CP who develop scoliosis or hip subluxation/dislocation may show asymmetrical weight bearing in sitting (Fig. 7.5) with a resultant poor ability to sit, even with custom-made adaptive seating.28,29,30 Scoliosis may continue to worsen after bone growth is complete.30
Asymmetry in upper extremity neuromuscular control, musculoskeletal structure and function, and sensation may interfere with upper extremity movements and the ability to use bimanual skills. In assessments of neonates poststroke, Guzzetta et al31 found a correlation between asymmetry of wrist movements and the developmental of hemiplegia at 3 months of age. Adults poststroke show alterations in bimanual coordination,32,33 which respond favorably to both unimanual and bimanual rehabilitation. Bimanual skill practice may access interhemispheric neural networks that unimanual activities do not.32
Postural Control: Weight Shifting
Weight shifting refers to the ability to redistribute body mass through muscle activity. Weight shifting is used both during active position changes and to recover balance. Clinicians are interested in efficiency of this weight redistribution and its safety. Weight shifting is performed in an infinite number of transitional movements from one position to another, and the clinician using NDT observes and handles the client to determine if the weight-shifting strategies a client uses are efficient and safe.
Strategies to gain and regain control of upright standing are the most frequently researched weight-shifting studies. Researchers and clinicians are interested in assisting clients to use successful weight-shifting strategies to recover posture during sway conditions to prevent falls.
Several common strategies in standing are used in children and adults with and without postural impairments. In many instances of postural sway, a combination of these strategies may be used:
• Trunk strategy: Trunk and limb movement in the transverse plane can be a part of weight shifting strategies in standing (Fig. 7.6). Trunk rotation may serve the purpose of reducing the sway at the ankle in standing sway34,35 and is used in people with and without neuromuscular impairments. Trunk and limb transverse plane strategies are coupled with strategies in the lower extremities.
Fig. 7.6 JW, who is described in Case Report A2 in Unit V, works with her therapist to incorporate trunk and hip rotation into her standing-balance and weight-shifting strategies.
• Hip strategy: Movement of the body’s center of mass occurs primarily at the hip in large, fast disturbances of posture (Fig. 7.7). Activity of the abdominals and quadriceps femoris muscles in forward sway and activity of the paraspinals and hamstrings in backward sway control posture to maintain upright.3,36 Hip strategies are used in adults and children, both with and without neuromuscular disabilities.3,36
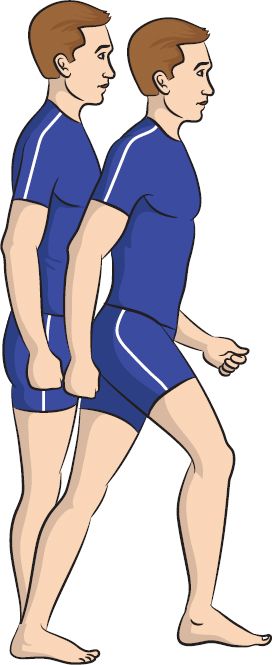
• Ankle strategy: Postural stability is controlled by movement primarily around the ankle joint. In people without neuromuscular impairments, it is the strategy most commonly used to respond to smaller and slower disturbances of posture.3 In people without neuromuscular impairments, the sequencing of muscle activity starts at the ankle and moves up (distal to proximal sequence) (Fig. 7.8). In forward sway, the gastrocnemius contracts first, then the hamstrings, then the paraspinals.3,36 With backward sway, the anterior tibialis is active first, then the quadriceps, then the abdominals.
• Change-in-support strategy: Changing the base of support under the body’s center of mass when standing—a stepping strategy—is a strategy to recover an upright position in fast, destabilizing conditions (Fig. 7.9).3,36 These strategies assist balance recovery as well as protect the body from injury. In the upper extremities, these types of strategies are referred to as protective extension strategies.
In studies with visually guided weight-shifting practice, adults without disability and adults poststroke have been able to improve the timing and effectiveness of postural sway to maintain an upright position,35,37,38,39,40 although more time may be needed to complete the strategy in those poststroke. School-aged, ambulatory children with CP have showed improvement in their speed of muscle-contraction onset and muscle-activation organization, and reduced muscle coactivity during postural sway strategies with practice in reactive balance.41
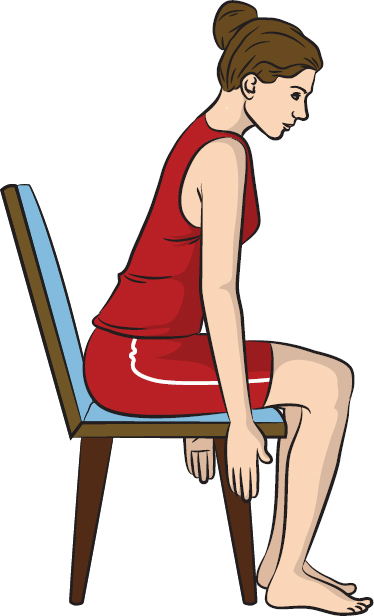
Sitting postural sway has also been studied, showing activity of the trunk and lower extremities when the person is swaying in the sagittal plane.36 In older children and adults, muscle activity includes extensor activity of the hips, trunk, and neck in forward sway with the anterior tibialis recruited in reaching if the feet are planted (Fig. 7.10). To reerect from the forward position, the gastrocnemius is recruited. In backward sway, the hip flexors, abdominals, and neck flexors are recruited (Fig. 7.11).
Postural Control: Balance
Balance is the ability to control the body’s center of mass within the base of support,3 taking into consideration that the base of support is often changing (dynamic balance). Balance requires the coordination of responses to all forces acting on the body to produce stability.11,42 These include external and internal forces, which require multisensory detection. Body systems that participate in balance include the biomechanics of the musculoskeletal system, all sensory systems, and many areas of organization in the CNS to produce precise motor responses while remaining flexible to changes in evolving movement.43,44
Balance, also known as postural stability,3 can be challenged in several ways42:
• Reactive balance occurs in response to external forces acting on the body, changing the base of support or disturbing the position of the center of mass. Sensory feedback is required to initiate the process of response. An example of reactive balance is the body’s response to being hit with an opening automatic door at the grocery store.
• Anticipatory balance occurs in anticipation of internally generated destabilizing forces as a result of the body’s own movement. Postural adjustments occur prior to the initiation of a movement action to counteract expected perturbations to ensure stability.45,46 Experience refines this process, which relies on feed-forward to act. An example of anticipatory balance is the entire body’s motor activity prior to picking up a stack of books from the countertop.
• Adaptive balance allows changes in postural control as the task and environment change while posture and movement unfold. This type of balance requires continual and complex interactions among sensory systems, CNS processing, motor responses, and musculoskeletal alignment.44 An example of adaptive balance is the body’s ongoing changing motor activity when the individual is kicking a playground ball in a game of kickball.
Fig. 7.10 This woman uses extensor activity of the hips, trunk, and neck with feet pushing against the surface as she leans forward.
Balance can be examined using clinical standardized and nonstandardized tests, and the clinician ensures that all three types of balance are tested. Whereas researchers can use computerized posturography to objectively measure the postural sway during platform translations or rotation along with varying the sensory conditions surrounding the platform, the clinician usually relies on simpler tools to examine balance.
Balance requirements vary according to how large the base of support is (creeping on all fours vs. standing without support or standing independently vs. standing while holding onto a walker or cane) and how far the center of mass is from the base of support. The clinician therefore tests balance in the postures that the client typically uses in functional tasks and may challenge the client with postures that are unfamiliar.
Balance requires, in part, the ability to recruit direction-specific muscle groups to control body sway.47,48,49,50,51,52,53 Recruitment order of these muscles typically follows a developmental as well as a position and task-specific sequence. Under some conditions, people with various neuropathologies can show different recruitment order, more variability with repetitions of the same task, less flexibility in adjusting recruitment to specific tasks, and the use of altogether different muscles to attempt the same functions as people without neurodisabilities.20,47,53 Compare the alignment during postural sway in Fig. 7.12a, b.
One neural strategy to increase postural stability for control of balance is to coactivate muscles in various synergies or to coactivate producing cocontraction around a joint.54 This strategy is seen in people with and without neurodisabilities. The degree of coactivity distinguishes efficient from inefficient postural stability. Children with CP often show higher levels of coactivation when compared with children without disability.55,56
Adults poststroke have shown larger sway areas than controls without disability in sitting unsupported, with poor postural control of trunk musculature implicated.57
Brogren et al51 tested reactive balance in children ages 7 through 11 with spastic diplegic CP while they were seated on a movable platform (most were nonfunctional ambulators). The children recruited balance responses in a proximal to distal order similar to those seen by young children without disability and by adults without disability in unstable positions. The children with diplegia also often used coactivation of antagonistic muscles, perhaps as a way to provide greater stability.
Hadders-Algra et al48 studied babies ages 4 through 18 months with CP in sitting and lying down positions as they reached and therefore tested anticipatory postural reactions. They found that, although most of the babies could recruit basic postural organization, they had difficulty modulating that activity to the reaching task and tended to use excessive coactivation of antagonists.
Fig. 7.12 (a, b) As the young woman on the left leans forward, she is likely to recruit muscle activity distal to proximal, using gastrocsoleus, hamstrings and quadriceps coactivity, gluteals, and trunk extensors. The girl with spastic diplegia on the right may recruit activity primarily from her upper body first, then after a latency of a few milliseconds, recruit activity in the lower body. Note that, even if the same muscles are used to attempt postural control, the girl with diplegia will be using her muscles in different body segment alignment and may be using concentric contractions where eccentric are more effective and vice versa.
Woollacott and Shumway-Cook41 tested reactive balance in standing in children with spastic diplegia and spastic hemiplegia who could stand independently for at least 30 seconds, finding increased lengths of time compared with children without disability to recover balance due to delays in muscle contraction onset, recruitment of muscle activity proximal to distal, and increased coactivation of antagonistic muscles.
Ferdjallah et al34 found that in quiet standing with eyes-open and eyes-closed testing conditions, children ages 5 to 13 with spastic diplegic CP who were independently ambulatory used limb and trunk movements in the transverse plane to maintain balance rather than ankle dorsi-/plantar flexion and inversion/eversion. This strategy compensated for poor abilities to generate ankle movements. Children without disability used limb and trunk rotation only when there was excessive sway; their preferred strategy was ankle movement during small arcs of sway.
Tomita et al21 studied anticipatory balance in teenagers with spastic diplegia and children without disability as they stood and moved their arms. Both groups activated erector spinae and medial hamstrings prior to the anterior deltoid, although the EMG amplitudes were significantly smaller in the group with CP in the erector spinae and hamstrings while the peak arm acceleration showed no significant differences between groups. Center of pressure on the feet was more anterior in the initial standing position in the teens with CP, and their displacements were larger with reach.
Dickstein et al58 studied anticipatory balance in the trunk with limb flexion movements from an initial position of sitting with feet flat on the floor. Fifty people post–middle cerebral artery stroke and30 adults without disability were tested. Muscles on both the right and left sides of the trunk were active when a limb on either side of the body moved in both groups of participants. Results also showed reduced activation of the lateral latissimus dorsi and the external abdominal obliques on the hemiparetic side in those people poststroke when moving either the arm or the leg in flexion on either side of the body, with delayed onset of postural muscle activity.
In a pilot study with ambulatory veterans post–severe TBI in an inpatient rehabilitation center, Pickett et al44 used computerized posturography testing with force platforms while performing the six conditions of the Sensory Organization Test. Results showed primarily vestibular impairments related to balance impairments with vision used to compensate. Vestibular nerve shearing caused during blast injuries in this population may be a part of the pathology.
Movement
Movement is a multisystem body structure and function. Movement selection is shaped by the neuromuscular system, musculoskeletal system, sensory systems that provide feedforward and feedback, context (personal and environmental), and behavioral intentions.1,13 It is a response to input from various body systems1 and to environmental and personal contexts. Movement is controlled and coordinated in milliseconds through the integration of a body that responds, executes, interprets, and adjusts to continual feedback.1 The nervous system, musculoskeletal system, and all sensory and perceptual systems are a part of this integration, responding to contextual demands, growth, development, aging, and disease or disability. The cardiovascular, respiratory, and digestive systems provide nutrition and energy to allow movement to take place.
Development and control of movement are described in Chapters 12 and 14 on motor control and motor development in Unit III. The NDT clinician will consider these questions while observing movement and handling the client to note characteristics of movement:
• Are movement strategies selected that are safe and efficient and meet functional demands?
• Are graded movements available when needed—large and small movements, ballistic and targeted movements?
• Is movement generated along with active postural support? If postural control is ineffective, are movements that would be necessary to complete a task suppressed or exaggerated in attempts to substitute for postural control? (For example, the upper extremity may be held against the body in an effort to control the trunk in an upright position if the trunk and hip posture is ineffective; or the eyes, jaw, cervical, and lumbar extensors may act together to attempt to hold a person’s head erect if postural control is ineffective.)
• Can a client control and coordinate movement at multiple joints in the same limb (intralimb coordination) or between limbs and the trunk and head (interlimb coordination)?
• Are extraneous or involuntary movements present that contribute to ineffective or inefficient control and coordination?
• What contributes to movement dysfunction in the single systems—neuromuscular, musculoskeletal, all sensory systems, cognition, respirations, cardiovascular, digestive—for this client?
7.1.4 How Does the NDT Clinician Examine Posture and Movement?
• Visual observation: The clinician uses visual inspection to examine how the client organizes postures and movements. The clinician may decide that a video recording of the examination will assist because of the replay capabilities and the ability to play the recording on slower speeds.
The clinician observes how one segment of the body moves and what the rest of the body does to control posture and stability as that part moves. The clinician also observes consistency or inconsistency in repeat performances of postures and movements. The clinician notes how the client acts and reacts to naturally occurring changes in body position and environmental conditions (Fig. 7.13). For example, what happens to stance and walking control when the client encounters an uneven surface after walking on a smooth surface? What happens to oral motor control when the client attempts to eat a different texture of food? What happens when the next toy is bigger and heavier than the previous one?
• Palpation: The clinician places fingers over a muscle group to note activity during rest, posture, and movement (Fig. 7.14).
• Handling for examination: The clinician manually contacts a body segment to note when the segment is active, how long it is active, and which muscle groups are active as the client attempts posture and movement. The clinician may provide manual stability or correct alignment, adjust the base of support, and then observe how the client responds to these changes. The clinician may control certain body segments or joints to observe how the client adjusts posture and movement when there are fewer segments or joints for the client to control. The clinician may provide graded sensory input through handling to observe how the client responds. For example, an SLP may place firm pressure on the midline of the tongue with a gloved finger to observe whether the tongue can respond with a cupping shape.
• Standardized and nonstandardized testing: The NDT clinician may use standardized and nonstandardized testing to assess aspects of posture and movement. For example, there are several balance tests available for use in pediatric and adult populations with neurological impairments. The NDT clinician is cautious when interpreting results of these tests as they apply to intervention. For example, balance tests may not be able to predict under which contexts will balance responses fail, and they do not indicate which impairments are responsible for the failure or what strategies will be most effective in intervention.11
Fig. 7.13 As Mark, described in Case Report A1 in Unit V, lifts his left arm and shifts weight onto his left leg, he is able to lift his right leg in either a balance reaction or voluntarily to step.
Fig. 7.14 As Mark’s physical therapist asks him to reach with his right arm, she can palpate the musculature around the scapula to detect activity. She can also support and reposition his scapula as he moves his arm with her hand positioned this way.
7.1.5 Identifying Ineffective Postures and Movements
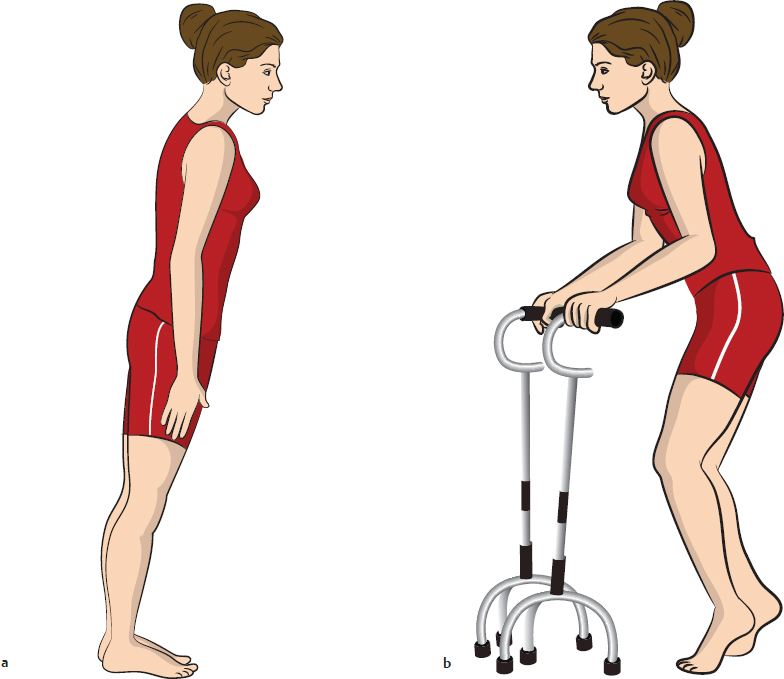
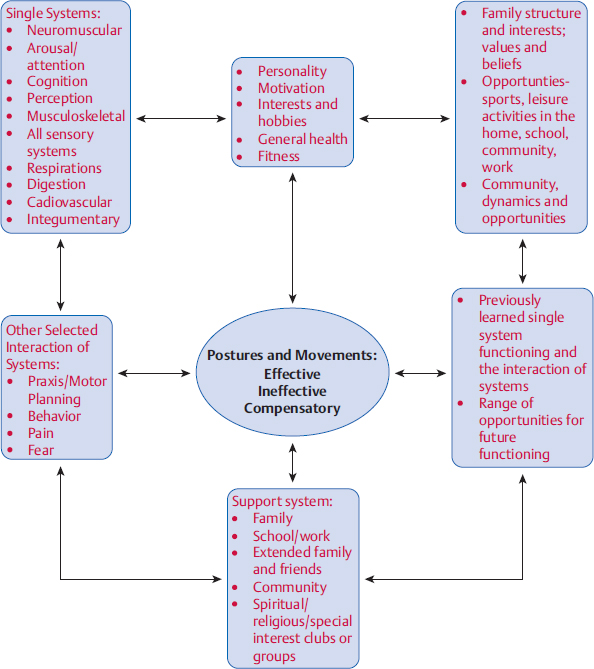
Recall the head control and knee hyperextension diagrams presented in Chapter 5. In viewing the diagrams of the head control and knee hyperextension postures and movements, we see the dynamics of many influences on activities (and the shaping of those activities into participation). Posture and movement are examples of the interaction of body systems (and within postural control are orientation, alignment, symmetry/asymmetry, weight shifting, and balance), but their expression and constant reshaping do not result simply from a combination of single-system structures and functions. The diagram in Fig. 7.15 includes many of the influences that shape expression of posture and movement at the moment and reshape it throughout a person’s life span.
7.1.6 Identifying Other Multisystem Body Functions: The Interaction of System Integrities and Impairments within the Context of Participation and Activity—Two Examples
Praxis and Motor Planning
Praxis, meaning action in a general sense, refers to the ability to do something, whether it is the practice of art, science, or movement skill. When used in the field of habilitation and rehabilitation, praxis refers to movement skills. Praxis is doing.59 Specifically, praxis describes goal-based purposeful and complex motor actions, including gestures and tool use.60,61,62,63 According to Sanger et al,61 examination of praxis needs to consider the following:
• The age of the person examined—the movement must be developmentally appropriate; in the case of an adult, a skill that has been learned, and in a child, one that should have been learned at that particular age.
• The person’s familiarity with the skill or gesture.
• That the movement was adequately explained or demonstrated to the person.
• That the person understood the verbal instructions or a demonstration of the movement.
• That the person possesses adequate muscle force, selective voluntary control, balance, endurance, and range of motion to perform the task.
• That the person is motivated to perform the task.
Praxis involves three processes, which are gleaned from the current literature only by reading about impairments in praxis.60,61,64,65,66,67,68,69 Although Ayres70 defined these processes many years ago, definitions of praxis are difficult to find in the current research literature. These processes are as follows:
Fig. 7.15 Posture and movement affect all aspects of a person’s life, and in turn, are affected by all aspects of a person.
1. Ideation: Conceptualization of the motor skill, gesture, or tool use; ideation involves cognition (working memory and goal selection), attention, and perception.
2. Planning:“Computing” the movement; the ability to initiate and sequence a task with anticipatory forces, the use of mental imagery to create an internal model of the movement, the ability to select salient sensory cues relevant to the task, the ability to scan for movement errors through the sensory systems and make adjustments through sensory feedback, the ability to predict body or body segment position at the end of the movement; all of these abilities are modified with practice and experience.
3. Movement execution: The selected postures and movements performed in a coordinated and efficient sequence specific to the task.
There is some inconsistency in terminology between praxis and motor planning within the literature. Motor planning is defined as the “ability to predict the future state of the motor system or the consequences of its action.”65 Crajé et al71 and Janssen and Steenbergen72 use a similar definition. In the praxis literature, no universal model differentiates between motor planning and praxis. Motor planning problems are defined as types of apraxias, and apraxias are referred to as motor planning impairments. Sometimes, planning seems to refer to the big picture of motor planning/praxis, and at other times, it is used in a more restricted sense to mean the second process of praxis.
The definitions of impairments in this multisystem function are more clear and consistent than the motor planning and praxis definitions. Apraxia is a term used for adults with lesions that disrupt praxis. Apraxia is a group of disorders of conceptualization, planning, and execution of learned, skilled movements, gestures (especially sequences of gestures), and/or tool use despite intact motor and sensory systems, comprehension, and cooperation.61,73,74,75
Apraxia is often categorized as ideational or ideomotor. Ideational (conceptual) apraxia is a failure to conceptualize the task automatically or on command either because the person no longer understands the act or cannot remember the idea of the task, especially a task with multiple steps (e.g., preparing a sandwich).67,73 A client with ideational apraxia may hold a comb and when asked to comb his hair, respond by placing the comb in his mouth or try to write with it. He may not be able to explain what a comb is used for. A client asked to prepare a sandwich may be able to open the bread wrapper, hold a knife and spread with it, pick up meat, and squeeze the mustard container (all motor execution), but he may spear the meat with the knife, fold the bread in half and lay it aside, or place the meat inside the bread wrapper.
Ideomotor apraxia describes impaired performance of a learned skill despite having sensory, motor, and language skills to perform the skill.73 The client can describe how a task is performed and can perform a task automatically but cannot perform the task on command, especially a multi-step task. A client with ideomotor apraxia may walk across the kitchen and place her plate in the dishwasher after dinner. However, if she is asked to pick up her plate, rinse it, and place it in the dishwasher, she will not be able to do so. When specifically asked to walk to the sink from the table, she may demonstrate an awkward gait pattern.
The lesions responsible for apraxia are often located in the parietal cortex, which has connections with the supplementary, premotor, and motor cortices.68,69,76 Lesions in the left hemisphere may cause more severe apraxias than lesions in the right hemisphere61,68,77 and may be seen with aphasia. Lesions in the cerebellum may also be implicated in motor planning impairments.66
Developmental dyspraxia is a term used to describe children with impairments similar to those of adults with apraxia63 who have difficulty using tools, sequencing gestures, and sequencing motor tasks without muscle weakness, sensory loss, incoordination, aphasia, or cognitive impairment.62,78,79,80 The lesions in dyspraxia are unknown but may be associated with early mild global cortical injury.61,81
Ayres,70 who first studied developmental dyspraxia, said that children with this disability know what they want to do but can’t do it. She emphasized that dyspraxia involves impairment(s) with ideation and planning separate from the motor execution of a task. She noted that children with CP may or may not have dyspraxia. To examine children with CP for dyspraxia, the clinician must be familiar with the motor control the child possesses and then examine praxis separately from motor execution.
Developmental dyspraxia has been studied in children with CP in those who are capable of producing the movements required for the task and who can complete standardized and nonstandardized tests.65,71,72,78,82 Researchers have been able to detect impairments in motor imagery,71 visual-spatial planning,65 anticipatory fingertip force planning,82,83 and unilateral and bilateral grasp.72 Most of the children in these studies were classified as spastic hemiplegic or diplegic.
Psychosocial Behavior State
Behavior refers to the actions and reactions of a person in response to both the internal and the external environment. In this section, the psychosocial aspects of behavior are considered as a multisystem phenomenon. Psychosocial interaction involves arousal, attention, motivation, goal-direction, sensory perception, and motor expression. Although it is beyond the scope of this text to discuss details of all of the contributions to psychosocial behavior, some these single systems that contribute to psychosocial behavior will be discussed.
Performance outcomes of clients depend not only on posture and movement but also on personal factors, the environment, and the neural substrates that control behavior. The clinician practicing with the NDT Practice Model values these factors just as much as the contributions of sensorimotor factors. Therefore, the NDT Practice Model includes examination of personal attributes and the environmental context of activity and participation. The clinician administers formal or informal questions or surveys about psychosocial functioning and requests and/or integrates plans from the professional evaluations of team members, such as neuropsychologists, teachers, vocational instructors, and guidance counselors. The clinician values formal and informal surveys that the client and family complete as part of the examination of all factors that influence activity and participation.
Research regarding motivation, self-worth, perceived competence, and externalized/internalized behavior expression has been studied in children with CP.84,85,86 These researchers often consider their conclusions to be preliminary and exploratory because research in this area is relatively recent. Schuengel et al,85 in surveying children with CP and their parents, found that their general sense of self-worth and perceived competence were similar to those of children without disabilities. Like children without disability, there was an association between those who reported lower perceived competence and self-worth and internalizing behaviors such as depression, anxiety, withdrawal, and somatization.
Sipal et al84 found that behavior impairments were higher in a group of children with CP ages 9 through 13 when compared with children without disabilities, but problems diminished over a 3-year period. Parents and care-givers rated each child’s behavior while a physician rated the severity of CP according to the Gross Motor Function Classification System. Family support and stress factors were related to behavior, while in turn, the children’s behavior was also found to affect the family environment. This relationship was similar to the relationships found in families with children without disabilities in other studies. There was a positive association of total behavior problems to the severity of CP and to level of pain.
Majnemer et al86 investigated motivational mastery (the intrinsic drive to attempt to master a skill that is at least moderately challenging). This motivation was viewed as related to personal beliefs about how well people perform and how much value is assigned to the task personally. Persevering when challenged was perceived to be based on past experience, current abilities, environmental context, and personal desire to achieve. Preliminary results suggest that children with CP may have lower motivational levels than peers without disabilities, and they were correlated to lower cognitive ability and motor function and to higher levels of perceived parental stress. Behavioral difficulties were correlated with lower motivation to persist as well.
Finset and Andersson87 compared coping styles for apathy and depression of student controls with people post-stroke and post-TBI. Using multivariate analyses, they found no association between coping strategies and lesion location in either experimental group. They concluded that there is a complex interplay between the lesion and psychological factors such as premorbid personality and coping repertoire.
Lack of motivation, or apathy, is common poststroke and may be associated with cognitive impairment, damage to some nuclei of the basal ganglia, and thalamic lesions.88
Aggression after TBI may be the most common behavior impairment, seen in all severity levels. In 208 patients with mild head injury in a study by Benedictus et al,89 one of three had behavior impairments, and these impairments were more prevalent than physical impairments in all severities. In the group with mild head injury, behavior impairments were important (along with cognitive impairments) in predicting return to work.
7.1.7 Examining Single-System Body Structures and Functions
Clinicians using the NDT Practice Model learn how to examine body system structures and functions in their academic education programs. The purpose of accredited academic programs is to prepare clinicians for general practice, and these programs have tremendous amounts of material for students to learn, so each body system cannot be covered in depth, especially with all of the pathologies a program must introduce. Clinicians in many related professions learn body system structure and function with various emphases, depending on each profession’s specialty. As clinicians who use the NDT Practice Model, we examine body systems within the confines of our professional practice acts and our academic preparation.
Because this text is written primarily for OTs, PTs, and SLPs who treat clients with neuromuscular diseases and disabilities, this section will describe single-system structure and function related to stroke, TBI, and CP. Ultimately, the clinician is responsible for using this information within the confines of professional practice acts and codes of ethics.
Neuromuscular System
Much of our knowledge about neuromuscular structure and function comes from experimental research studies that measure parameters of muscle tone, muscle recruitment activity, timing and sequencing, force production, and intra- and interlimb coordination with the aid of EMG and computer analysis.20,21,45,46,47,51,53,56,83,90,91,92,93,94,95,96,97,98 These studies increase a clinician’s descriptive knowledge of nervous system control and coordination, but they rarely add to procedural knowledge for clinical intervention.
Muscle Tone
The clinician uses consistent methods of testing, consistent joint position and alignment, consistent measurements in a variety of body positions, consistent environmental conditions, and a consistent definition of muscle tone that is written in the documentation to examine muscle tone. Standardized and nonstandardized clinical tests of normal and abnormal tone can be used. The clinician will be aware of the reliability and validity of these tests, their sensitivity, subjectivity versus objectivity of measurements, and their correlation to functional activity and participation.99,100,101