Case Report B5 Enhancing Functional Independence in a 10-Year-Old Boy with Cerebral Palsy, Spastic Quadriparesis Neuro-Developmental Treatment (NDT) is a problem-solving approach that focuses on the identification and intervention of sensorimotor impairments.1 Studies by Slusarski2 and Arndt et al3 support the efficacy of NDT intervention for the improvement of gait in children with cerebral palsy and for the improvement of dynamic trunk control in infants with posture and movement dysfunction. However, other literature regarding the efficacy of NDT interventions often does not reflect the essence of NDT. For example, Mahoney et al4 discuss the effects of early motor intervention on children with Down syndrome and cerebral palsy. In their work, the authors state, “NDT involves handling a child with the goal of inhibiting abnormal tone to facilitate automatic reactions to promote normal development.” This is a limited and outdated definition of the NDT approach and does not capture the critical aspects of NDT. Essential to NDT is analysis of system impairments as they relate to functional activities and participation.5 Emphasis on the components of alignment, base of support and weight shift, as well as posture and movement strategies drive the intervention strategies.5 Finally, outcome development with the focus on functional skills that are meaningful to the family and child is fundamental to successful outcomes.5 This case report present to clinical specialists the decision-making framework and clinical reasoning that are used in NDT. This report describes the changes in motor abilities, motivation, and individual empowerment that developed following the application of NDT principles, twice weekly for 45 minutes, within a 10-week period of physical therapy, for a 10-year-old child with cerebral palsy, with motor and topography classifications of spastic quadriparesis. Jamie is a 10-year-old boy with spastic quadriparesis. Jamie is a precocious boy who is charming to the many adults that he encounters on a daily basis. He is bright and engaging while easily holding conversations about pop culture, local sports teams, and the gossip of his community. Recently, he has been on a quest to meet one of his favorite celebrities. However, he has a difficult time connecting with peers his age that may not share his interests or preferred activities. Jamie was the product of a 28-week gestation and was diagnosed with periventricular leukomalacia (PVL) during his neonatal course. His medical history is otherwise unremarkable. He received physical therapy services from the age of 7 months to the present time in a variety of settings, including early intervention, school-based therapy services, and outpatient physical therapy services. He also received occupational therapy services from age 12 months to the present. He has had intermittent periods of speech-language therapy, primarily focused around oral motor control and articulation concerns. He has no history of soft tissue surgery. He received Botox (Allergan) injections to both hamstrings in June 2005 and March 2009. Jamie’s motor disability is classified as level IV according to the Gross Motor Function Classification System.6 Children with a Gross Motor Function Level IV show self-mobility with limitations, such as power mobility in the community. He currently attends a public school in mainstream classes and completes grade-level academics without any learning disabilities. He shows anxiety and does not employ coping strategies well within personal relationships. For example, he is uncomfortable with play with same-aged peers and friends who may not be willing to play the video game of his choice. He may not tolerate going to a friend’s party that is loud and chaotic. Ultimately, his anxiety may be driven by difficulties in motor performance. Jamie demonstrates decreased neuromuscular control of both upper and lower extremities and trunk. Control, strength, and coordination of the right arm and leg are better than the left. Jamie shows disruption of sequential muscle activation, making it difficult maintain stability in response to changing environmental demands. Additionally, he shows difficulty with scaling movement control of both upper and lower extremities. Likewise, he shows impaired ability to selectively activate his legs. As a result, he cannot modify movements quickly in response to functional demands, and therefore patterns of movement are more stereotypic in nature. He also has disrupted coordination of functional muscle synergies for effective antigravity control. Consequently, his stability response to balance perturbation is impaired. Jamie shows ability to initiate movements but has reduced ability to sustain activation of antigravity postures of the shoulder girdle stabilizers, elbow extensors, hip abductors, hip extensors, and knee extensors. He also has a tendency to fix or stabilize the pelvis with muscle activation of hip flexors and hamstrings. Therefore, he shows instability during functional demands, such as lifting or reaching. Additionally, he shows decreased movement of his center of mass over his legs to activate against his support surface with his feet. Jamie shows significant instability of the trunk, and his sustained postural activation of the trunk and pelvis for core stability is poor as evidenced by his performance more than 2 standard deviations below the mean on the Sitting Reach Test. Overall strength of the trunk is in the poor range (2/5 grade of strength). Overall lower extremity strength is in the fair range (3/5 grade of strength) in the right leg and poor range (2/5 grade of strength) in the left leg, except for right hip abduction, extension, and plantar flexion, which are in the poor range (2/5 grade of strength). Range of motion of the lower extremities is decreased in the hip extensors with − 20° of hip extension on both legs. He has 30° popliteal angle on the right leg with 40° popliteal angle on the left leg. Hip abduction is 45° on the right and 30° on the left. Ankle dorsiflexion is 0 to 30° with the knee extended on the right and 0 to 15° on the left. Plantar flexion is within normal limits on both sides. Knee extension is within normal limits. Jamie demonstrates limited kinesthetic awareness of his lower extremities; he has poor awareness of his body in space. His functional vision is influenced by decreased control of visual tracking, diminished sustained visual attention, and reduced depth perception. He is hyperalert to auditory input and enjoys opportunities for vestibular input, but he has a difficult time focusing on tasks when his environment is too stimulating. As a result, he has difficulty modulating emotions, attention, and movements. Additionally, Jamie shows good problem solving in cases of novel motor challenges. With excitement, his postural tone increases, and with fatigue, his tone decreases. His overall endurance for activity is low. However, with frequent changes in tasks, he can sustain movement activity for long periods. He is dependent (assists in < 25% of task) for dressing and hygiene. He is able to complete a stand pivot transfer to the toilet involving turning/changing direction with moderate assistance (completes 50% of the transfer). Jamie requires moderate pelvic assistance as well as verbal/visual cues to complete transitions that involve turning his body in space about its axis. He also feeds himself independently. In terms of gross motor capabilities, Jaime demonstrates significant activity limitations. The Gross Motor Function Measure (GMFM) was chosen to document Jamie’s gross motor function performance as compared with other children with cerebral palsy. The GMFM-88 is a standardized observation instrument validated to measure gross motor function changes over time in children with cerebral palsy.7 His scores are provided in Table B5.1. Specific activities reveal a performance level consistent with that of an exercise ambulator. He is able to sit on a typical chair with back support and standby supervision for a period of 5 minutes. He can use his hands for nonrefined functional skills when seated in a typical chair. When seated in an adapted chair with a pelvic belt positioned, foot plates, and trunk lateral support, he is able to use his hands for fine manipulation of simple objects, such as picking up checkers or keyboarding. He is able to sustain upright sitting in an adapted seat with fair to good symmetry. However, he has a tendency to posture the head/neck in mild hyperextension with upward visual gaze. With environmental setup or positioning of the speaker at an appropriate level, he is able to orient his head upright in midline and sustain the posture for 15 minutes or more. Also noted is the posture of arms flexed with high guard with a tendency to posture with the hips adducted or the hips and knees bent in standing. Consequently, he uses a walker to sustain standing independently. He is able to walk with a reverse walker for ~ 200 yards before needing a rest. Jamie ambulates within his home with control necessary to negotiate turns around furniture and through doorways with close adult supervision for safety due to occasional loss of balance. He has demonstrated the ability to walk a quarter of a mile on a track with significantly reduced speed, during his school’s walk-athon. He is also able to control the walker to turn 45 to 90° while walking with a significant decrease in walking speed when turns are involved. He is able to walk a distance of 45 feet in 45.4 seconds. He is independently mobile in a power wheelchair with supervision for safety in congested environments. Jamie uses a power wheelchair for mobility within the school environment. He is able to scoot himself to the edge of the wheelchair to initiate a sit to stand transfer. He transfers from wheelchair to stand with minimal assistance (completes 75% of the transfer). He is able to lift himself back into the wheelchair once seated on the edge of the wheel-chair. Additionally, he is able to turn on and turn off the power to the wheelchair, and he shows safety awareness in the wheelchair. Table B5.1 Jamie’s scores on the GMFM-88
B5.1 Introduction
B5.2 Data Collection and Examination
B5.3 Examination of Functional Movement Skills
B5.4 Neuromuscular Control
B5.4.1 Strength/Range of Motion
B5.4.2 Sensory Awareness and Processing
B5.4.3 Activities of Daily Living
B5.4.4 Movement Skills
Lying and rolling | 69% |
Sitting | 58% |
Crawling and kneeling | 12% |
Standing | 5% |
Walking/running | 6% |
|
|
Total Score | 30% |
Mean GMFCS IV | 36% |
Median GMFCS IV | 32.9% |
Abbreviations: GMFCS, Gross Motor Function Classification System; GMFM, Gross Motor Function Measure.
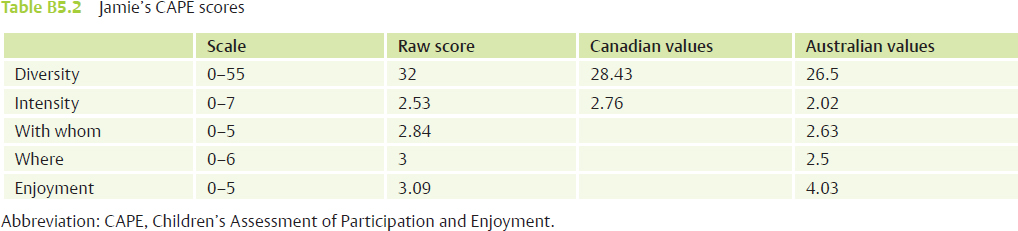
B5.4.5 Participation
The International Classification of Functioning, Disability and Health (ICF) model stresses the importance of participation as a measure of disability. In the process of evaluating the influence of motor limitations on overall participation, measures such as the Children’s Assessment of Participation and Enjoyment (CAPE)8 are useful. The CAPE measure is a self-reported assessment that examines participation in activities outside of the school day, and it provides information regarding context and enjoyment. The scale has a rating for the areas of diversity (types of activities in which he participates), intensity (the frequency of participation), with whom (the people in his family or community with whom he participates), where (activities in the home vs. the community), and enjoyment (enjoyment received from participation). A higher score for each rating area indicates a higher level of participation for that area. Testing with the CAPE was completed and demonstrated results for Jamie as seen in Table B5.2.
Test results show that Jaime participates in a wide variety of activities with his diversity value (types of activities in which he participates) greater than the values observed in both the Canadian and the Australian studies9,10 (two studies using the CAPE that defined representative performance ranges for children with cerebral palsy). His overall intensity (the frequency of participation) is low, similar to the values seen in the Canadian study. Also similar to the study values, Jamie shows decreased value of with whom (the people in his family or community with whom he participates) because his activities are primarily completed with family members. His where value reflects emerging participation in activities in school and the community as opposed to in the home only. His overall enjoyment is slightly above average but lower than reported values in the Australian study.
Summary of Function Based on the ICF Model Assessment
Participation
• Jamie participates in family life, including meals and play with his siblings.
• He participates with his extended family in community activities.
• Jamie attends public school in mainstream classes and completes grade-level academics.
• He shows anxiety and does not employ coping strategies well within personal relationships.
Participation Restrictions
• He has limited play or interaction with same-aged peers without the presence of someone from his family.
• He may not be willing to play the video game of his choice with friends who do not always comply with his wishes.
• He may not tolerate going to a friend’s party that is loud and chaotic.
Activities
• Jamie ambulates with a walker and standby supervision.
• Jamie transfers from wheelchair to walker with minimal assistance.
• Jamie transfers from wheelchair to bed or an alternative chair with moderate assistance.
• Limitation: Jamie is unable to move out of his wheelchair into alternative household positions, such as lying in bed, sitting on a sofa, moving to a table and chair for meals, moving to the toilet.
Body Function and Structure (Key Impairments)
• Increased hip and knee flexion in standing.
 Excessive muscle activity/increased muscle stiffness of hip adductors and hamstring muscle, upper extremity flexors.
Excessive muscle activity/increased muscle stiffness of hip adductors and hamstring muscle, upper extremity flexors.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree