Case Report B1 Multidisciplinary Examination and Intervention Planning for Identical Twin Infants with Extreme P rematurity
B1.1 Background and Purpose
This case report illustrates a multidisciplinary approach to intervention with identical twin infants born prematurely. Each year in the United States, over half a million (1/8) infants, are born prematurely and develop complications that result in impairments impacting their growth and development.1 For example, the effects of preterm birth may cause neurological sequelae resulting in delayed or atypical gross, fine, and visual motor development2; compromised processing and/or integration of sensory information3; impaired oral motor and respiratory control4,5; as well as reflux or other gastrointestinal conditions.6 Infants who are identified as high risk or those who have delayed motor skills on standardized tests should be referred for a multidisciplinary examination to determine the need for ongoing therapy.
Performing an effective examination requires observation and analysis of these infants’ sensory and motor behavior with respect to their environment, medical status, and family considerations. Input from the parent or care-giver is also vital to thoroughly evaluate the infant’s needs. From our experience7,8 and that of others,9,10,11 there is evidence to indicate that Neuro-Developmental Treatment (NDT) offers a viable model to observe and analyze movement and the skills to evaluate the examination data, develop an effective intervention plan, and design strategies to address the functional goals of the family. In addition, the International Classification of Functioning, Disability and Health (ICF) provides an effective framework to organize clinical observations into hypothesized system impairments and to assess the influence of the impairments on functional activities and participation.
This case report illustrates the use of the NDT Practice Model (see Chapter 5) and the ICF (see Chapter 3) to examine and analyze the sensorimotor performance of high-risk preterm twins. This case report speaks to the value of a collaborative multidisciplinary process, which includes the parent as an integral member of the team. In addition, examination and intervention photos and videos are available on Thieme MediaCenter.
B1.2 Case Description
B1.2.1 Medical History
Mya and Maddison, the subjects of this case report, are identical twins born at 26 weeks’ gestation. The infants were delivered by cesarean section to a 20-year-old single mother. At birth, Mya weighed 722.9 g (1 lb 9.8 oz), and Maddison weighed 737.1 g (1 lb 10 oz). The twins were respectively diagnosed with grade 3 and 4 intraventricular hemorrhage (IVH), mild bronchopulmonary dysplasia (BPD), stage 2 retinopathy of prematurity (ROP), and medical necrotizing enterocolitis (NEC). They remained hospitalized for 3 months and 3 days. During their hospital stay and following discharge, the twins had repeated feeding failures. Postdischarge, the girls were hospitalized three times for failure to thrive.
B1.2.2 Initial Examination
Prior to This Case Report
The initial examination was performed by an early intervention team (physical and speech therapy) when the infants were 11 weeks 5 days adjusted age (AA), which was a chronological age of 5 months 28 days. Weekly physical and speech therapies were recommended. Physical therapy was provided in a clinic setting, but medical appointments and frequent illnesses interfered with consistent physical therapy services. Scheduling challenges interfered with immediate access to speech therapy. An occupational therapist was not included as a member of the initial examination team.
B1.2.3 Case Report Examination
At 17 weeks 6 days AA (8 months chronological age), the infants began receiving all three therapy services in a clinic setting, and their mother consented to participate in our case report.
Parental Concerns
During our initial meeting, we talked with the mother and noted her concerns and questions to ensure they were considered during the analysis of the examination data and later addressed in the intervention plan and the goal-setting meetings. At this meeting, she expressed worries regarding the babies’ feeding and sleeping patterns. She also informed us that her doctor was tracking the infants’ growth, weight gain, and difficulties with feeding. The babies’ mother also voiced fears about the twins’ motor development and vision secondary to their diagnoses of ROP. In addition, the mother reported that Maddison failed the newborn audiological screening, and the mother noticed that Maddison did not startle when exposed to loud unexpected noises. Finally, the mother articulated difficulties with activities of daily living (ADLs), including bathing and positioning. She requested assistance with problem-solving solutions to all of these issues. These concerns, together with the responsibility of being a single parent to the twins and their 3-year-old sibling, left the mother feeling stressed and anxious.
Participation/Societal/Attitudinal Factors
Participation and societal factors were also identified. The mother was able to apply her previous parenting experience to identify concerns and advocate for her infants. The twins were also fortunate to have a large and supportive extended family. Although the babies were enrolled in the state early intervention program and many of the service providers came into the home, other services could only be accessed by bringing the infants to a clinic setting. This necessitated travel time and babysitting for the sibling.
Examination with Standardized Testing
Our initial examination consisted of a standardized assessment tool as well as clinical observations. In an NDT examination, the clinical observations include in-depth examination of base of support (BOS), alignment, and posture and motor control during spontaneous and elicited motor activities. Standardized testing provides a mechanism to benchmark infant performance with respect to normed scores for infants of similar ages and to assess changes in motor performance following intervention and outcomes relative to the infants’ individualized goals.12,13,14
Both twins were assessed using the Test of Infant Motor Performance (TIMP). The TIMP evaluates functional motor behavior in infants between the ages of 34 weeks postconceptional age and 4 months postterm.13 The TIMP is a test of the postural and selective control of movement needed for functional motor performance in early infancy. Research12,13,15 has shown that the TIMP can effectively discriminate among infants with varying degrees of risk for poor motor outcome based on perinatal medical conditions and can diagnose motor developmental delay based on age standards developed from a sample of 990 U.S. infants of all races/ethnicities.
TIMP test scores at 3 months of age have been shown to predict 12-month motor performance with good sensitivity (92%) and specificity (76%).12,13 Finally, the TIMP is sensitive to the effects of physical therapy provided to high-risk infants in the special care nursery and to home exercise programs taught to caregivers of premature infants following the infants’ discharge from the hospital.7,16,17
Mya’s raw score of 123 points placed her at the 50th percentile for her age. Maddison had a raw score of 111, which is in the 25th percentile and one point below the cutoff score (< 112) for referral. However, both infants qualified for early intervention based on their neonatal history. They also demonstrated difficulty organizing spontaneous movements in the upper and lower extremities (UEs and LEs) in multiple positions. In addition, at 8 months chronological age, they were unable to roll, sit, or push up on extended arms.
The standardized testing provided us with an overall view of the infants’ abilities to move spontaneously and to organize movement with respect to items that were designed to elicit a range of motor performance in prone, supine, sitting, side lying, and standing. Clearly, Maddison is a candidate for intervention, but Mya’s performance, while in the 50th percentile, is clinically worrisome because she is unable to organize her movements to explore her environment. In this case, as demonstrated from the next discussion of our clinical observations, Mya and Maddison would benefit from intervention. In addition, it was also vital to address the mother’s concerns about feeding, handling, and positioning for both infants.
B1.3 Application of NDT and the ICF Model to Examination and Intervention Planning
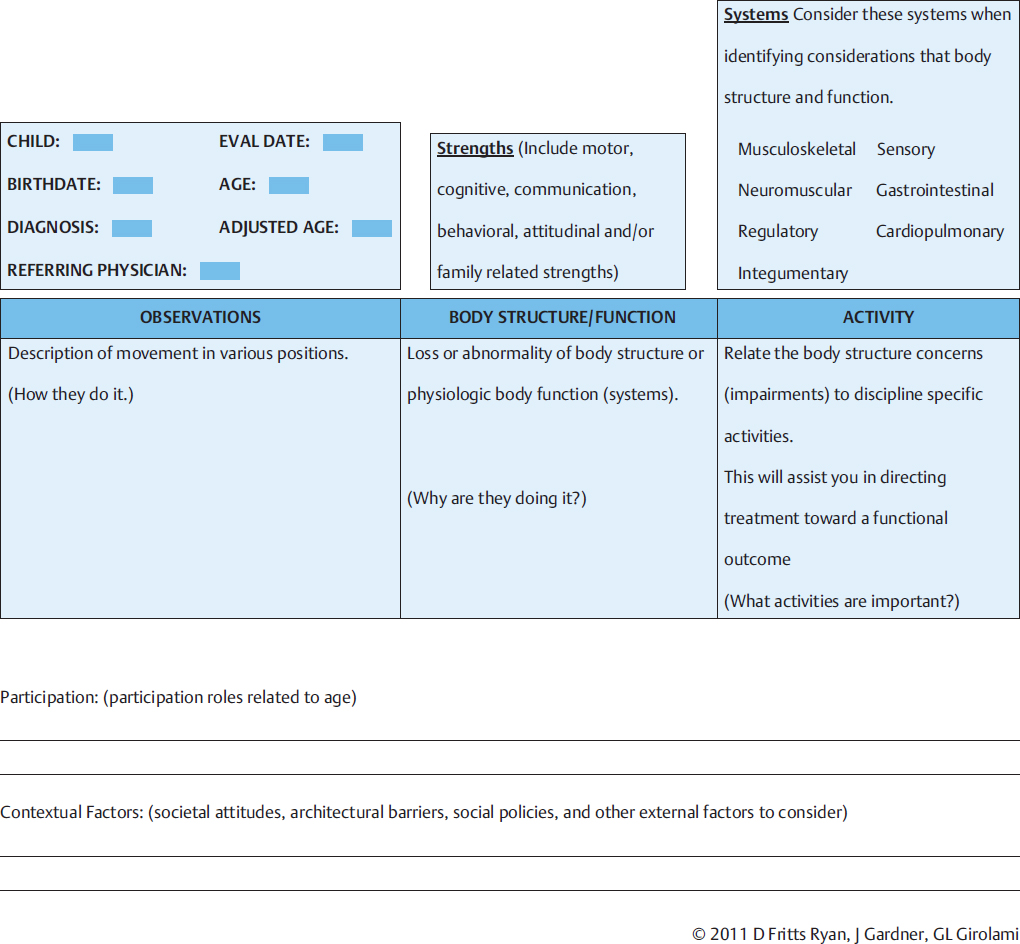
The Examination Worksheet (Fig. B1.1) was used as a data collection form to capture information from the first three phases of the process: clinical observations, hypothesized body structure and function impairments, and functional activities.
B1.3.1 Phase One: Observations
The examination was initiated by gathering observational data that are evaluated to hypothesize body structure and function impairments, design intervention plans, and develop meaningful individualized intervention strategies. In the NDT framework of examination and intervention, it was important to observe the functional ability of the infant and compare it to functional activities consistent with the adjusted age. Next, it was critical to note the presence and/or absence of the components necessary to successfully achieve each identified functional activity. Thus it was possible to hypothesize the significant body structure and function system impairments (neuromotor, sensory, cardiopulmonary, etc.) that were interfering with motor acquisition and then identify the motor and sensory components necessary to achieve the next functional level.
Through the lens of NDT, we examined the infants in the following positions: supine, prone, rolling, pull to sit, sitting, horizontal suspension, protective extension, and standing to obtain a holistic overview of their sensorimotor competency. In each of these positions, it was critical to observe how the infants organized their posture, alignment, and BOS and how they initiated, graded, and terminated muscle activity to prepare for and respond to changes in their position relative to gravity. We also observed their spontaneous motor ability and changes in posture and movement in response to handling, to the environment, and with respect to an array of stimuli (i.e., visual, auditory, or tactile). Observing and examining spontaneous and elicited movement in various positions was important because babies are placed in or selectively choose these positions during the first year of life.18 In addition, physicians routinely incorporate these postures in their examination of the infant when evaluating development and neurological integrity.19
Throughout our examination, we also gathered information regarding the babies’ adaptive responses to various sensory inputs and the influence of the stimuli on movement, posture, and alignment in all eight positions. The infants’ regulatory organization was also assessed. The regulatory system involves the ability to modulate the intensity of the arousal level while remaining engaged in the activity/interaction.3 It was important for us to determine how the level of arousal supported or compromised the infants’ motor and social behavior and their participation in daily activities.
There are a variety of ways to organize the examination observations. Refer to Thieme MediaCenter, which offers photos and videos of each infant in the above-described positions during their first examination and evaluation. These photos and videos allow for further examination of the twins’ alignment, posture, and responses to spontaneous and elicited movement in each position.
B1.3.2 Phase Two: Body Structure and Function Considerations
After gathering the observation data, we next initiated the evaluation process. This process began by hypothesizing if and how each system might be interfering with the body structures and functional activities. Armed with these hypotheses, we met with the mother to develop the functional goals. This goal setting was followed by the creation of discipline-specific intervention plans and applicable intervention strategies. Based on the observations we made during the examination, we describe an example that demonstrates the process of hypothesizing body structure and function impairments.
Example
Both infants used extension and pushing strategies when placed in sitting. They had difficulty organizing and sustaining upright sitting and were unable to generate the protective, anticipatory, or compensatory postural responses to independently sustain this position.
Hypotheses
We discussed potential impairments in the musculoskeletal (i.e., weakness or range of motion limitations), neuromotor (i.e., inadequate ability to initiate or selectively control muscle activity or poor agonist/antagonist control), sensory (i.e., vision or vestibular issues), and gastrointestinal (i.e., reflux) systems. Through our range of motion examination and observations in different positions as well as conversations with the mother, we ruled out significant impairments in the musculoskeletal and gastrointestinal systems. However, in each position, we noted both infants had difficulty initiating activity in the trunk flexors and grading agonist/antagonist control of the trunk flexors and extensors. In addition, neither baby could selectively control shoulder, elbow, and wrist movements in the sagittal or frontal planes, and this lack of control interfered with their ability to use their upper extremities (UEs) for support. Therefore, we hypothesized that the most significant impairment was in the neuromotor system, specifically initiation, selective control, and grading of trunk and UE muscle activity.
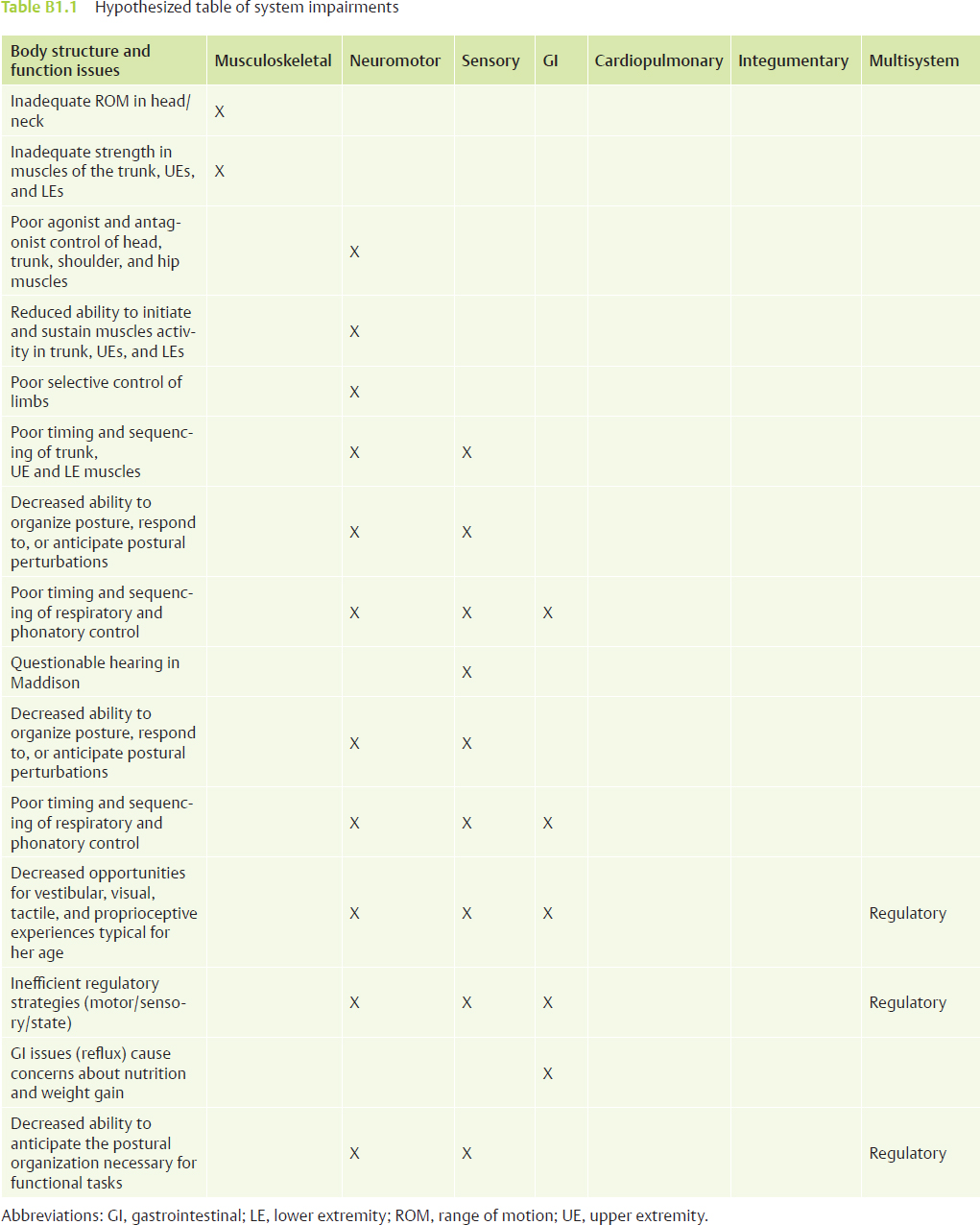
The process described above was applied to each of the identified functional activities. After observing, discussing, and testing a variety of hypotheses relevant to our observations, we generated a hypothesized list of key system impairments for each infant (Table B1.1). Careful appraisal of the impairment list allowed us to identify the redundant body structure and function impairments that received greater consideration when the intervention plan and strategies were designed.
As we hypothesized and prioritized the challenges in the various systems, we observed redundant issues in each position that affected the infants’ function. For example, consider the body structure (neuromotor impairment) of poor agonist/antagonist control of the head and trunk in Maddison (Fig. B1.2). She demonstrates this poor control in every position. After analysis, we concluded that her difficulty grading and controlling concentric and eccentric activity of the neck flexor and extensor muscles interfered with her ability to achieve adequate and symmetrical capital neck flexion to balance the strong neck extension. This predominance of neck extension biomechanically increased shoulder elevation, which, in turn, interfered with her ability to balance the trunk flexor and extensor muscles and also interfered with the scapular rhythm to support free UE movement needed for protective and support responses and sensorimotor exploration her body and the environment.
In addition, the imbalance of neck muscle activity prevented her from achieving optimal positional stability of the head and upper trunk necessary for the efficient timing and sequencing of bottle feeding. Therefore, by addressing the imbalance of agonist and antagonist control of her neck muscles’ activity, we optimized her sitting posture and alignment and enhanced the use of the UEs for functional and sensory exploration while also addressing feeding, which was a concern voiced by her mother and pediatrician.
A similar thought process was applied to the observation for Mya, who demonstrated decreased ability to organize posture and respond to or anticipate postural perturbations. Based on our observations, we considered possible sensory and neuromotor impairments. For example, in facilitated rolling, she required external assistance/guidance to initiate the lateral weight shift of her center of mass over her BOS, and head righting was inefficient (left greater than right). In addition, Mya’s ability to initiate, sustain, and selectively control movements was poorly developed.
Antigravity reach was limited in supine with strong scapular adduction, elbow extension, and intermittent fisting (Fig. B1.3). When Mya did bring her arms forward to the midline, she used shoulder circumduction, and the reach approach was ungraded and without intralimb disassociation. Mya substituted elbow extension and hand fisting for smooth elbow flexion, wrist extension, and open fingers. Once mid-line was achieved, she was then able to open the right hand but tightly clasped the left to provide increased trunk and upper limb stability for play. The stiffness of her movements decreased the proprioceptive feedback received, which is needed to assist with graded movement. However, Mya did realign her UEs toward the surface in anticipation of the position change as expected for her adjusted age.
Visual attention and engagement appeared fleeting and effortful in many activities and positions. Mya’s mother reported that, in some situations, Mya appeared more relaxed during supine play. From our observations and discussion with the mother, we determined that the level of self-regulation demonstrated during examination may negatively contribute to Mya’s ability to selectively initiate and sustain movement. Therefore, both neurological and sensory regulatory aspects were addressed during the intervention.
B1.3.3 Phase Three: Identify Functional Activities
This section outlines discipline-specific functional activities and illustrates how to write an intervention plan. These descriptions will provide additional examples of specific impairment areas that were hypothesized and addressed during intervention sessions and in the home programs.
The team identified the functional activities to emphasize for Mya and Maddison, while keeping in mind the mother’s priorities. The therapists also focused on immediate expectations for movement transitions, play, ADLs, and interaction as well as underlying motor and postural control needs to advance the infants to the next stage of development.
Physical Therapy: Examples of Functional Activities for Mya
Physical therapy interventions were designed to progress the infants in the acquisition of the gross motor and transition skills needed for independent play and the development of higher-level gross motor functional activities. Mya, who had more advanced motor skills than Maddison, was able to roll to her right side, but she could not independently make the transition to prone. With respect to rolling to the left, she was not as advanced, and she required assistance to initiate the supine weight shift needed to roll to side lying and continued guidance to complete the transition to prone. In prop sitting, Mya exhibited upright head control but recruited strong activation of trunk extensor muscles when attempting to sustain this position for play. When placed in standing, Mya supported on stiffly extended legs, causing a backward shift in her center of mass and an inability to align her trunk and hips over her BOS. In both supported sitting and standing, Mya demonstrated poor agonist/antagonist muscle activation, inefficient grading of muscle activity, and the lack of anticipatory and compensatory postural control to organize and sustain her posture over her BOS.
Fig. B1.3 In prone the extensor muscles of the trunk and lower extremities are strongly activated without antagonist control of the trunk flexors. Strong shoulder adduction and extension interfere with her ability to prop on forearms. Mya is unable to reach for a toy.
The mother voiced concerns regarding her infants’ inabilities to roll to prone and to sustain independent sitting. She felt they were frustrated and irritable because of their limited capacities to explore and play with toys. She voiced a desire to see them progress in their rolling, sitting, and standing skills. Based on the mother’s concerns, the following goals guided the physical therapy intervention.
1. Rolling from supine to prone to expand play opportunities and independent transitions.
2. Independently prop sitting to reach for and play with toys.
3. Maintaining supported standing for dressing, calming, and parent interactions.
Based on the physical therapist’s observations and hypothesized impairments, the following activities support the development of the postural and motor control necessary to facilitate the acquisition of the functional skills identified by the mother.
• Mya will be able to reach for and play with her legs and feet when she improves her abdominal strength and postural control, allowing her to sustain antigravity UE extension and pelvic lifting in supine. In addition, she will gain the motor skills to support sensory experiences and improved body awareness. Mya would also develop the core strength and control needed to initiate and experiment with weight shifting to the right and left (crossing midline) and returning to the midline balance point. This activity is a precursor to rolling, improves control of agonist/antagonist trunk muscle activity, and grading and experience of eccentric and concentric control. The ability to roll independently would expand play opportunities and independence.
• Mya will sustain forearm weight bearing and exploring weight shifting in prone, so that she will begin to develop trunk elongation, which will lead to reciprocal LE movement and the strength and control for independent rolling.
• Mya will independently roll to contribute to spinal flexibility in the frontal plane. This flexibility will facilitate antigravity lateral head and upper trunk lifting necessary for efficient rolling and enhanced LE disassociation.
• Mya will independently prop sit, thereby improving strength and the ability to grade muscle group activity in the UEs and trunk. The ability to initiate head turning without losing balance will drive weight shifting over the BOS, improve postural control in the sagittal and frontal planes, and contribute to the emergence of compensatory postural control. Control of independent sitting will provide a solid base for Mya to use her hands for exploration of her body and playing with toys.
• Mya will stand supported, developing the strength and grading to achieve positioning of her center of mass over the BOS. Control of her posture in standing will permit Mya to strengthen hip extensors and abductors, learn to grade hip and knee flexion, and practice weight shifting, bouncing, and small stepping movements.
See Table B1.2 for a summary of Mya’s physical therapy goals and body system impairment list.
Physical Therapy: Examples of Functional Activities for Maddison
The mother expressed similar goals for Maddison, although her gross motor skills in prone, sitting, and standing were not as advanced as those demonstrated by Mya. In addition, while Mya tended to use excessive and ungraded extension to maintain and play in these positions, Maddison used a strategy of flexing her limbs and holding her UEs together in midline. However, both infants required improved trunk and pelvic flexibility, muscle strength and grading, and the emergence of the compensatory and anticipatory control necessary to sustain balance. Therefore, the intervention plans for both infants looked similar, but the emphasis of the intervention strategies was altered to address their individual musculoskeletal, neuromotor, and sensory impairments. Thieme MediaCenter provides narrated videos that demonstrate how the intervention strategies were individualized for each infant.
Table B1.2 Physical therapy intervention planning worksheet
Name of Client: Mya | Date: ____________________ |
Functional goals | Body structure and function impairment list |
Mya will independently roll from supine to prone (over right and left sides) to play on her tummy. | • Insufficient spinal and pelvic mobility. • Insufficient strength and endurance in muscle groups in trunk, UEs, and LEs. • Poor agonist and antagonist control of trunk, shoulder, and hip muscles. • Poor selective control of limbs; repetitive limb movements. • Reduced variety of motor patterns in limbs. • Poor timing and sequencing of trunk, UE, and LE muscle activity. • Insufficient ability to initiate and sustain muscle activity
• Decreased ability to anticipate and organize feedforward and feedback postural organization required for this task. |
Interventions—sequence strategies relative to prioritized impairments | Expected impact on body structures and functions | Assess effectiveness of strategies: adapt, revise, or eliminate |
1. Activities to improve trunk stability and rotation in supine, prone, sitting. 2. Activities to increase activation and agonist/antagonist control of upper and lower extremities in supine, prone, sitting. 3. Weight-shifting activities in supine, prone, side lying, and sitting to improve ability to initiate and sustain muscle activity for weight-bearing, reaching, and transition activities. 4. Activities in supine, prone, side lying, and sitting to encourage Mya to initiate weight shifting with reaching for objects in supine, prone, side lying, and sitting. See Thieme MediaCenter for a video clip that shows working on this strategy and addressing which impairments are worked with. 5. Incorporate sensory strategies. 6. Activities in supine, prone, side lying, and sitting to encourage Mya to initiate transitions into and out of supine, prone, side lying, and sitting. 7. Activities in supine, prone, side lying, and sitting to encourage Mya to anticipate and respond to internal and external perturbations. | 1. Increased joint mobility and muscle strength in trunk, UEs, LEs. 2. Increased ability to sustain muscle activity in the UEs and trunk in all postures. 3. Improved ability to reach in all planes of movement while sustaining postures in supine, prone, side lying, and sitting. 4. Improved ability to initiate movement in the UEs and LEs for transitions, reaching, and UE weight bearing. 5. Improved ability to initiate UE and LE movements and weight shift outside the base of support without loss of balance. 6. Improved LE disassociation for weight shifting, rolling, and eventual transitions. 7. Improved ability to anticipate and respond to weight shift and to prepare for transitions. |
|
Abbreviations: LE, lower extremity; UE, upper extremity.
Occupational Therapy: Examples of Functional Activities for Mya
Occupational therapy interventions were designed to address components of performance in activities needed for reach and hand function, visual motor skills, UE support, and play behaviors. For Mya, reach and grasp were deficient in all positions and interfered with her ability to contact, grasp, and play. Mya used her UEs to substitute for inadequate symmetrical head and trunk control. Movements, when initiated, were ungraded and lacking in variety. In both prone and supine, typical 5-month-old play positions, Mya held her arms stiffly, and her grasp was tense and lacked the fluidity to accommodate the variability and size of different toys. Therefore, Mya’s ability to sustain a gross grasp and to learn through early reach and grasp experiences was limited. This lack of experience with reach and grasp limited Mya’s ability to use the UEs for exploring her environment and compromised experiences gained from the visual, tactile, and proprioceptive systems.
The development of postural control, ocular motor skills, as well as arm and hand function will allow both Mya and Maddison options for self-play and visual exploration, which was a goal expressed by their mother. In addition, their mother also articulated concern regarding functional areas for Mya. The following goals were set for Mya.
1. Finding positions and activities to strengthen visual attention and visual skills is extremely important to improve ocular motor fixation, localization, and tracking in all positions.
2. Improving Mya’s ability to sustain a posture and to independently play is critical to freeing the mother to pursue the needs of the other children.
3. Advancing UE skill and control to independently grasp and hold a rattle.
Activities that reflect achievement or will lay the fundamental groundwork for eventual achievement of the above goals included the following:
• The ability to easily and consistently reach up to mom’s face or to a toy while in supine and when supported in a seating device. To do this, Mya would need to develop increased strength and control to stabilize and control her head, trunk, and shoulder girdle. This would effectively free her arms and hands for reach, grasp, and play. In addition, the ability to reach, grasp, and explore different body parts is a primary way that 5- to 8-month-old babies improve self-regulation and body awareness and develop security in their ability to weight shift around the midline. This exploration would also provide rich opportunities for integrating multisensory information for play and awareness of the environment.
• Developing the skills to play with toys placed within arm’s reach when in prone. The ability to actively bear weight in forearm or extended arm propping while looking around in the environment will facilitate the weight shifting to develop reaching in space and eventually reach and grasp in prone. Reach and grasp will facilitate independence for play in prone, and this in turn will free up the mom’s time to spend with the other children (e.g., helping her 3-year-old get dressed or diapering Maddison). Mya also required increased active weight bearing and weight shifting around the body axis (rotation in the transverse plane) as well as the ability to shift her weight caudally toward the pelvis to increase stability for UE play. Active UE supporting would also provide Mya the stability for prolonged head lifting and turning that would permit visual scanning of her environment. In addition, Mya would benefit from the tactile and proprioceptive input to her arms and body, promoting better grading and awareness of her extremities. The improved ability to support her body and engage in her surroundings will create viable options for independent play in prone.
• Grasping and beginning to investigate a rattle with either hand while in a supported sitting position. Addressing the fundamental areas of organizing and strengthening postural control with reach will begin to allow more opportunities for Mya to use her hands to play with objects. In addition, specific preparation of the hand to accommodate to various sizes and shapes should begin in well-supported positions. The ability to grasp and mouth a toy, as well as to sustain the grasp and interact with a person or object in the environment, would build the foundation for self-initiated play and the ability for Mya to entertain herself.
Based on the analysis of the body systems’ structure and function, occupational therapy intervention strategies for Mya were prioritized. These are specifically outlined in the intervention section of Table B1.3.
Occupational Therapy: Examples of Functional Activities for Maddison
The twins’ mother expressed the same functional areas of concern for Maddison. Therefore, when examining activities appropriate to address with Maddison, the occupational therapist developed the same functional goals already presented for Mya. However, the intervention strategies and the handling applied differed because Maddison demonstrated more sensory aversions, less strength, and lower muscle tone with decreased ability to initiate movements than Mya. Videos of individualized intervention strategies can be viewed on Thieme MediaCenter.
The mother faced additional challenges with Maddison. This twin was unable to tolerate and enjoy bath time. Sensory and handling strategies specific to bathing were incorporated in Maddison’s intervention and home program activities. For example, deep pressure in a supportive supine flexed position was used by her mother to prepare Maddison for her bath. This position was carried over during bathing with supportive handling from her mother. Visual regard of her twin was also helpful.
Speech Therapy: Examples of Functional Activities for Mya
Speech therapy addressed oral motor, feeding, respiration, and language performance. For both Mya and Maddison, their mother was concerned about the growth and nutrition expectations outlined by her pediatrician. She also expressed the need to develop a manageable feeding schedule. Finally, efficient feeding and coordinated sucking, swallowing, breathing, and vocalizing were key areas of speech therapy focus.
For Mya, activities identified by the speech therapist that would reflect development of the foundations for accomplishing the above goals included the following:
1. Developing a consistent feeding schedule that the family could handle with correct calorie intake for growth and development.
2. Sequencing suck-swallow-breathe when bottle-feeding.
3. Maintaining sufficient airway clearance during feeding time.
4. Maintaining appropriate neck alignment and symmetry of head position to support swallowing.
5. Using sustained oral vocalizations to demonstrate communication intent.
6. Demonstrating improved respiration and phonation to transition from short nasal phonation to sustained oral phonation, through improved trunk alignment and control.
Table B1.3 Occupational therapy intervention planning worksheet
Name of Client: Mya | Date:____________________ |
Functional goals | Body structure and function impairment list |
1. Mya will reach up with either hand to Mom’s face or a toy easily and consistently in supine and in supported seating without being held by Mom. 2. Mya will play on her tummy on the floor with toys placed within arm’s reach for 5–10 minutes on her own. 3. Mya will grasp and mouth, grasp and engage in basic cause effect, entertaining herself for 5–10 minutes. 4. Mya will look, reach, and grasp a toy with either hand while floor sitting while Mom feeds twin for 5–10 minutes. | • Poor ability to initiate and sustain muscle activity in
• Poor selective control of muscle activation. • Poor dissociation of right/left sides of body, upper and lower body, upper/lower part of arm. • Poor timing and sequencing. • Decreased control of posture with vision. • Decreased control of posture with reach/grasp. • Decreased experiences using vision with reach and grasp. • Deficient strength of flexion/extension muscles in trunk, UEs, and LEs. • Poor agonist and antagonist control of trunk, shoulder, and hip muscles. • Decreased ocular fixation with postural control and with reach. • Decreased opportunities for this sensory motor experience. • Decreased ability to anticipate (feedforward) the postural organization necessary for functional tasks. |
Interventions—sequence strategies relative to prioritized impairments | Expected impact on body structures and functions | Assess effectiveness of strategies: adapt, revise, or eliminate |
1. Handling to improve sensory tolerance to using symmetrical trunk control with compensatory retracted UEs (deeper pressure, UE inhibition with aligned trunk and imposed weight shift, visual direction to match activity). 2. Activities to improve trunk stability, especially in frontal and transverse planes with UE compensatory patterns inhibited in prone, supine, and sitting while promoting head lifting and turning to visual and auditory inputs. 3. Activities to improve trunk control with scapular depression, shoulder flexion, and external rotation, such as unilateral WB and WS with active forward reach in prone, side lying, and sitting. 4. Activities to incorporate trunk, vision, and unilateral and bilateral reach to body parts and to objects. 5. Incorporate sensory strategies of increased proprioceptive/tactile input with handling to improve modulation and attention during movement (e.g., try ball surface in sit, side lying, and prone with ability to impose weight shift to activate more balanced use of posture in all activities). 6. Incorporate activities (as able) to encourage exploration of toys using both hands and visual engagement while posture is supported (e.g., object placement/timing/choice to match motor and visual goals, texture to promote fingering, interaction to promote sustained attention). 7. Assisting Mom to find ways to increase visual engagement and attention; increase grasp accommodation experiences. 8. Adaptive positioning to carry over team goals of symmetry, midline postural control in play positions: bouncy chair, prone propping over a roll and Boppy Pillow, travel chair with insert and tray. | 1. Decreased hyperalert response during movement and play. 2. Decreased stiffness in reach; graded UE and hand placement and exploration. 3. Increased variation in reach for play objects. 4. Sustained UEs in weight-bearing placement over open hand. 5. Increased fingering exploration of toys. 6. Grasp accommodation to varied shapes with active thumb movement. 7. Increased visual fixation and attention; increased cause–effect play. 8. Bouncy chair, prone prop over roll and Boppy Pillow, travel chair with insert. |
|
The mother’s priority for Mya was improved calorie in-take to maintain medically acceptable levels on all growth charts. Prior to this time, the twins had been hospitalized three times for failure to thrive and vomiting. In addition to the evaluation of movement control in a variety of positions, bottle feeding was also assessed. Mya’s position of excessive shoulder elevation and neck extension made coordination of suck-swallow-breathe difficult. Alignment during feeding needed to be addressed, as did choice of bottles, nipples, and formula.
Positions that required more upright control were demonstrated and taught to the mother. These positions supported improved bottle feeding and they optimized the introduction of strained foods by spoon. Improved positioning also supported Mya’s capability for communication and play. See Table B1.4 for a summary of Mya’s goals, body structure and function impairments, and intervention strategies.
Speech therapy also addressed respiration and phonation. Mya could activate her diaphragm when the need for postural control was less demanding (e.g., supine). As the postural demands increased, she had difficulty coordinating respiration and vocalizing. As suggested by Massery,20 “Trunk control, breathing and internal functions such as the GI tract, are dependent on the ability of the body to generate, maintain and regulate pressure in the thoracic and abdominal chambers.”
Speech Therapy: Examples of Functional Activities for Maddison
The concerns for Maddison were similar to those already presented for Mya. However, Maddison had more asymmetry, less trunk strength, and a slower respiratory pattern than her twin. Feeding and positioning strategies were similar, yet had to be adapted to specifically address Maddison’s differences. In addition, Maddison lacked the ability to consistently respond to and localize auditory stimuli and was suspected of having a hearing impairment.
B1.3.4 Phase Four: Developing a Plan of Care
The success of the intervention plan depends on a dialogue between the parent and the therapy team. In our case, the parent contributed information that augmented our observations and was instrumental in development of the functional goals written for each infant. Our next step was prioritizing the hypothesized impairments that interfered with goal achievement and designing intervention strategies to address all identified impairments.
NDT education provides the therapist with the theory and practice to develop the individualized intervention strategies to achieve optimal functional outcomes.7,9,21 The NDT-educated therapist also possesses the handling and evaluation skills to expertly implement and modify each strategy based on the needs and performance of the infant throughout the intervention session.
In the case of Mya and Maddison, the parent-identified goals and body structure and function impairments were similar for each infant. Review Table B1.2, Table B1.3, and Table B1.4 to see the physical therapy, occupational therapy, and speech intervention plans for Mya. They also describe the intervention planning phase of the NDT problem-solving framework. The upper section of each table exemplifies the discipline-specific functional goals for Mya and the hypothesized body structure and function issues that interfere with acquisition of the discipline-specific goals. The lower section prioritizes the intervention strategies (column one) and their expected outcome (column two) on the hypothesized body structure and function impairments.
It was also critical to evaluate the effect of each strategy. This was accomplished through critical, online assessment (i.e., second to second) of the effect of handling based on the infant’s sensory and motor responses. We also considered how handling effects positive or negative changes in posture and movement. This ongoing examination allowed us to adapt and revise each strategy throughout the session to ensure optimal responses in the infant’s sensory and motor performance, thus creating a support environment for the attainment of functional skills. This online thought process is documented via the narrations for each of the intervention videos on Thieme MediaCenter which offer the opportunity to compare and understand how the intervention strategies were applied and modified based on the individual needs and responses of each infant.
B1.3.5 Phase Five: Home Programs
NDT encourages functional home programs that offer opportunities to practice the components necessary for skill acquisition in daily routines. Our team explored possibilities for meaningful home carryover of activities that supported the team goals. Initial home program ideas were directed toward the development of manageable feeding routines for both Mya and Maddison, which were critical due to concerns related to failure to thrive. Specific strategies have already been outlined in the section on speech therapy intervention.
It was also important to recognize the mother’s environment and participatory constraints and to offer home activities that could be consistently implemented every day. Therefore, we developed viable positioning options that could be incorporated before and after feedings. These positions freed the mother to feed one baby at a time or to address the needs of the older sibling. In addition, these positions were safe, and they optimized alignment and supported the development of improved postural control. The positions encouraged symmetry and promoted head and trunk control, UE reaching, and engagement opportunities to support self-initiated play. Fig. B1.4 shows the twin’s mother positioning her infants as instructed for feeding.
The following positioning options were recommended with the suggestion that they be rotated throughout the day.
1. An adapted feeding seat was recommended with a pummel and rolled towels to aid positioning. A tray was added to encourage forward weight bearing on UEs. This positioning provided effective practice for increased UE symmetry, visual interaction, and should girdle stability for exploration of toys using hands together in the midline.
2. For prone play, we suggested a rolled towel or small Boppy Pillow (The Boppy Company, LLC) to biomechanically shift weight backward toward the pelvis. This position facilitated the twins’ abilities to lift and turn their heads and promoted midline UE alignment and opportunities to use the hands for play and exploration.
Table B1.4 Speech intervention planning worksheet
Name of Client: Mya | Date: ____________________ |
Functional goals | Body structure and function impairment list |
1. Mya will receive adequate nutrition for her adjusted age based on the guidelines established for infants with very low energy expenditure. 2. Mya will maintain a continuous suck-swallow-breathe pattern when drinking 6 oz of formula. 3. Mya will eat 4 oz of strained food when being spoon fed by a parent. 4. Mya will use sustained vocalizations to create a communication loop with her mother during play activities. | • Poor ability to initiate and sustain muscle activity while feeding with
• Poor selective control of muscle activation. • Tongue and jaw decreased stability. • Poor timing and sequencing of suck-swallow-breathe pattern. • Deficient in strength of flexion/extension muscles in trunk, UEs, and LEs to support alignment needed in head/neck while feeding. • Poor agonist and antagonist control of trunk, UEs, LEs. • Decreased ability to anticipate the postural organization necessary for this functional task (feedforward). • Mom’s lack of information regarding prematurity and nutritional needs. |
Interventions—sequence strategies relative to prioritized impairments | Expected impact on body structures and functions | Assess effectiveness of strategies: adapt, revise, or eliminate |
1. While feeding with the bottle, support the baby’s head at the base of the skull. Apply a slight elongation of the neck to flex the head slightly. 2. Place your finger in the lateral portion of the gum ridges. Allow the baby to munch on your finger. This will allow better tongue/jaw separation during feeding. 3. Use a bouncy chair with rolls to improve head and trunk positioning. Feed solids in this upright symmetrical position. 4. Provide opportunities to chew on her fingers, teething toys, or your little finger (placed on the lateral portions of the gum ridges). This activity will allow better separation of the tongue and jaw during feeding. 5. Feed in an upright symmetrical position for solid foods. 6. Thicken liquids with cereal to allow more time for the swallow. (Mya swallowed much faster with cereal added to thicken food). 7. Assist Mom to eliminate Mya’s habit of grazing on bottle throughout the day. 8. Define nutritive versus nonnutritive sucking for Mom. 9. Help Mom establish routine feeding schedule.
| Improve head flexion during sucking and improve tongue position while bottle drinking and with solids. |
|
Abbreviations: LE, lower extremity; UE, upper extremity.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




 Upward rotation of scapula for arm movement overhead.
Upward rotation of scapula for arm movement overhead. Trunk muscles activity in all planes.
Trunk muscles activity in all planes. Pelvis for stability while initiating UE and LE movements.
Pelvis for stability while initiating UE and LE movements. LE reciprocal control.
LE reciprocal control. scapula depression/upward rotation with humeral flexion and with trunk control.
scapula depression/upward rotation with humeral flexion and with trunk control. abdominals, especially in frontal and transverse planes.
abdominals, especially in frontal and transverse planes. pelvis for stability while activating UEs.
pelvis for stability while activating UEs. scapula depression/upward rotation with humeral flexion and with trunk control.
scapula depression/upward rotation with humeral flexion and with trunk control. abdominals, especially in frontal and transverse planes.
abdominals, especially in frontal and transverse planes. pelvis for stability.
pelvis for stability. 7 a.m. 8 oz formula; 9 a.m. 4 oz stage 2 fruit or veggie.
7 a.m. 8 oz formula; 9 a.m. 4 oz stage 2 fruit or veggie. 11 a.m. 8 oz formula; 12 p.m. 4 oz stage 2 fruit or veggie.
11 a.m. 8 oz formula; 12 p.m. 4 oz stage 2 fruit or veggie. 2 p.m. 8 oz formula; 4 p.m. 8 oz formula.
2 p.m. 8 oz formula; 4 p.m. 8 oz formula. 6 p.m. 4 oz stage 2 fruit or veggie.
6 p.m. 4 oz stage 2 fruit or veggie. 11 p.m. 8 oz formula
11 p.m. 8 oz formula






