Chapter 3 Fluoroscopy, Ultrasonography, Computed Tomography, and Radiation Safety
 At the present time, multiple forms of radiological imaging devices are used to evaluate and confirm the diagnosis of clinical conditions.
At the present time, multiple forms of radiological imaging devices are used to evaluate and confirm the diagnosis of clinical conditions. Safety is still a very real concern, and awareness of risk that is taken with each procedure is important.
Safety is still a very real concern, and awareness of risk that is taken with each procedure is important. Interventional pain procedures are now required to be performed with the use of radiological guidance in most situations. Without imaging, patients may be placed at greater risk unnecessarily.
Interventional pain procedures are now required to be performed with the use of radiological guidance in most situations. Without imaging, patients may be placed at greater risk unnecessarily. Minimizing radiation exposure is still most important. MRI or US allows the performance of evaluations without radiation exposure, and may be considered in specific situations.
Minimizing radiation exposure is still most important. MRI or US allows the performance of evaluations without radiation exposure, and may be considered in specific situations. Careless use of and overexposure to radiation can compromise the health and well-being of both the operator and the patient being examined. Careful attention to lead apron quality, sizing, and regular safety inspections of all equipment are important.
Careless use of and overexposure to radiation can compromise the health and well-being of both the operator and the patient being examined. Careful attention to lead apron quality, sizing, and regular safety inspections of all equipment are important. The use of pulsed or reduced dose techniques of fluoroscopy are important safety measures to consider, particularly in higher dose procedures such as spinal cord stimulation electrode placement.
The use of pulsed or reduced dose techniques of fluoroscopy are important safety measures to consider, particularly in higher dose procedures such as spinal cord stimulation electrode placement.Ultrasound
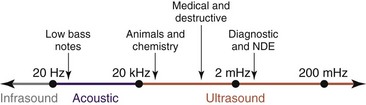
Ultrasound is cyclic sound pressure with a frequency greater than the upper limit of human hearing. Although this limit varies from person to person, it is approximately 20 kHz (20,000 Hz) in healthy, young adults, and thus 20 kHz serves as a useful lower limit in describing ultrasound (Fig. 3-1).
Safety Concerns
Most infants now born in the United States are exposed to ultrasonography before birth, and in Germany, Norway, Iceland, and Austria, all pregnant women are screened with ultrasonography. To date, researchers have not identified any adverse biological effects clearly caused by ultrasonography, even though 3 million babies born each year have had ultrasound scans in utero. This is an enviable safety record. However, the National Council on Radiation Protection and Measurements advocates continued study of ultrasound safety, improvements in the safety features of ultrasound systems, and more safety education for ultrasound system operators.1 Because of the sheer number of people exposed to ultrasonography, any possibility of a harmful effect must be investigated thoroughly.
Ultrasound gel is intended only for external use. If a needle becomes contaminated with gel, every effort should be made to remove the needle and replace it with a sterile new one. Even though the gel initially is sterile, the substance itself may irritate structures either in the epidural space or even intrathecally. Either way, one should err toward needle replacement. Remember, ultrasound gel contains propylene glycol, glycerine, phenoxyethanol, and FD&C Blue #1. For properties and side effects of ultrasound gel, see Box 3-1.
Computed Tomography
The CT scanner is an expensive yet sophisticated way to guide needle placement (Fig. 3-2). It is somewhat expensive for the routine use of image-guided procedures, especially in an office-based practice or even an ambulatory surgery center. One could justify the use of such a device if looking at a study or working in a hospital with access to a scanner. Most scanners are used daily for diagnostic workups but not for pain management procedures. They allow for excellent needle placement and biopsies that are performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree