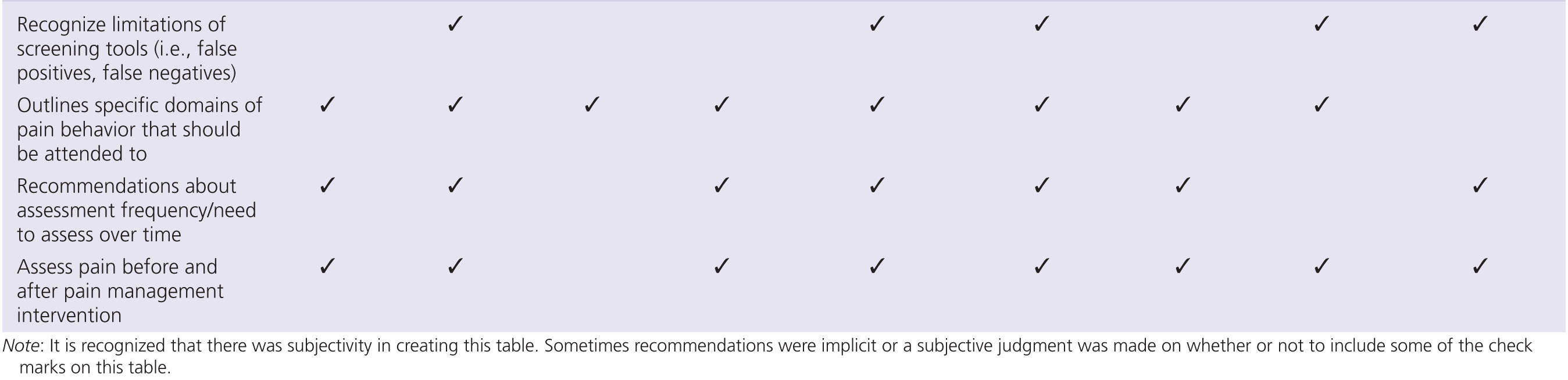
Some guidelines recommend specific standardized assessment tools while others do not. In addition, guidelines generally recognize that pain assessment is a complex process and should not be restricted to the evaluation of pain intensity. As such, emphasis should be placed on functional limitations, emotional functioning, social environment, and other related domains. The following is a summary of key points from various guideline documents.
American Geriatrics Society
The American Geriatrics Society (AGS) [4] has adopted a guideline for the pharmacological management of persistent pain in older persons but did not elaborate much on assessment. Instead, the AGS 2009 [4] document refers the reader to previous literature [24] including previous guidelines [3]. In fact, the AGS 2002 [3] guideline included more detailed information on pain assessment but much of the focus was on older adults who can self-report pain. Nonetheless, the AGS 2002 [3] task force identified the following domains as being important in the pain assessment of older adult with cognitive impairments: facial expressions, verbalizations and vocalizations, body movements, changes interpersonal interactions, changes in activity patterns or routines, and mental status changes. These domains can form the basis for the evaluation of the comprehensiveness of any pain assessment that involves the dementia patient.
Pain in Residential Aged Care Facilities (Australian Pain Society) [7]
The guideline recognizes the challenges of pain assessment in patients with dementia and provides recommendations for both assessment and management. Only the pain assessment recommendations are considered here. The guideline emphasizes a comprehensive approach to pain assessment and stresses the importance of obtaining self-report where possible, use of adaptations to simplify procedures as necessary (e.g., use of simplified language), and informant reports. Staff members are encouraged to look for the behavioral pain expressions falling under the AGS expressive domains mentioned above and to evaluate the impact of pain (e.g., on mood, ambulation). The importance of multidisciplinary collaboration is also emphasized. The Abbey Pain Scale [1] was recommended as a useful standard for pain assessment and the Resident’s Verbal Brief Pain Inventory [7] (a modified version of the Brief Pain Inventory) [14] was recommended as the standard for the assessment of residents with sufficient cognitive ability (in addition to use of numeric and verbal descriptors scales). The Australian guideline, however, was produced prior to a proliferation of psychometric research, development, and refinement of long term care (LTC) assessment tools focusing on patients with dementia. As such, the specific tool recommendations did not take into account the more recent literature.
Australian and New Zealand Society for Geriatric Medicine [52]
This document focuses on pain in older persons and contains a brief section of pain assessment that discusses pain in dementia. The section is quite general but recognizes that persons with mild to moderate dementia are often able to self-report pain as well as the importance of behavioral observation and use of observational tools. No specific tools are recommended.
American Medical Directors’ Association (AMDA) Pain Management Guideline [5]
Despite a primary focus on pain management, the AMDA guideline discusses assessment in some detail. It is directed to members of interdisciplinary teams working in long-term care (LTC) facilities. There is emphasis on physical examination and test results, along with history information, including collateral informant reports, as well as on an effort to identify the cause of pain. Staff are encouraged to look for signs and symptoms that may suggest pain. Use of a specialized assessment tool is suggested (and tool examples are given with appended copies of a few self-report and observational tools), although no tool is specifically recommended. Assessors are encouraged to make determinations of the impact of pain on mood, activity, and quality of life.
International Interdisciplinary Consensus Statement on Pain Assessment in Older Persons [24]
This consensus document represents, perhaps, the most significant international and interdisciplinary effort to develop guidelines for effective pain assessment in older persons and to cover all key aspects of assessment (e.g., physical, psychological, pharmacological, pain intensity, review of specific tools) [24]. While the document was intended to provide guidelines for seniors with and without dementia, only the sections focusing on dementia are discussed here. The large international group of authors adopted a broad focus and did not only consider guidelines for the assessment of pain (based on both observation and self-report, where available) but also outlined approaches to history taking physical examination (including mobility and balance, neurological examination, medication history, cognitive status evaluation, and assessment of psychological functioning). Most aspects of the physical examination were focused on older adults in general and were not unique to the patients with dementia. As such, they are not reviewed here.
Specific recommendations for older adults with dementia stress the importance of history, physical examination and interview information (including interview with collaborative informants), use of both self-report and observational procedures where possible [19], recommendations for specific unidimensional scales that have been shown to be useful in the assessment of older persons with mild to moderate dementia (e.g., Colored Analog Scale [CAS] [41, 47], numeric rating scales (e.g., 0 = no pain; 10 = pain as severe as it can be), or verbal rating scale, involving verbal descriptors of pain such as mild, moderate, and severe), recognition that pain assessment during movement is most likely to elicit pain behaviors, examination of whether use of analgesics results in reduced pain behaviors, use of an individualized approach to assessment involving the collection of baseline scores for each patient, consistent use of assessment tools over time (i.e., tools must be used under consistent circumstances such as during a specific transfer or program of physiotherapy), and recognition of the limitations of screening tools in pain assessment. Specific promising assessment tools such as the PACSLAC [16] and the DOLOPLUS-2 [50] are mentioned with the caution that more research was needed (i.e., no one tool was specifically recommended for the assessment of patients with dementia).
National Nursing Home Pain Collaborative [31]
Although many consensus guidelines had not recommended specific observational pain assessment tools for older adults with dementia, the National Nursing Home Pain Collaborative did so based on systematic examination of the literature, psychometric properties, and expert consensus. Specifically, the collaborative recommended use of two tools by LTC facilities: the PAINAD [49] and the PACSLAC [16]. They argued that the PAINAD is useful for daily assessment including follow-up evaluations of pain interventions, whereas the PACSLAC, being more comprehensive, was recommended as a baseline and monthly or quarterly maintenance assessment tool to reflect broader changes in behavior and activity. The PACSLAC was also recommended to facilitate integration of ongoing pain monitoring with Minimum Data Set (MDS) [10] documentation because of good correspondence to MDS indicators. It is noted that, since the National Nursing Home Pain Collaborative made these recommendations, the PACSLAC has been refined and shortened without compromising comprehensive coverage of the pain assessment domains deemed important by the AGS [11].
In addition to recommending specific tools, the Collaborative emphasized the importance of eliciting verbal report where possible, the need for comprehensive pain assessments, the need for repeated pain assessment, integration with MDS [10] and federal United States requirements, the advantages of pain assessment during movement, development of policies to ensure facility-wide pain screenings with accountable staff, and the need for continuing pain education of all front-line staff.
The British National Guideline for Assessment of Pain in Older People [46]
Together with the British Geriatrics Society and the Royal College of Physicians, the British Pain Society developed a national guideline for the pain assessment of older persons. The guideline recognizes the need for comprehensive pain assessments for all older adults as well as the limitations that people with dementia may face in the communication of pain. As such, it stresses the need for observational assessment. Domains to be assessed by observation, similar to those recommended by the AGS [3], are also outlined. The guideline emphasizes the need to attempt self-report with all patients and to adapt self-report scales, as necessary, for older adults with communication impairments. The specific tool that was recommended for observational pain assessment was the Abbey Scale [1]. Especially useful in the guideline is the presentation of an algorithm for the assessment of pain in older persons (see Fig. 13-1).
Task Force of the American Society for Pain Management Nursing [32]
This document addresses a variety of populations with limited ability to communicate (e.g., persons with intellectual disabilities, infants and persons with advanced dementia). In other words, the document is less specialized than other recommendation and guideline documents presented here. This American Society for Pain Management Nursing (ASPMN) task force recommended that a pain assessment hierarchy be established that should involve attempted self-report, search for potential causes of the pain, observation of pain behaviors, use of proxy reporting, and attempt of an analgesic trial (and evaluation of the extent to which this reduces pain indicators). The task force also recommended use of a psychometrically valid pain assessment tool and minimization of emphasis on physiological indicators (such as heart rate changes) because the correlation of such indicators with self-reported pain tends to be weak or absent. Postintervention assessment and documentation were also recommended. Specific assessment tools designed for seniors with dementia are mentioned, but the reader is referred to the work of the National Nursing Home Pain Collaborative document [31] reviewed above.
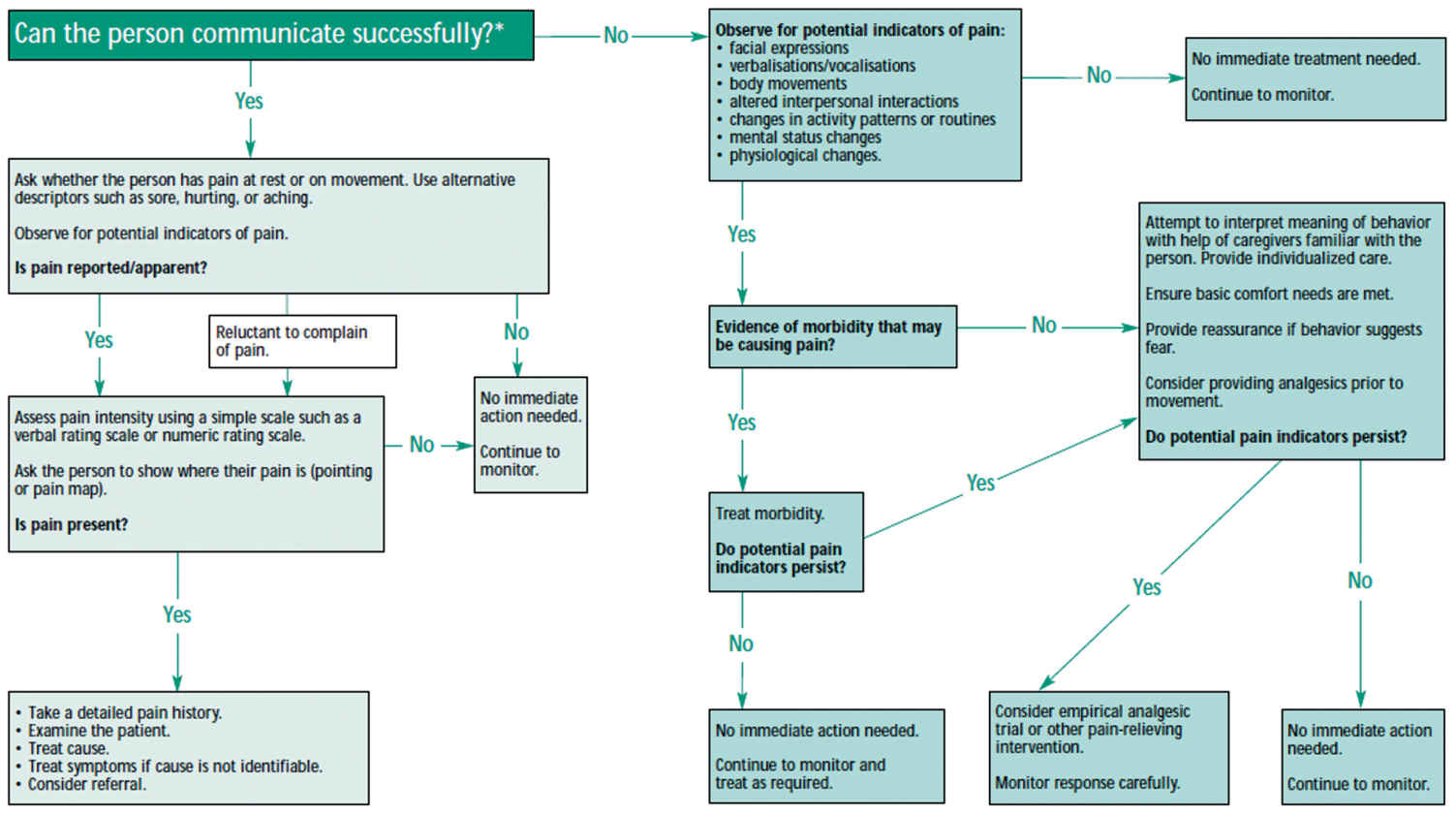
FIGURE 13-1 Copyright © 2007 Royal College of Physicians. Reproduced from Royal College of Physicians et al. [46], with permission. Algorithm for the assessment of pain in older people.
Transforming Long-Term Care Pain Management in North America Guidelines [28]
Despite advances in the area of pain assessment in dementia as well as guideline development by credible and influential groups, best practices in pain assessment have not been implemented on a large scale basis. As a result, pain problems continue to go undetected [15, 24, 33, 39, 44]; behavioral disturbance due to pain is managed by psychotropic medication [13], which has been shown to hasten death and lead to unnecessary polypharmacy [8, 9, 26]. Given the absence of wide scale implementation, a group of pain and public policy experts addressed the question of wide-scale implementation failure [28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






