Halo-Related Complications
Robert C. Decker
Steven R. Garfin
The halo was initially described in 1959 for cervical immobilization of patients following uninstrumented fusion for poliomyelitis (1). Since then, its indications have been expanded to include patients with inflammatory diseases, neoplasia, infection, trauma, and related postsurgical cervical and cervicothoracic procedures. While the reported motion restriction varies in the literature, the halo does provide the greatest immobilization below C2 possible with external orthoses (2, 3 and 4). Despite the ability of the halo to stabilize the spine and allow early mobilization, its potential complications along with increased utilization of internal fixation have resulted in a decrease in its popularity. This chapter explores how the halo affects the patient, the potential complications of halo use, prevention and management of these complications, and complications in specific patient populations.
COMPLICATIONS
Van Middendorp’s prospective cohort study evaluating the complications of halo use in 239 patients found that 60% of patients treated in a halo had a complication. This agrees with previous reviews that have shown a high overall complication rate with halo use (5, 6, 7 and 8). Overall, there were 26 major, 72 intermediate, and 121 minor complications in Van Middendorp’s study. Major complications were defined as those causing permanent physical impairment or death and included deterioration of neurologic status, acquired permanent neurologic deficits, and thromboembolism. Temporary complications were grouped into intermediate and minor groups. Intermediate complications included pulmonary complications, such as respiratory distress, atelectasis and pneumonia; halo-related complications such as pin penetration through the skull and halo ring loosening; and loss of cervical alignment. Minor complications included temporary neurologic conditions (peripheral nerve paresthesias, nerve root pain, nerve root palsy), delirium, difficulties swallowing, pin loosening, pin site infection, and pressure sores (9).
PIN LOOSENING
Pin loosening is the most common complication, reported in 3.7% to 100% of patients (6,9, 10, 11 and 12). A loose pin has been defined as one that can be freely twisted without resistance or when the tip is visible (6). Kostuik (13) considered a loose pin as one in which the torque applied through the pin is less than 8 inch-pounds. Patients often appreciate loosening as a clicking sensation at the pin-skull interface. Fleming found it was common for many, if not all, pins to become loose due to an average 83% decrease in compressive force at the pin site over time (14). Ventral pins loosen more commonly than dorsal pins. This has also been found to occur in the pediatric population (6,15).
Initially, it was believed that pin loosening was related to pin site infection. Early reports recommended against pin retightening as it was thought to lead to an increased rate of skull penetration and spread of infection (1,12). Garfin et al. (6) found that keeping pins tight decreased the risk of drainage. Additionally, Vertullo et al. demonstrated retightening could decrease the rate of pin site complications. They found a very low rate of pin site infection (1.1%) and loosening (3.7%) when pins were retightened at 24 hours and 1 week after application (12). Additionally, Van Middendorp et al. (9) confirmed that pin loosening was not significantly related to the development of pin site infection.
Currently, it is common practice to retighten pins at 24 hours and again at 1 week after application as this protocol has led to a decreased rate of loosening. Initially, halo pins were tightened to 0.7 Nm (6 inch-pounds) and more recently to 0.9 Nm (8 inch-pounds) to help decrease loosening (10). Botte et al. (5,16) demonstrated that increasing the amount of torque from 0.68 to 0.90 Nm decreases the prevalence of pin loosening from 36% to 7% and reduces the rate of infection from 20% to 2%. Nemeth and Mattingly’s (11) study confirmed this, demonstrating an 8% prevalence of loosening when tightening to 0.90 Nm with a retightening protocol.
The halo ring is important in decreasing pin loosening. A well-fitted ring decreases the lever arm of the pin, which
in turn reduces the moment of torque acting on the pin and the subsequent motion at the pin-bone interface (10). Additionally, the material of the halo ring influences pin force. Pins inserted into graphite rings lose 57% to 71% of their initial strength after tightening the lock nut, while pins placed in metal rings did not demonstrate the same phenomenon (17). Lastly, closed halo rings resulted in greater rigidity as compared to open rings (18).
in turn reduces the moment of torque acting on the pin and the subsequent motion at the pin-bone interface (10). Additionally, the material of the halo ring influences pin force. Pins inserted into graphite rings lose 57% to 71% of their initial strength after tightening the lock nut, while pins placed in metal rings did not demonstrate the same phenomenon (17). Lastly, closed halo rings resulted in greater rigidity as compared to open rings (18).
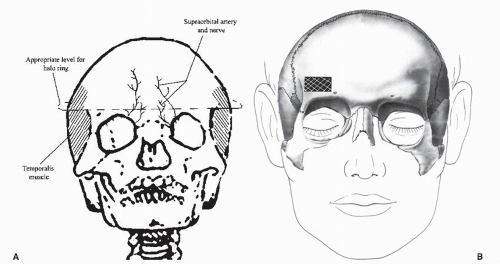
The halo’s ventral pins should be placed within the safe zone defined as 1 cm superior to the orbital rim, over the lateral two-thirds of the orbit, and below the equator of the skull. The safe zone avoids injury to the frontal sinus, supraorbital nerve, and supratrochlear nerve medially. Additionally, it prevents injury to the zygomaticotemporal nerve and the temporalis fossa laterally. Ballock et al. (19) found that pins placed higher resulted in a construct that was less rigid. The ideal pin location was 0.5 cm rostral to the eyebrow. Pins placed 1 to 1.5 cm above were 10% and 30% less rigid. Placement of the pins below the equator engages the skull close to, or at, a 90-degree angle, which is also biomechanically superior (Fig. 107.1).
Nemeth described a six-pin halo construct for adults to decrease the risk of pin loosening. In addition to the standard ventrolateral pins, pins were placed 1 and 2 cm behind each ear. The two extra pins were placed dorsally because of aesthetics, a documented lower rate of loosening compared to ventral pins, and a lower risk of infection. They found the load to failure of the six-pin construct was 171% of the standard four-pin constructs. In a retrospective review of patients treated with six pins, there was a 2.4% prevalence of pin loosening with an infection rate of 1.9% (11) (Fig. 107.2).
Pin design has also been investigated to help decrease the risk of pin loosening. Halo pins are sharp conical points that engage the outer cortical wall of the skull. Current halo and pin designs are unable to adapt to small changes in the geometry of the skull during treatment due to bone remodeling, stress relaxation of the skull, and wear and abrasion of the pin sites. Over time, pins loosen in a time-dependent manner due to the biologic resorptive response of bone under pressure (20). This problem is currently addressed by higher torque initial tightening and retightening (12). Voor and Khalily (21) found that pins with a cylindrical mill tip had greater stiffness than did the conventional conical tip. Additionally, some work has been done with adaptive halos that do not have threaded pins and models that utilize facemasks to provide noninvasive immobilization. These designs are still experimental and have not made their way into clinical use (22). The tradeoff of these noninvasive halo devices may be visual and eating limitations due to the face mask, and the potential for skin pressure problems.
PIN INFECTION
Pin site infection has many presentations ranging from superficial infection to deep abscess. Pin site infections have been described in 1.9% to 22% of patients treated with a halo (1,6,7,10,15,23). Van Middendorp et al. (9) found pin site infection was not related to loosening but was significantly related to penetration through the outer table of the skull.
Botte prospectively studied whether a skin incision prior to pin insertion altered complications as compared to no incision. He found no difference in the amount of infection, loosening, or scarring (24). A Cochrane review of infection rates with different types of cleaning or dressings
around percutaneous pin sites found that there was insufficient evidence for a specific cleaning strategy to minimize infection rates. A prospective, randomized study looking at pin site care in children with external fixators, traction pins, and halos suggested that half-strength peroxide was superior to soap-and-water cleaning (25). Currently, there is no consensus regarding the optimal pin site care technique (26). In our practice, pins are inserted under sterile conditions and then cleaned daily with 1/2 normal saline and 1/2 hydrogen peroxide solution initiated by nursing staff in the hospital and continued in the outpatient setting by the patient.
around percutaneous pin sites found that there was insufficient evidence for a specific cleaning strategy to minimize infection rates. A prospective, randomized study looking at pin site care in children with external fixators, traction pins, and halos suggested that half-strength peroxide was superior to soap-and-water cleaning (25). Currently, there is no consensus regarding the optimal pin site care technique (26). In our practice, pins are inserted under sterile conditions and then cleaned daily with 1/2 normal saline and 1/2 hydrogen peroxide solution initiated by nursing staff in the hospital and continued in the outpatient setting by the patient.
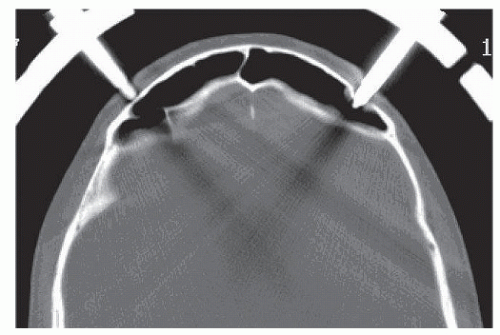 Figure 107.2. Axial head CT demonstrating right ventrolateral halo pin penetration into the frontal sinus. Pin was subsequently removed and placed more laterally with a good result. |
If infection is suspected, it is recommended to start oral antibiotics at the earliest sign. The utility of culture of the drainage is unknown. If pin sites are draining and the pin becomes loose, it is not recommended to retighten the pin (5,6,27). If pins are loose, then they should be removed, the site debrided with cultures obtained, and IV antibiotics started. If possible, a new pin site location should be sought. Deep infection may lead to osteomyelitis or intracranial abscess and need for operative debridement (6,27, 28, 29 and 30).
INTRACRANIAL PENETRATION
Van Middendorp et al. (9) found pin penetration through the outer table of the skull in 5% of patients with no pin penetrations through the inner table of the skull and, therefore, no leakage of cerebrospinal fluid, epidural abscess formation, or meningitis. Outer table penetration was found to be associated with pin loosening. Other studies have found intracranial penetration in 1% to 4% of patients (6,23,27).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree