Figure 79.1. The effects of oxygen deprivation on corticostriatal field potential in Wistar rats. The upper part shows the effects of different periods of hypoxia on the field potential amplitude. In all of the experiments, hypoxia was initiated at time 0 and lasted 10, 20, 30 or 40 minutes. At the bottom, A, B, C and D represent the field experiments showing the potential amplitude before (a), in (b) and after (c), in different periods of hypoxia. Calibrations in D also apply to A, B and C.
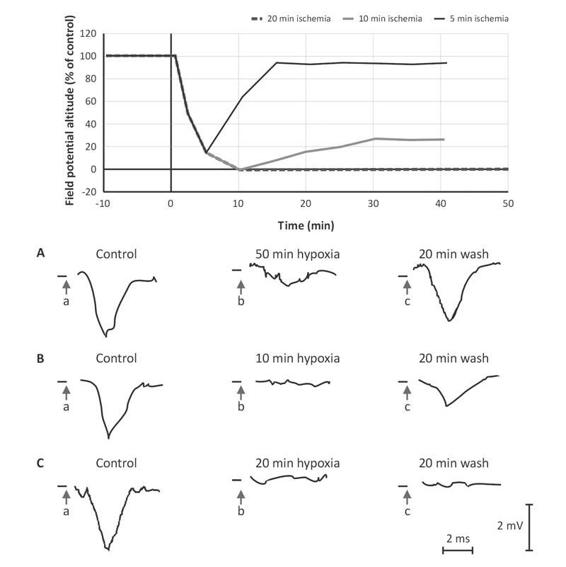
Figure 79.2. The effects of ischemia on corticostriatal field potentials of the brains of Wistar rats. The upper part shows the effects of different ischemia periods on the field potential amplitude. In all of the experiments, ischemia started at time 0 and lasted 5, 10 or 20 minutes. At the bottom, A, B and C represent experiments showing the potential amplitude before (a), in (b) and after (c), from different ischemia periods. Calibrations in C also apply to A and B [15].
79.11 The Electroencephalogram
This simple method is available in most centres and has high sensitivity. It has even been used as a form of continuous monitoring in patients with HIE. It must be taken into account that its interpretation can be affected by pharmacological action, particularly benzodiazepines and barbiturates.
There is some consensus that some patterns show poor prognosis: suppression paroxysm, presence of periodic discharges and electrical silence. In 1990, an electroencephalographic (EEG) grading scale was created which was applied 24 hours after successful cardiopulmonary resuscitation, yielding prognostic values with 98.4% veracity; since then, several studies have attempted to verify these findings. The scale assigns 5 grades, where grades 1 and 2 are predictors of full recovery, and grades 4 and 5 denote a poor neurological prognosis (Table 79.1).
Grade I | Dominant alpha rhythm with some theta-delta activity, reactive |
Grade II | Theta-delta activity with some normal alpha activity, reactive |
Grade III | Predominantly theta-delta activity without normal alpha activity |
Grade IV | Low voltage delta activity, not reactive Alpha coma (generalized non-reactive alpha activity) Paroxysm-suppression pattern |
Grade V | Isoelectric |
Table 79.1. EEG grades in patients with HIE.
79.12 Neurobiochemical Markers
The difficulty in establishing a clinical prognosis has led to research into finding biochemical markers that have a close correlation with neurological prognosis.
79.12.1 Creatine Kinase Isoenzyme BB in Cerebrospinal Fluid
The brain is rich in creatine kinases and its BB enzyme, and it does not have types MM and MB. For this reason, CKBB activity is not affected by extracerebral factors. At experimental levels a good correlation has been shown between the elevation of this enzyme and the degree of neurological damage. The peak elevation occurs within the first 48 to 72 hours after cardiac arrest, has a sensitivity of 82% and a specificity of 85%, and a positive predictive value for persistent vegetative state of 0.96 when levels reach or exceed 50 UI/l, reaching a specificity of 100% with cut-off values of 205 IU/l.
79.12.2 Serum Neuron-specific Enolase
Levels reflect structural brain damage; values of 33 ng/ml predict persistent coma or brain death with a specificity of 100% and a sensitivity of 80%. However, one limitation is that there is no temporal correlation known to confirm a prediction.
79.12.3 Serum Astroglial S100 Protein
Just like neuronal enolase, S100 protein reflects structural brain damage. Values ≥0.2 ng/ml from the second day on have a positive predictive value of 100% for mortality, while values <0.2 ng/ml within the first 14 days show a survival prognosis of 89%. When the evaluation is conducted immediately after the event, S100 protein values are significantly higher in patients with persistent brain damage than in those who recover without neurological sequelae.
A systematic review of the usefulness of biochemical markers as predictors was published in 2001, which concluded that although the CKBB results were interesting, there were methodological flaws and an inadequate number of patients; therefore, they are insufficient as isolated prognosis guides.
79.13 Images
During the first 24 hours, the brain computed tomography (CT) scan lacks sensitivity, so a slight or moderate alteration can pass unnoticed, while if there is evidence of injury, the damage is significant. The most common early finding is the disappearance of grooves caused by cerebral edema. After 48 hours, hypodense lesions in the cerebral cortex, cerebellum and basal ganglia appear evident on the image. Bordering infarcts and brain atrophy are evident in the following days.
Magnetic resonance imaging (MRI) is more sensitive for detecting infarctions and cerebral edema, above all with the diffusion technique, which can appreciate gray matter alterations during the acute period, alterations in the white matter during the subacute period, and return to normal during the chronic phase. From the second week on, in T1, T2 and fluid-attenuated inversion recovery (FLAIR) sequences there appear hyperintense cortical lesions, which represent cortical laminar necrosis.
As for other techniques, such as MR spectroscopy and single-photon emission computed tomography (SPECT), some interesting data have been presented, but their diagnostic and prognostic values are still under study.
79.14 Therapeutics
Successful resuscitation of a patient from a sudden death event is only the beginning of a therapeutic process which under the best circumstances will return the patient to daily activity with total self-sufficiency. However, the figures derived from several studies are not as encouraging in these results; they indicate that barely 20% of patients return to absolute self-sufficiency without residual or minimal deficit.
Some 80% of survivors end up with a result that can vary from partial to total dependence, with the consequent family and social costs.
Managing a patient after a sudden death episode is therefore extremely complex, and all information that can be obtained is critical, both for immediate management as well as subsequent therapeutic decisions. In this sense, it is very important to know the levels of self-sufficiency prior to the event, the associated co-morbidity that can have a triggering or aggravating effect, and the perspective from the social and family environment.
A few years ago, treatment of patients suffering from cardiorespiratory arrest was based on cardiovascular resuscitation and general medical treatment. The absence of specific therapies marked an uncertain, and usually poor neurological prognosis, the majority evolving to total dependency, persistent vegetative state or death [8].
In recent years, different measures have been questioned in the treatment of HIE, most of which supported by pathophysiological reasoning, as several studies have failed to demonstrate significant differences in their use in clinical practice. However, the use of induced hypothermia has shown promising results.
Currently, we have measures directed at counteracting different points in the chain of injury. Among general neurological protection measures are ensuring CBF by maintaining normal or moderately high blood pressure, providing adequate oxygen supply to reach a PO2 of 100 mmHg, and trying mild hyperventilation, 30 to 35 mmHg.
In an injured brain, it is necessary to prevent further damage that could worsen its condition; as we have seen, hypoxia and ischemia bring about greater fragility and predisposition to injury from other causes. Under these conditions, considering that 30% of patients have seizures, the prophylactic use of anticonvulsants is recommended. Achieving metabolic stability, with internal environmental balance and no imbalances in either glucose or intra- and extracellular components, is one of the primary objectives. Within these, there is a special attention to calcium, since as we have seen it plays a significant role in many neuronal injury processes.
79.14.1 Calcium Antagonists
Numerous studies have failed to demonstrate the usefulness of calcium in ischemic encephalopathy, despite having a pathophysiological basis that supposes a beneficial effect. More than 30 studies that included oral and intravenous calcium antagonists were analyzed, many of which were excluded due to methodological flaws, and none showed a clear benefit. It is worth noting that a statistically significant difference was found in one study, where a subgroup that received nimodipine within the first 12 hours of the event was analyzed. This suggests that failure to prove utility is probably due to administration subsequent to establishment of the injury [9].
79.14.2 Hypothermia
Around 40% of patients survive cardiorespiratory arrest in the extra-hospital environment, but it is estimated that near 20% of these will have limiting neurological damage. Hypothermia has been used as a therapeutic method with good results; however, the exact mechanism by which it acts on HIE is not known. Many mechanisms have been proposed, including reduction of released mediators during hypoxia, delayed production of enzyme products and free radicals, protection of lipid membranes, decreased metabolism and cerebral oxygen demand, reduced intracellular acidosis, reduced intracranial pressure, and protection of ongoing ischemia. Early work on the use of hypothermia began in 1950 when it was used in cardiac surgery. In the 1990s its use was intensified in experimental animal models, and most recently it has been used in human studies in an attempt to find its application in different, mostly neurological, pathologies.
Canine models showed a lower incidence of neurological deterioration after the application of hypothermia, and interestingly, an increase in tolerance to global ischemia, which increases as temperature decreases. For example, if the temperature is reduced from 37°C to 25°C, the time without damage lasts 5 times longer [10].
In humans, two prospective, multicenter, randomized controlled studies have been performed to date; the first was done by a European group and included 273 patients who suffered extra-hospital cardiac arrest, 136 of which were treated with hypothermia between 32° and 34°C for 24 hours, while in 137 normothermia was maintained. After 6 months, the neurological outcome in 55% of patients in the hypothermia group was good, with independence and re-insertion to work, at least part time, as compared with 39% of patients in the control group. (RR 1.4, 1.08-1.81); the number needed to treat (NNT) was 6 (95% CI 4-25]. The mortality at 6 months was 41% in the treated group and 55% in the control group (RR 0.74, 0.58-0.95); the NNT was 7 (95% CI, 4-33). There was no difference in medical complications between the groups [11].
The second study was done in Australia and included 77 patients resuscitated from an extra-hospital cardiac arrest; 43 were treated with hypothermia at 33°C for 12 hours and in 34 normothermia was maintained. At discharge, 49% of the patients treated with hypothermia had a good neurological state, being discharged to their homes or a rehabilitation centre, while in the normothermia group, only 26% achieved this goal (p=0.046). There was no statistical difference in terms of mortality (51% in hypothermia and 68% in normothermia). There were also no significant medical complications reported in the group treated with hypothermia [12].
It must be noted that in both studies, there is a duality in the result of hypothermia application, since almost all treated patients either die (41% and 51%, respectively) or end up without severe neurological damage (55% and 49%, respectively).
In a meta-analysis by Holzer et al., it was found that hypothermia at 33°C applied to resuscitated patients with extra-hospital cardiac arrest statistically increased the possibility of patients with a favourable neurological recovery at discharge (OR 1.68, 1.29-2.07), with an NNT between 4 and 13 [13].
Since 2003, with these data, the International Liaison Committee on Resuscitation (ILCOR) has incorporated moderate hypothermia at 32-34°C for 12 to 24 hours as a recommendation for patients who have been resuscitated from extra-hospital cardiac arrest [14].
Figure 79.3 shows a patient with HIE secondary to a sudden cardiac death episode under moderate intravascular hypothermia, while Figure 79.4 summarizes the flowchart for resuscitated sudden death event.

Figure 79.3. Patient with HIE secondary to a sudden cardiac death episode under moderate intravascular hypothermia. The monitor to the right displays a temperature of 33.1°C.
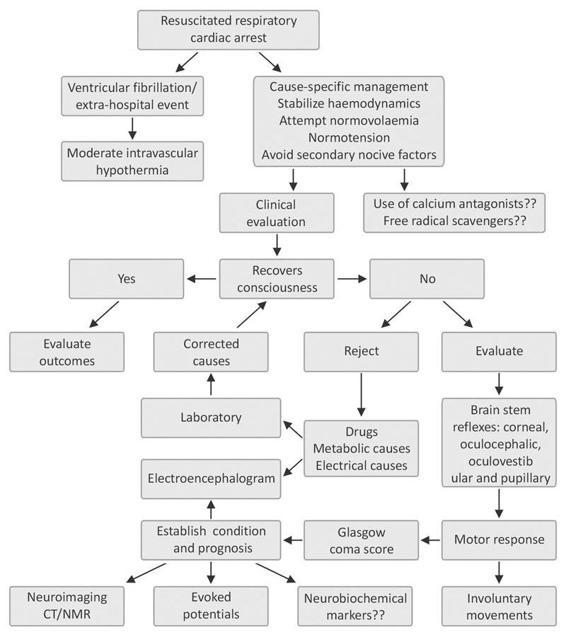
Figure 79.4. Flowchart for resuscitated sudden death event, with an emphasis on addressing hypoxic ischemic encephalopathy.
References
1. Young B. Anoxic and ischemic brain injury. In: Young B, Ropper A, Bolton CH (eds). Coma and impaired consciousness. McGraw-Hill: New York, 1998; pp. 409-56
2. Seta K, Yuan Y, Spicer Z, et al. The role of calcium in hypoxia-induced signal transduction and gene expression. Cell Calcium 2004; 36: 331-40
3. Vaagenes P, Ginsberg M, Ebmeyer U, et al, Cerebral resuscitation from cardiac arrest: pathophysiologic mechanisms. Crit Care Med 1996; 24(2 Suppl): S57-68
4. Anatoly A, Starkov A, Christos Chinopoulos B, et al. Mitochondrial calcium and oxidative stress as mediators of ischemic brain injury. Cell Calcium 2004; 36: 257-64
5. Maiese K, Caronna J. Coma after cardiac arrest: clinical features, prognosis, and management. In: Ropper A. (Ed). Neurological and neurosurgical intensive care. New York: Raven Press, 1993; pp. 331-49
6. Wijdicks EFM. Neurologic complications of cardiac arrest. In: Wijdicks EFM. (Ed). Neurologic complications of critical illness. Oxford: Oxford University Press, 2002; 123-42
7. Maramattom BV, Wijdicks EFM. Postresuscitation Encephalopathy: Current Views, Management, and Prognostication. The Neurologist 2005; 11: 234-43
8. Horn J, Limburg M. Calcium antagonists for ischemic stroke a systematic review. Stroke 2001; 32: 570-6
9. Ginsberg MD, Belayev L. The effects of hypothermia and hyperthermia in global cerebral ischemia. In: Maier CM, Steinberg GK (eds). Hypothermia and cerebral ischemia: Mechanisms and clinical applications. Totowa: Humana Press, 2004; pp. 17-38
10. Ginsberg M, Belayev L. Hypothermia and cerebral ischemia: Mechanisms and clinical applications. Totowa: Humana Press, 2004; pp. 17-38
11. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002; 346: 549-56
12. Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002; 346: 557-63
13. Holzer M, Berbard SA, Hachimi-Idrissi S, et al. Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta-analysis. Crit Care Med 2005; 33: 414-8
14. Nolan JP, Morley PT, Vanden Hoek TL, et al. Therapeutic hypothermia after cardiac arrest: an advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation. Circulation 2003; 108: 118-21
15. Pedersen JZ, Bernardi G, Centonze D, et al. Hypoglycemia, hypoxia, and ischemia in a corticostriatal slice preparation: electrophysiologic changes and ascorbyl radical formation. J Cereb Blood Flow Metab 1998; 18: 868-75
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






