14
CHAPTER
![]()
ICU Continuous EEG Monitoring
Keith E. Dombrowski
The advent of digital video EEG (vEEG) recording has created unique opportunities in the hospital, particularly in the intensive care unit (ICU). Prolonged or continuous EEG (cEEG) monitoring refers to the continuous recording of digital EEG for hours, days, or weeks at a time. cEEG with simultaneous video recording are performed for various reasons but most frequently for seizure monitoring. In the past decade, the role of cEEG monitoring in the ICU has and continues to expand rapidly. Much of this growth has come from the recognition of the high prevalence of nonconvulsive seizures (NCS) and nonconvulsive status epilepticus (NCSE) in the ICU and growth of neurocritical care services Neuro Intensive Care Unit (NeuroICU) in general. NCS are defined as electrographical seizure activity in the absence of a clear clinical correlate. Status epilepticus has been defined as the presence of frequent NCS, usually occupying more than 30 minutes in an hour of the recording. NCS and NCSE in the ICU were recognized but underappreciated events until late. cEEG is also uniquely suited as a monitor of brain dysfunction in general, particularly abnormal cerebral metabolism. cEEG monitoring is a very sensitive detector of cerebral ischemia and hypoxia, particularly when it is potentially reversible and when clinical examination of the patient is unhelpful or is not possible. cEEG monitoring is suited to the dynamic ICU environment where brain injury can evolve or change quickly. Due to this rapid growth in cEEG monitoring, much more is known about the utility of “ICU EEG,” particularly with respect to patient selection and the type and duration of monitoring. However, cEEG monitoring offers many challenges. Clinically, cEEG monitoring in the ICU has presented epileptologists with unique electrographic patterns that can often be difficult to interpret. Logistically, a cEEG monitoring service can be difficult to maintain due to financial, personnel, and technological constraints. However, the future of cEEG monitoring is rapidly becoming a reality with 24/7 availability in most academic centers and real-time interpretation services with some using cutting-edge trending software.
cEEG MONITORING SERVICE
There are numerous factors to consider when starting or managing a cEEG monitoring service. Digital vEEG has made recording and reviewing hours or days of EEG monitoring possible through high-quality acquisition platforms, efficient data storage, and network accessibility. In the past decade, digital EEG acquisition with a broad dynamic range, excellent noise reduction technology, and high sampling can be easily acquired and reviewed on flexible platforms with intuitive user interfaces. High-definition cameras are routinely used for recording and providing detailed images synchronized with the EEG. The availability of mobile technologies leveraging broadband networks and large-volume digital data storage has made storage and remote review of large amounts of EEG possible. Ever-improving hospital telecommunications and information technology services have been essential in initiating and maintaining such services. Though such services are currently limited to large academic institutions, the price of technology goes down over time and the cost of starting and maintaining such services will become less onerous in the future. Essential components to an effective cEEG monitoring service include a fleet of portable or fixed digital vEEG acquisition systems, a robust network with on-call IT support, and effective data storage and management systems.
Some recent advances in electrode technology have made cEEG monitoring easier to perform and more versatile than in years past. Though reusable gold-plated electrodes remain the norm for many neurophysiology labs, silver–silver/chloride-coated plastic electrodes are more versatile and can reduce the cost of ICU EEG monitoring services (personal communication). Because many patients receiving EEG monitoring have brain injury, the likelihood of needing neuroimaging during a prolonged EEG study is relatively high. Plastic electrodes can significantly reduce the amount artifact seen on CT scans compared to gold-plated electrodes (Figure 14.1). Some electrodes are even employed when obtaining MRI scans as well. This reduces the time and cost of removing and reapplying gold electrodes and will likely improve work flow for a busy clinical service. Needle electrodes were commonly used in ICU and neonatal settings prior to the HIV epidemic. With improvements in needle safety and the availability of disposable needle electrodes, there has been resurgence in their use. Needle electrodes can allow for long-term recordings that provide high-quality data with less maintenance than that of glued cup electrodes. They may also be applied faster than glued cup electrodes, further improving workflow. Though infection and bleeding are a concern, there has been no data to indicate that even long-term needle placement results in a significant risk of infection or injury from placement. As with plastic cup electrodes, needle electrodes can be CT and MRI compatible.

FIGURE 14.1 Plastic cup electrodes in CT.
![]()
An equal, if not more important, factor to consider is that of staffing, specifically technologists and interpreting personnel. An effective cEEG monitoring service requires 24-hour staffing either with in-house or on-call technologists. Due to the rigors necessary for proper, technically adequate EEG acquisition, registered technologists should be employed whenever possible. The ICU is an electrically hostile environment replete with artifact. Proper EEG electrode placement is necessary to reduce preventable artifacts as well as assist in localization of seizures and other evolving cerebral pathology. Interpreting personnel typically consist of neurophysiologists or specially trained technologists. In most institutions, cEEG monitoring for seizures consists of continuous recording with intermittent review of the data at various intervals. Unless there is in-house coverage or sufficient networking capabilities, on-demand cEEG review requires 24-hour on-call services and a physical presence in the hospital to review the data. Maintaining a sufficiently large workforce to start and interpret EEG studies is a difficult task for most institutions.
Technological and personnel requirements represent only two hurdles to overcome when operating a cEEG monitoring service. The other significant factor is cost. From one institution, the annual yearly cost of maintaining a busy cEEG monitoring service in 2011 (1500 patient days/year) was estimated at nearly $460,000, with most of that cost being derived from personnel salaries (personal communication). Cost-effectiveness studies of pharmaceuticals and medical services are becoming increasingly common in the United States and must be considered when determining the true cost benefit of a procedure. Therefore, total cost of a cEEG monitoring service must also consider the hospital charge to the patient and their insurance carrier. Though cEEG monitoring is an expensive service, there appears to be a favorable cost–benefit. One study looked at the outcome of patients with traumatic brain injury and found an improvement in outcome for the patients as well as a significant reduction in length of stay and total cost for hospitalization (1). There are likely other, unmeasurable benefits gained from cEEG monitoring, including discontinuation or reduction in medication and changes in clinical decision making obtained as a result of EEG monitoring. Presently, there are cost-reduction strategies being used throughout the United States to reduce the cost and burden of EEG monitoring as well as improve the accessibility of such services. Such strategies include disposable, nontechnician applied electrode templates or limited electrode arrays for emergency EEG studies. However, further cost-effectiveness studies will be required as cEEG monitoring becomes more commonly employed.
RECORDING EEG IN THE ICU
The ICU is a very unique environment for recording EEG. There are few places in the hospital where more monitors and equipment are accommodated into a single room. If cEEG monitoring equipment is not “hard-wired,” a portable acquisition system must then be placed in the room as well. Electrical safety of the patient is of supreme importance and ICU rooms are well designed and rigorously tested to ensure that each new piece of equipment can be safely used. However, many other hazards to cEEG monitoring exist. Without adequate training, a study can be disrupted or interrupted by inexperienced staff that may disconnect a network cable, headbox, or video equipment. ICU staff must be properly educated before the introduction of cEEG monitoring in order to reduce the chances of study disruption. Even experienced nurses are significantly challenged when a patient is placed on cEEG monitoring. They must contend with a large bundle of electrodes, which can become wrapped around IV tubing, bedrails, or other monitoring cables. Without effective management of the hardware, it is easy to accidentally remove even well-secured electrodes. The duration of a cEEG monitoring study also makes degradation of the quality of recording more likely as electrodes may fall or be pulled off in the middle of the night when quick repair is least likely. Transport of a patient on cEEG monitoring is particularly challenging as all cables and wires typically travel with the patient unless they are removed beforehand. Emergent neuroimaging or travel to an operating room may often need to be accomplished with all of the electrodes in place. Most ICUs are supplied with acetone or other solvents. However, in circumstances where the study shouldn’t be interrupted, the staff must carefully secure all of the equipment in the bed before transport. Wireless amplifiers may reduce these issues in the future, but these devices are not available in many institutions.
The ICU is also electrically hostile, making unusual artifacts common occurrences. It is essential to know the environment in which the patient is being monitored. Unique artifacts seen during recording include those derived from the ventilator cycling, suctioning, IV drip pumps, bed percussion/vibration modules, dialysis, and aortic balloon pumps/ventricular assistance devices (Figure 14.2). Nursing interventions such as suctioning, chest percussion, and manipulation of the wires are a significant source of artifactual signal. Digital EEG recording offers advantages in mitigating these aberrant signals. Manipulation of montages and filters can assist in eliminating or reducing the impact of environmental and patient-derived artifacts. Most cEEG monitoring machines are equipped with a mechanism to mark or provide notes directly onto the digital record. Annotation of the record by the nursing staff and technologist is very helpful in distinguishing artifact from cerebral signals. Annotations serve an equally useful function of marking when drugs are administered or when movements of interest are noted. As with other forms of prolonged EEG monitoring, the value of simultaneously recorded video cannot be overstated.
The patient population is as unique as the ICU environment. As many patients requiring cEEG monitoring have significant head or brain injury, technologists must carefully position electrodes to avoid contaminating an open wound or operative site. In many cases, individual electrodes must be displaced or removed altogether. Intracranial anatomy is often shifted due to cerebral edema and intracranial fluid collections, making localization of seizures more challenging. Electrical dipoles may have an aberrant appearance or polarity due to intracerebral hemorrhage or postoperative fluid collections. Head injury often results in significant scalp edema, which can produce attenuation of the EEG signal on the side of the injury. Skulls defects are frequent, making breach rhythms common. Though needles are less frequently used for recording EEG, they present particular difficulty in patients with large skull defects such as craniectomies. Special consideration should also be given when applying needles in patients with coagulopathies. Patient-generated artifacts are numerous and more common in the ICU, including myoclonic jerking, shivering, asymmetric eye movements, and nystagmus. Knowledge of the patient’s admitting diagnosis, skulls defects, and intracranial devices is essential in accurately interpreting the record. It is common for frontal electrodes (F3 and F4) to be missing as a result of an external ventricular drain or other intracranial pressure monitors placed on the skull. In many cases, review of the patient’s neuroimaging in conjunction with the EEG can significantly increase the diagnostic yield of the study.
INDICATIONS
The most common reason for performing a cEEG study in the ICU is for detection of subclinical or nonconvulsive seizures (NCS) in a patient with significant alteration in consciousness. In many cases, cEEG monitoring is initiated after known or suspected clinical status epilepticus. The likelihood of developing subclinical seizures or status epilepticus after GCSE can be over 30% (2). Refractory status epilepticus requires cEEG monitoring for suppression of electrographical seizures. After several important publications, the prevalence of de novo NCS (15%–30%) and NCSE (10%–15%) in the ICU is clearly much higher than previously thought (3,4). cEEG monitoring is the only effective method for detecting these types of seizures and therefore uniquely suited to this job. Early application of cEEG monitoring in the brain injured is critical in identifying and treating NCS and NCSE as seizures become more difficult to treat over time (5). The diagnosis and treatment of NCS and NCSE may be critical in avoiding adverse patient outcomes in certain populations. Though seizure detection is probably the most important question that can be answered, encephalopathic patterns with or without epileptiform abnormalities can provide very useful information. The spectrum of encephalopathic patterns, namely mild–moderate theta slowing, marked and severe delta slowing, suppression, and burst suppression patterns can provide helpful diagnostic and prognostic information for many patients with septic encephalopathy, drug intoxication, and cardiac arrest (CA). In those with suspected but undiagnosed neurological disease, findings of focal slowing and epileptiform abnormalities can provide diagnostic guidance (ie, bilateral independent periodic discharges [BiPDs] in suspected infection, lateralized periodic discharges [LPDs] in those patients with seizures and a leukocytosis). This information can be important for guiding other diagnostic testing.
cEEG monitoring is not limited to the detection of NCS and NCSE and has proven critical in ICU spell characterization. Similar to studies performed outside the ICU, characterization of paroxysmal events is a common use for cEEG monitoring. Stereotyped motor movements presumed to represent seizures are a frequent reason for the request of an EEG or for cEEG monitoring in the ICU. Many such movements are seen and include intermittent posturing from herniation, clonus, and tremor. Other more benign movements that are confused with seizure include coughing while on a ventilator as well as stereotyped movements during arousal or emergence from anesthetic agents. In rare circumstances, cEEG monitoring may be necessary to diagnose presumed psychogenic status epilepticus in the emergency room or ICU. Though many stereotyped movements do not represent seizure activity, some very focal seizures may not manifest with a scalp EEG correlate. In other cases, an ictal EEG correlate is obscured by myogenic or movement artifact. Video recording is essential in these scenarios. Alternatively, brief neuromuscular blockade can suppress muscle artifact in order to better visualize cerebral activity that underlies the behavior. This is sometimes necessary in those with frequent myoclonic activity where it is too difficult to differentiate epileptic activity from artifactual signal.
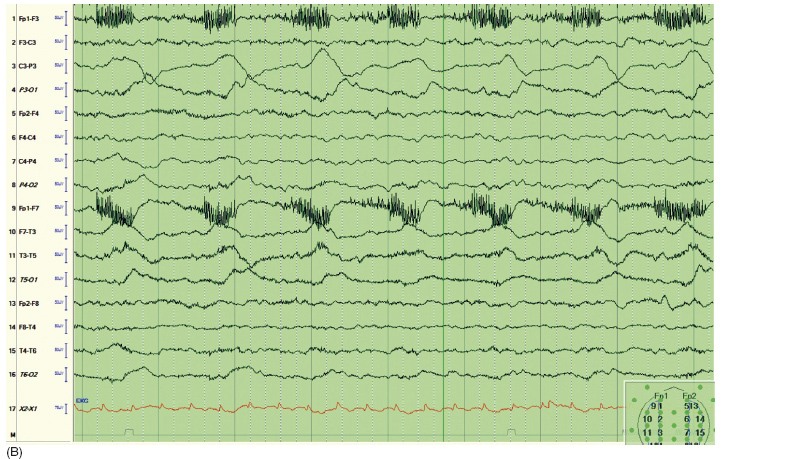
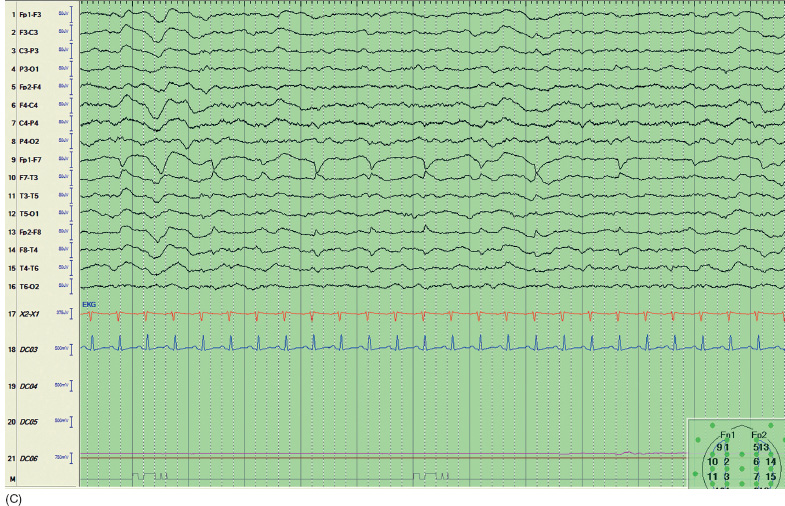
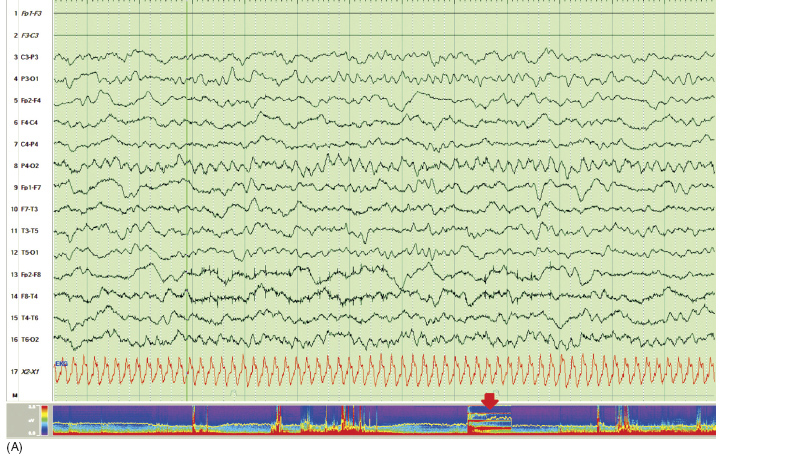
FIGURE 14.2 Examples of artifact in the ICU. (A) Artifact introduced by bed percussion module. The arrow indicates the appearance of this artifact on a compressed spectral array. (B) Artifact introduced by tachypnea on a ventilator. (C) Nystagmus mimicking epileptic discharges in a sedated patient.
![]()
cEEG monitoring is commonly used to measure the depth of anesthesia, whether it is for suppression of seizures or titration to a level of burst suppression sufficient to control intracranial pressure. Though bispectral index (BIS) is frequently used in the operating room, there is limited evidence for its use in those with brain injury. In patients with refractory status epilepticus, cEEG monitoring is used not simply to monitor for the occurrence of seizure but is also often used to make dose adjustments to midazolam or pentobarbital infusions for burst suppression or complete suppression. Another common indication for dose titration to burst suppression is treating refractory intracranial hypertension. Given the dose-dependent side effects seen with most anesthetics, especially propofol and pentobarbital, complete suppression of EEG activity is often not beneficial if the goal of controlling intracranial pressure has been achieved. In many institutions, pentobarbital remains the agent of choice for controlling refractory intracranial hypertension. As serum levels do not correlate well with either effectiveness or toxicity, cEEG monitoring is required to titrate the effective dose of pentobarbital to obtain burst suppression. Reducing EEG activity to that of burst suppression correlates well with maximal reduction in cerebral metabolic oxygen demand (CMRO2). Avoidance of electrocerebral inactivity (ECI) may reduce the possibility of causing further cardiac suppression. Further dose limiting of barbiturates may decrease the possibility of causing other harmful side effects seen in the ICU, including a gastrointestinal ileus and hypothermia. Though some evidence has suggested that BIS measurement may be useful in these cases, the standard of care in most institutions remains cEEG monitoring (6).
Routine EEG has been used for several decades as a prognostication tool, particularly after CA. cEEG monitoring is becoming useful for this purpose as well. Though there is no evidence as of yet to suggest that cEEG monitoring would necessarily be more helpful than a routine study for prognostication, consistent and compelling information has been gained from cEEG monitoring. In most patient populations studied, a lack of EEG reactivity in the absence of heavy sedation is consistently associated with a poor prognosis. The evidence for this is best documented in comatose post-CA patients, but it is present in those with TBI and SAH as well. Given the desire for long-term prognostication in comatose CA patients, this form of brain injury has been best studied. Burst suppression patterns with or without therapeutic hypothermia (TH) are associated with a poor outcome, whereas a continuous reactive record is associated with a good outcome (7). Given that TH is now the standard of care and cEEG monitoring is often performed, more prognostic information will likely be available in the future. cEEG monitoring has been useful for prognosis in other conditions including sepsis where the appearance of LPDs is associated with a poor outcome (8). Other forms of EEG abnormalities in sepsis are also associated with a poor outcome, including suppression and triphasic waves (TW, now referred to as PDs with triphasic morphology). When quantitative trending software is used to analyze a patient’s EEG, decreased alpha variability and an increase in delta power is associated with poor outcome in TBI and SAH patients. A decrease in the alpha:delta ratio and an increase in the brain asymmetry index is associated with worse outcome in acute ischemic stroke (7).
A more recent and novel use for cEEG is as a neuromonitor to detect cerebral ischemia alone or as a component of multimodal neuromonitoring. With developments in quantitative EEG trending tools, cEEG monitoring can be an extremely sensitive real-time detector for cerebral ischemia and other forms of acute brain injury, particularly in those patients where the clinical examination is unhelpful. Either alone or in combination with brain tissue oxygen monitors or cerebral microdialysis catheters, cEEG monitoring can provide data on the development or worsening slowing or suppression suggestive of developing ischemia. This is possible through advanced quantitative EEG software packages that trend data in real time. This is an exciting development for cEEG, but this form of monitoring is available in few institutions and requires significant logistical support to be performed reliably and consistently.
An essential part of maintaining a clinical cEEG monitoring service is the development of guidelines or a protocol to foster proper utilization of this service. A truncated example is provided in Table 14.1.